The appeals process starts with your Medicare Summary Notice or MSN MSN is a web portal and related collection of Internet services and apps for Windows and mobile devices, provided by Microsoft and launched on August 24, 1995, the same release date as Windows 95.MSN
Who receives a Medicare summary notice?
The Medicare Summary Notice is only for people with Original Medicare. That includes Part A and Part B. If you have Medicare Part D (standalone prescription drug coverage) or a Medicare Advantage plan, you won’t get a summary notice. You’ll get an Explanation of Benefits (EOB) instead, and it may come more often than every three months.
How long to keep Medicare summary notices?
Most experts recommend saving your Medicare summary notices for one to three years. At the very least, you should keep them while the medical services listed are in the process of payment by Medicare and supplemental insurance. How long you keep these records depends on your personal preference.
How to understand Medicare summary notices?
What should I do if I get this notice?
- If you have other insurance, check to see if it covers anything that Medicare didn’t.
- Keep your receipts and bills, and compare them to your MSN to be sure you got all the services, supplies, or equipment listed.
- If you paid a bill before you got your notice, compare your MSN with the bill to make sure you paid the right amount for your services.
What are the levels of Medicare appeal?
There are five levels in the Medicare claims appeal process:
- Level 1: Your Health Plan. If you disagree with a Medicare coverage decision, you may request your health plan to redetermine your claim.
- Level 2: An Independent Organization. ...
- Level 3: Office of Medicare Hearings and Appeals (OMHA). ...
- Level 4: The Medicare Appeals Council. ...
- Level 5: Federal Court. ...
What are the chances of winning a Medicare appeal?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.
What are the steps taken when appealing a Medicare claim?
Left navigationFile a complaint (grievance)File a claim.Check the status of a claim.File an appeal. Appeals if you have a Medicare health plan. Get help filing an appeal.Your right to a fast appeal.Authorization to Disclose Personal Health Information.
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
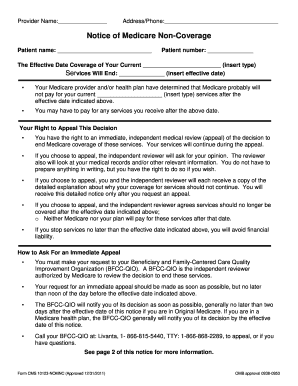
What is the purpose of the Nomnc Notice of Medicare non coverage?
A Notice of Medicare Non-Coverage (NOMNC) is a notice that indicates when your care is set to end from a home health agency (HHA), skilled nursing facility (SNF), comprehensive outpatient rehabilitation facility (CORF), or hospice.
How long does it take Medicare to review an appeal?
about 60 daysHow Long Does a Medicare Appeal Take? You can expect a decision on your Medicare appeal within about 60 days. Officially known as a “Medicare Redetermination Notice,” the decision may come in a letter or an MSN. Medicare Advantage plans typically decide within 14 days.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
Which of the following are reasons a claim may be denied?
Here are the top 5 reasons why claims are denied, and how you can avoid these situations.Pre-Certification or Authorization Was Required, but Not Obtained. ... Claim Form Errors: Patient Data or Diagnosis / Procedure Codes. ... Claim Was Filed After Insurer's Deadline. ... Insufficient Medical Necessity. ... Use of Out-of-Network Provider.
Can you be denied Medicare coverage?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
What is the purpose of the appeals process is it an effective process?
The first thing to understand is what the purpose of the appeals process actually is. Rather than being a re-trying of your case, it is a judicial review of the decision of the trial court that heard it initially. A judge will review all the relevant facts and determine if a harmful legal error occurred.
Who gets a Nomnc?
A Medicare provider or health plan (Medicare Advantage plans and cost plans , collectively referred to as “plans”) must deliver a completed copy of the Notice of Medicare Non-Coverage (NOMNC) to beneficiaries/enrollees receiving covered skilled nursing, home health (including psychiatric home health), comprehensive ...
When must you provide a client with an Nomnc Notice of Medicare non-coverage )?
Important: the NOMNC form should be issued no later than two days before the proposed end of services. space directly below the Highmark product logo, on the first page of the form. under which the member has coverage. If this is not the case, please select the appropriate form.
What is a Nomnc for?
The NOMNC letter is a Centers for Medicare and Medicaid Services (CMS) approved form that a provider must deliver to a Medicare Advantage patient receiving covered skilled services, such as home health, in certain situations when services are terminating.
How do you appeal?
How to Write an Appeal Letter in 6 Simple StepsReview the appeal process if possible.Determine the mailing address of the recipient.Explain what occurred.Describe why it's unfair/unjust.Outline your desired outcome.If you haven't heard back in one week, follow-up.Appeal letter format.
How do I correct a rejected Medicare claim?
