How to fill out a Medicare ABN form?
Proper ABN Completion
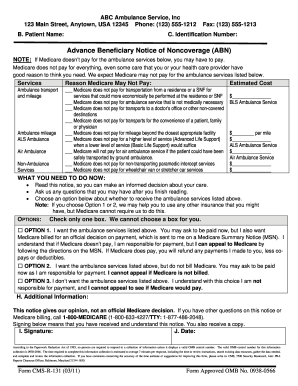
- Patient’s name, specific service and estimated charge amount must be listed on the ABN.
- The ABN cannot be given to a patient who is under duress or requires emergency treatment.
- Check for specific the criteria and download the form: http://www.cms.gov/BNI/02_ABN.asp
When should a Medicare ABN be given?
- What providers use an ABN form? ...
- Are blanket ABN forms legal? ...
- Are blanket ABN forms legal? ...
- When would you use an ABN? ...
- Is ABN only for Medicare? ...
- What is ABN form for Medicare? ...
- When would you use an ABN? ...
- What is an ABN form used for? ...
- Are ABN forms only for Medicare? ...
- Can ABN be used for Medicaid? ...
What if a patient refuses an ABN form?
You must choose one of these options:
- Option 1: You want the items or services that may not be paid for by Medicare. ...
- Option 2: You want the items or services that may not be paid for by Medicare, but you don’t want your provider or supplier to bill Medicare. ...
- Option 3: You don’t want the items or services that may not be paid for by Medicare, and you aren’t responsible for any payments. ...
Do Medicare replacement plans require an ABN?
my understanding of the ABNs is exactly what you put if it is a service that is covered under certain circumstances but probably not for what you are doing it for, you get the ABN. Replacements follow Medicare regulations, so I would think the same services you would get them for Medicare you would get them for the replacements, but it is always best to check the payor.

What is a Medicare ABN and why is it important?
An ABN notifies Medicare that the patient acknowledges that certain procedures were provided. It also gives the patient the opportunity to accept or refuse the item or service and protects the patient from unexpected financial liability if Medicare denies payment.
What is an ABN for Medicare?
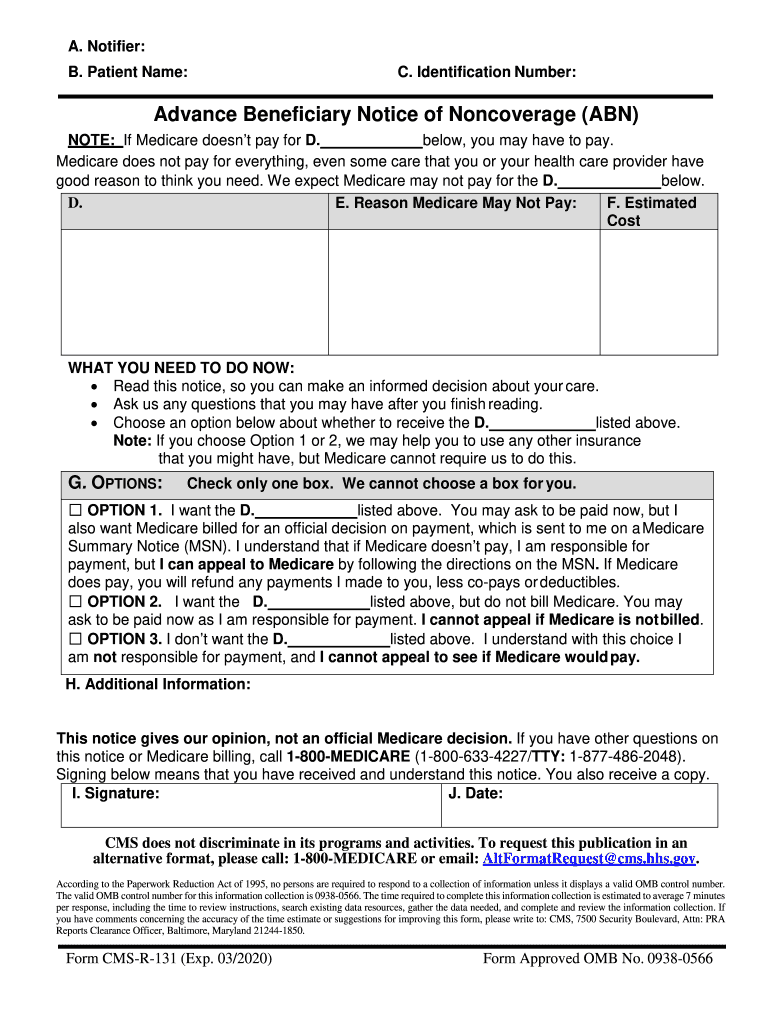
This notice is called an “Advance Beneficiary Notice of Noncoverage” (ABN). The ABN lists the items or services that Medicare isn't expected to pay for, along with an estimate of the costs for the items and services and the reasons why Medicare may not pay.