When a claim is denied because the information submitted was incorrect, often the claim can be reopened using a Clerical Error Reopening (CER). CERs can be used to fix errors resulting from human or mechanical errors on the part of the party or the contractor.
How do I appeal a Medicare Part B premium?
First, you must request a reconsideration of the initial determination from the Social Security Administration. A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772. 1213) as well as by writing to SSA.
How long does Kepro have to make a decision?
The Medicare Advantage plan has information about how to start the appeal process. If you feel you may get worse by waiting too long, you can ask for an expedited appeal. This means the Medicare Advantage plan must make a decision about the appeal within three calendar days.
What happens if Medicare denies coverage?
If Medicare denies coverage of an item or service, an individual has the right to appeal the decision. People must provide proof with a claim and submit this to Medicare with an application form.
What is a fast appeal?
If waiting for a decision would affect a person’s health, they can ask for a fast appeal. An example of the need for a fast decision might be if someone is an inpatient in a hospital or SNF and they are concerned that the facility is discharging them too soon.
What is Medicare appeal?
It helps to provide evidence that supports your appeals case from a doctor or other provider. There might be times when Medicare denies your coverage for an item, service, or test. You have the right to formally disagree with this decision and encourage Medicare to change it. This process is called a Medicare appeal.
Why do you appeal Medicare?
Reasons for appeal. Appeals process. Takeaway. You’ll receive a notice when Medicare makes any decisions about your coverage. You can appeal a decision Medicare makes about your coverage or price for coverage. Your appeal should explain why you don’t agree with Medicare’s decision. It helps to provide evidence that supports your appeals case ...
Why is Medicare denying my coverage?
There are a few reasons Medicare might deny your coverage, including: Your item, service, or prescription isn’t medically necessary.
What is a fast appeal?
In a few cases, you’ll file what’s called a fast appeal. Fast appeals apply when you’re notified that Medicare will no longer cover care that’s: at a hospital. at a skilled nursing facility. at a rehabilitation facility. in hospice.
How long does it take to get a decision from Medicare?
You’ll hear a decision about your appeal within 60 days.
What is level 3 appeal?
At level 3, you’ll have the chance to present your case to a judge. You’ll need to fill out a request form detailing why you disagree with your level 2 decision. Your appeal will only be elevated to level 3 if it reaches a set dollar amount. Office of Medicare Hearings and Appeals review.
How many levels of appeals are there?
The appeals process has five levels. Each level is a different review process with a different timetable. You’ll need to request an appeal at each level. If your appeal is successful at the first level, or if you agree with Medicare’s reasoning for denying your appeal, you can stop there. However, if your appeal was denied ...
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What is a home health change of care notice?
The “Home Health Change of Care Notice” is a written notice that your home health agency should give you when your home health plan of care is changing because of one of these:
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
Who can help you file an appeal for Medicare?
You can get help filing your appeal from your doctor, family members, attorneys, or advocates. As a Medicare beneficiary, you have certain rights. One of them is the right to appeal a Medicare decision that you think is unfair or will jeopardize your health. The Medicare appeals process has several levels.
What happens if Medicare Appeals Council isn't in your favor?
If the decision of the Medicare Appeals Council isn’t in your favor, you can present your case to a judge in federal district court. The amount of money you’re asking Medicare to pay must meet a set amount to proceed with an appeal in court.
What to do if Medicare won't pay for your care?
If Medicare won’t cover your care, you can start the appeals process then. Pay for your continued care out of pocket.
What is the Medicare number?
your Medicare number (as shown on your Medicare card) the items you want Medicare to pay for and the date you received the service or item. the name of your representative if someone is helping you manage your claim. a detailed explanation of why Medicare should pay for the service, medication, or item.
How long does it take for Medicare to issue a decision?
The Office of Medicare Hearings and Appeals should issue a decision in 90 to 180 days. If you don’t agree with the decision, you can apply for a review by the Medicare Appeals Council.
What happens if Medicare refuses to pay for medical care?
If Medicare refuses to cover care, medication, or equipment that you and your healthcare provider think are medically necessary, you can file an appeal. You may also wish to file an appeal if Medicare decides to charge you with a late enrollment penalty or premium surcharge.
How many levels of appeal are there for Medicare?
There are five levels of appeal for services under original Medicare, and your claim can be heard and reviewed by several different independent organizations. Here are the levels of the appeal process: Level 1. Your appeal is reviewed by the Medicare administrative contractor. Level 2.
What is a CMS model notice?
CMS model notices contain all of the elements CMS requires for proper notification to enrollees or non-contract providers, if applicable. Plans may modify the model notices and submit them to the appropriate CMS regional office for review and approval. Plans may use these notices at their discretion.
How long does a hospital have to issue a notice to enrollees?