Is an ABN form only for Medicare?
The ABN, or Advance Beneficiary Notice, is a form that is intended for only for Medicare beneficiaries – not Medicare advantage plans or Medicare part C, just true Medicare.
Who uses ABN form Medicare A or B?
Medicare Advantage is offered by commercial insurance carriers, who receive compensation from the federal government, to provide all Part A and B benefits to enrollees. Therefore, an ABN is used for services rendered to Original Medicare FFS (Part A and Part B) enrollees.
Why is ABN required?
An Australian business number (ABN) makes it easier to keep track of business transactions for tax purposes. It is compulsory for businesses with a GST turnover of $75,000 or more to have an ABN and to be registered for GST.
When must a patient have an ABN?
An ABN is required when an item or service is expected to be denied. This may occur at any one of three points during a course of treatment which are initiation, reduction and termination, also known as "triggering events."
When should an ABN not be issued?
If the provider does not have a reasonable belief that the service or item that is normally payable will be denied than an ABN is prohibited from being issued. Other circumstances were you are prohibited from issuing an ABN include: To make a beneficiary liable for Medically Unlikely Edit (MUE) denials.
How long is a Medicare ABN good for?
one yearAn ABN can remain effective for up to one year. The ABN must describe an extended or repetitive course of noncovered treatment as well as a list of all items and services believed to be non-covered. If applicable, the ABN must also specify the duration of the period of treatment.
Is an ABN free?
It is free to apply for an ABN. However, if you use a tax practitioner or another service provider to complete your application for you they may charge a fee for their services. It's important to choose a registered tax agent or BAS agent.
Who receives an ABN form?
The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, is issued by providers (including independent laboratories, home health agencies, and hospices), physicians, practitioners, and suppliers to Original Medicare (fee for service - FFS) beneficiaries in situations where Medicare payment is expected to be ...
What does an ABN include?
Every ABN requires specific information, including:Your full name.The name, address, and phone number of the provider issuing the ABN.The name of the service or item that might not be covered.The reason Medicare may not pay.Estimated cost.
Is an ABN required if Medicare is secondary?
The ABN needs to be on file for the year that the patient is responsible for paying. If the patient fits Medicare's guidelines for “high risk” they are allowed to have the pap every 12 months and no ABN is required.
What Is A Medicare Waiver/Advance Beneficiary Notice (ABN)?
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying y...
If I Receive An ABN Form, What Are My Options?
You have the option to receive the items or services or to refuse them. In either case, you should choose one option on the form by checking the bo...
What If I Refuse to Sign An ABN, but I Want The Items Or Services Anyway?
If you refuse to sign, one of two actions will take place: 1. Mayo Clinic may decide not to provide the items or services. 2. A second person will...
When I Am Liable For Payment Because I Signed An ABN, How Much Can I Be charged?
When you sign an ABN and become liable for payment, you will have to pay for the item or service yourself, either out of pocket or by some other in...
Why Do I Routinely Receive An ABN For Certain Items Or Services?
Certain items or services that are covered by Medicare are only covered up to a certain number of times within a specified amount of time. Examples...
Do Abns Mean That Medicare Is Reducing Coverage?
No. ABNs do not operate to reduce coverage at all. Only if and when Medicare does deny the claim, do you become liable for paying personally for th...