As under original Medicare, a hospital must issue to plan enrollees, within two days of admission, a notice describing their rights in an inpatient hospital setting, including the right to an expedited Quality Improvement Organization (QIO) review at their discharge. (In most cases, a hospital also issues a follow-up copy of this notice a day or two before discharge.) If an enrollee files an appeal, then the plan must deliver a detailed notice stating why services should end. The two notices used for this purpose are:
What are the different types of notices?
The following model notices are available in both Microsoft Word and PDF formats in the "Downloads" section below: 1 Notice of Right to an Expedited Grievance 2 Waiver of Liability Statement 3 Notice of Appeal Status 4 Notice of Dismissal of Appeal
When does a plan issue a written notice?
A plan must issue a written notice to an enrollee, an enrollee's representative, or an enrollee's physician when it denies a request for payment or services. The notice used for this purpose is the:
What is a MOON in Medicare?
Medicare Outpatient Observation Notice (MOON) Hospitals and CAHs are required to provide a MOON to Medicare beneficiaries (including Medicare Advantage health plan enrollees) informing them that they are outpatients receiving observation services and are not inpatients of a hospital or critical access hospital (CAH).
What to do if you decide to appeal a health care decision?
If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision.
What happens if my Medicare plan doesn't decide in my favor?
Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
How to appeal a denied Medicare claim?
If a claim was denied, first contact your provider’s office to make sure there was not a billing error leading to the denial. If the reason for the denial is not provided in your MSN, contact 1-800-Medicare to inquire further. If the reason for denial is not provided in your EOB, contact your plan for that information. The reason for denial will help determine your next steps. You can appeal a decision:
Who can file an appeal for you?
loved one, social worker, caregiver, or other chosen party may file an appeal for you. However, you may need to fill out a form saying that the person you select is your authorized representative. You can appoint your representative by completing an “Appointment of Representative” form (CMS Form
How old is Penny from Medicare Advantage?
Penny is 67 years old and recently selected a new primary care physician. This month, she received a bill from this new doctor for her Annual Wellness Visit. Penny was confused because she knew that her Medicare Advantage Plan should cover the full cost of this visit. When Penny contacted her plan, she learned that this visit had been denied because her former primary care physician had already billed the plan for it. Penny has not visited her former primary care physician at all this year. She worries that she may be the victim of fraudulent billing.
What to do if Medicare denied a service?
If you receive a health service denial from Original Medicare or your Medicare Advantage Plan, always call your doctor’s office to ensure they did not make a billing mistake before proceeding with an appeal. If you receive a drug denial, call your plan to check for potential errors before requesting a formal denial notice.
How old is Mai from Medicare?
Mai is 75 years old and has Original Medicare. She received a Medicare Summary Notice (MSN) that indicated she was denied coverage for her home health care based upon not being considered homebound. Mai is confused about why the care was denied and worries that she will not be able to pay her bill. She is not sure of her rights.
Can you appeal if you miss the deadline?
Submitting your appeal by the deadline will ensure that your appeal is fully considered. However, if you miss the deadline, you may be able to extend it by asking for a Good Cause Extension. You can receive a Good Cause Extension if you have a valid reason for not appealing in time. Reasons for a Good Cause Extension include, but aren’t limited to:
How long does it take to appeal a Medicare denial?
If an individual has original Medicare, they have 120 days to appeal the decision starting from when they receive the initial Medicare denial letter. If Part D denies coverage, an individual has 60 days to file an appeal. For those with a Medicare Advantage plan, their insurance provider allows 60 days to appeal.
How to contact Medicare if denied?
If an individual does not understand why they have received the Medicare denial letter, they should contact Medicare at 800-633-4227, or their Medicare Advantage or PDP plan provider to find out more.
Why is Medicare denial letter important?
Medicare’s reasons for denial can include: Medicare does not deem the service medically necessary. A person has a Medicare Advantage plan, and they used a healthcare provider outside of the plan network.
How long does it take for Medicare to redetermine a claim?
Medicare should issue a Medicare Redetermination Notice, which details their decision within 60 calendar days after receiving the appeal.
What is an IDN for Medicare?
Notice of Denial of Medical Coverage. Medicare may send a Notice of Denial of Medical Coverage or Integrated Denial Notice (IDN) to those who have either Medicare Advantage or Medicaid.
What happens if Medicare does not pay for a service?
Summary. If Medicare does not agree to pay for a service or item that a person has received, they will issue a Medicare denial letter. There are many different reasons for coverage to be denied. Medicare provides coverage for many medical services to those aged 65 and over. Younger adults may also be eligible for Medicare if they have specific ...
What is SNF-ABN?
A Skilled Nursing Facility Advanced Beneficiary Notice (SNF-ABN) lets a beneficiary know in advance that Medicare will not pay for a specific service or item at a skilled nursing facility (SNF). In this case, Medicare may decide that the service is not medically necessary.