Who Do I Contact If I Have More Questions About My Medicare Coverage?
For more information about your Medicare coverage, please contact Medicare directly: 1. Phone: 800-633-4227 (toll-free) 2. Website: www.medicare.go...
What is a Medicare waiver/Advance Beneficiary Notice (ABN)?
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying you :
Why do I routinely receive an ABN for certain items or services?
Examples of these "frequency limited" services include laboratory tests, some preventive screening tests and vaccinations. If you receive an ABN that gives a frequency limit as its reason, it means that Medicare will not pay if you exceed that limit on the service.
When I am liable for payment because I signed an ABN, how much can I be charged?
When you sign an ABN and become liable for payment, you will have to pay for the item or service yourself, either out of pocket or by some other insurance coverage that you may have in addition to Medicare. Medicare fee schedule amounts and balance billing limits do not apply. The amount of the bill is a matter between you and Mayo Clinic. If this is a concern for you, you may want to ask for a cost estimate before you sign the ABN.
What happens if Medicare denies you a claim?
The claim will be sent to Medicare. You may be billed while Medicare is making its decision. If Medicare does pay, you will be refunded any payments that are due to you. If Medicare denies payment, you will be personally responsible for full payment.
Who is responsible for Medicare denies payment?
You will be personally responsible for full payment if Medicare denies payment
Does Medicare apply to Mayo Clinic?
Medicare fee schedule amounts and balance billing limits do not apply. The amount of the bill is a matter between you and Mayo Clinic. If this is a concern for you, you may want to ask for a cost estimate before you sign the ABN.
Do ABNs mean that Medicare is reducing coverage?
No. ABN s do not operate to reduce coverage at all. Only if and when Medicare does deny the claim, do you become liable for paying personally for the service or item. If Medicare decides to pay the claim, you have lost nothing by signing the ABN.
What is an ABN?
The ABN is a formal information collection subject to approval by the Executive Office of Management and Budget (OMB) under the Paperwork Reduction Act of 1995 (PRA). As part of this process, the notice is subject to public comment and re-approval every 3 years. With the latest PRA submission, a change has been made to the ABN. In accordance with Title 18 of the Social Security Act, guidelines for Dual Eligible beneficiaries have been added to the ABN form instructions.
Who completes the signature box on an ABN?
Once the beneficiary reviews and understands the information contained in the ABN, the Signature Box is to be completed by the beneficiary (or representative). This box cannot be completed in advance of the rest of the notice.
What is a Medicare ABN form?
An ABN form is a written notice that Medicare may not, or will not, pay for services or items recommended by your doctor, healthcare provider or supplier. The form includes the items or services that Medicare isn't expected to pay for, the reasons why and an estimate of the costs. An ABN allows you to clearly see your financial liability for the items or services and gives you a chance to determine your options.
What options do Medicare ABN forms provide?
ABN forms generally provide you with 3 options. Here are the actual options, plus some additional insight:
Do you have to deliver ABN form?
Your doctor, healthcare provider or supplier must deliver the ABN form before providing the recommended items or services. 1 In fact, it must be given far in advance so you have time to consider your options without feeling rushed. 2
Does Medicare cover all services?
Original Medicare may not cover all of the services or items you need. If a Medicare payment is expected to be denied, you must be provided an Advanced Beneficiary Notice of Noncoverage (ABN) before receiving the items or services.
What is a Medicare ABN?
Medicare’s Advance Beneficiary Notice (ABN) of Noncoverage is a form that you must issue to your office patients when you believe that Medicare may not pay or cover a proposed treatment, service, or item.
What is a Mandatory Medicare ABN?
Medicare requires you to issue an ABN to a patient when you have reason to believe that a proposed treatment, service, or item that Medicare typically covers, won’t be covered in the patient’s situation. This is considered a mandatory ABN, and you would use this type in the following situations:
What are Medicare ABN Modifier Requirements?
There are so many different situations that can affect which ABN you should use. For example, do you know:
What happens if Medicare doesn't pay?
Option 1: The patient agrees to the service/item, that you will bill Medicare, and if Medicare doesn’t pay, he or she will be financially responsible.
When is ABN required for telemedicine?
Screenings outside coverage areas: Issue a mandatory ABN when a patient requests a screening in an area not covered by policies such as a request for a telemedicine screening outside a rural coverage area.
Does Medicare cover discontinuation of care?
Discontinuation of care: When the provider has determined that a patient no longer needs a service, but the patient disagrees and wants to continue, Medicare probably will not cover the service any longer. In these cases, you must issue an ABN so that you can collect from the patient directly.
What is an ABN for Medicare?
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying you: Medicare may deny payment for that specific procedure or treatment. You will be personally responsible for full payment if Medicare denies payment.
What is an ABN number?
An ABN is a unique 11 digit number that identifies your business to the government and community. You can use an ABN to: identify your business to others when ordering and invoicing. avoid pay as you go (PAYG) tax on payments you get.
What does an ABN look like?
The ABN is an 11-digit number where the first two digits are a checksum. Unlike with the tax file number (TFN), the ATO has publicised the formula for checking and creating valid ABN checksums. Also, the nature of the ABN algorithm means that any 9-digit number can be made into a valid ABN.
Is an ABN required for Medicare Advantage plans?
Medicare Advantage Plans usually do not require the same type of Advance Beneficiary Notice (ABN) as traditional Medicare. Therefore, it's critical when you verify each plan, you determine whether the carrier has its own ABN form that you are required to use.
What happens if Medicare denies a claim?
If Medicare refuses to pay for a service under Original fee-for-service Part A or Part B, the beneficiary should receive a denial notice. The medical provider is responsible for submitting a claim to Medicare for the medical service or procedure.
What happens if a patient refuses to sign an ABN?
However, Medicare's Refund Requirement clause still protects patients who refuse to sign the ABN. Providers can deny a service to a beneficiary who has refused to sign an ABN unless the consequences (e.g., health and safety of the patient or civil liability in the case of harm) rule out this option.
What is an advance beneficiary notice?
An Advance Beneficiary Notice (ABN), also known as a waiver of liability, is a notice a provider should give you before you receive a service if, based on Medicare coverage rules, your provider has reason to believe Medicare will not pay for the service.
What Type of Medicare Is Subject to ABNs?
You'll only receive an ABN if you have Original Medicare, which consists of Part A (hospital insurance) and Part B (doctor’s visits, medical equipment, ambulance service). These plans are issued directly by Medicare. If you have a Medicare Advantage plan from a private health insurance company, you won't receive an ABN for any service or treatment.
How Does the ABN Appeal Process Work?
If Medicare denies the claim and you believe the item or service should be covered, you have the option to appeal the decision. To file an appeal, you must:
What is an advanced beneficiary notice of non-coverage?
The Advanced Beneficiary Notice of Non-Coverage (ABN) is a form required by Medicare. It advises the patient that the procedure being performed might not be covered and paid by Medicare fiscal intermediary or carrier. Consequently, the patient is given the opportunity to knowingly pay for the service should its reimbursement be declined or to [voluntarily] refuse the service. By signing the ABN and accepting to continue with the procedure, the patient accepts financial responsibility for paying should the reimbursement to the provider be declined. The ABN is a requirement for any procedure or service that the provider knows could be rejected.
What is a PDF rewriter for Medicare?
PDF rewriter allows you to create changes on your Medicare ABN Form 2021 CMS-R-131 2021 from the net connected gadget, customize it according to your needs, indicator that digitally and also deliver in different ways.
What is DME billing?
DME billing is all about billing for the services or equipment either prescribed to the patient or used in the treatment procedure. The different steps involved in DME billing include are the same steps which make up an RCM cycle. When a patient visits a provider’s office, he provides his insurance information, signs the ABN document, ABN and other necessary forms. The entire treatment process is recorded both visually and in an audio format. This recording is then sent to the medical transcription team who convert the entire conversation into a readable format. Codes are assigned for the ser... What is a good medical equipment billing software? What is the structure of a Durable Medical Equipment (DME) supply company? How does a DME (durable medical equipment) distributor's business model operate in the US? What are some examples of durable medical equipment? How do you sell durable medical equipments?