
What are S codes in medical billing?
The NDC is 10-digits divided into three segments:
- The first segment identifies the product labeler (manufacturer, marketer, repackager, or distributor of the product).
- The second segment identifies the product itself (drug-specific strength, dosage form, and formulation).
- The third segment identifies the package size and type.
What are the medical billing codes?
Medical billing can be a huge task ... Check if the staff is proficient in ICD-10, HCPCS, CPT codes and if the company is ISO-certified and HIPAA (Health Insurance Portability and Accountability Act) compliant. Ask about their rate of rejected claims ...
Where to find billing codes?
Medical billing and coding are also boosted with the software ... of Law for Health Information Management SHARE THIS POST Find News News
What are the two types of medical billing?
- Patient Check-in and Check-out. Patient check-in and check-out are relatively straight-forward front-of-house procedures. ...
- Prepare Claims/Check Compliance. ...
- Transmit Claims. ...
- Monitor Adjudication. ...
- Generate patient statements. ...
- Follow up on patient payments and handle collections. ...
What is a billing code?
A Billing Code Type is a label used to identify work performed for billing purposes. For example, if you bill for every 40-foot container that is unloaded, create a BIlling Code Type for that work (e.g. CONTAINER-40).
Does Medicare use CPT codes?
For Part B services, Medicare pays physicians based on the services they provide. The American Medical Association (AMA) developed Current Procedural Terminology (CPT) codes to create a taxonomy of procedures that physicians perform.
What is Medicare billing code 99214?
According to CPT, 99214 is indicated for an “office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three key components: a detailed history, a detailed examination and medical decision making of moderate complexity.” [For more detailed ...
What are the codes for medical billing?
There are three types of medical billing codes used in the U.S. healthcare system:International Classification of Diseases (ICD) codes.Current Procedure Terminology (CPT) codes.Healthcare Common Procedure Coding system (HCPCS) codes.
Where do I find Medicare CPT codes?
To find the CPT or HCPCS billing code, look on the bill provided to you by your health care provider. You may also download a zip file of the 2022 HCPCS codes, then select the “January 2022 Alpha-Numeric HCPCS File (ZIP).”
What CPT codes are not covered by Medicare?
Certain services are never considered for payment by Medicare. These include preventive examinations represented by CPT codes 99381-99397. Medicare only covers three immunizations (influenza, pneumonia, and hepatitis B) as prophylactic physician services.
What's the difference between 99213 and 99214?
In a typical 99213 visit, you may not need to review or update the patient's PFSH at all, but a 99214 requires at least one of those areas be reviewed and documented.
What is the difference between 99214 and 99215?
To get an idea of the monetary difference between the two codes, a major national healthcare insurer's policies list CPT Code 99214 as reimbursable for up to $107.20 for each patient. With the same insurer, CPT Code 99215 is reimbursable for up to $144.80 for each patient.
What is code 99213 used for?
CPT® code 99213: Established patient office or other outpatient visit, 20-29 minutes.
How do you find the code?
PCFirefox – CTRL + U (Meaning press the CTRL key on your keyboard and hold it down. While holding down the CTRL key, press the "u" key.) ... Internet Explorer – CTRL + U. Or right click and select "View Source."Chrome – CTRL + U. ... Opera – CTRL + U.
What is an example of medical coding?
Medical Coding Example 1 In this medical coding example, the coder receives a patient record on abscess drainage and needs to translate the information regarding the indications, medication and procedure into medical codes according to intervention radiology CPT codes.
What are the types of medical coding?
Medical Coding involves the following types of codes.ICD Codes.CPT Codes.HCPCS Codes.DRG Codes.Modifiers.
What is Medicare reimbursement rate?
A Medicare reimbursement rate is the amount of money that Medicare pays doctors and other health care providers for the services and items they administer to Medicare beneficiaries. CPT codes are the numeric codes used to identify different medical services, procedures and items for billing purposes. When a health care provider bills Medicare ...
How much does Medicare pay for coinsurance?
In fact, Medicare’s reimbursement rate is generally around only 80% of the total bill as the beneficiary is typically responsible for paying the remaining 20% as coinsurance. Medicare predetermines what it will pay health care providers for each service or item. This cost is sometimes called the allowed amount but is more commonly referred ...
What is the difference between CPT and HCPCS?
The CPT codes used to bill for medical services and items are part of a larger coding system called the Healthcare Common Procedure Coding System (HCPCS). CPT codes consist of 5 numeric digits, while HCPCS codes ...
How much more can a health care provider charge than the Medicare approved amount?
Certain health care providers maintain a contract agreement with Medicare that allows them to charge up to 15% more than the Medicare-approved amount in what is called an “excess charge.”.
Is it a good idea to check your Medicare bill?
It’s a good idea for Medicare beneficiaries to review their medical bills in detail. Medicare fraud is not uncommon, and a quick check of your HCPCS codes can verify whether or not you were correctly billed for the care you received.
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
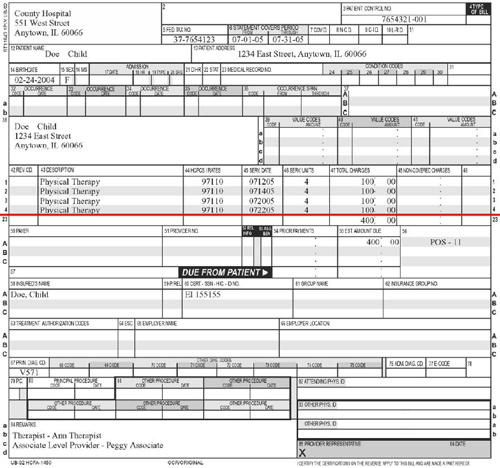
What form do you need to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500. For the most part, however, billers will enter the proper information into a software program and then use ...
What is 3.06 Medicare?
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
Is it harder to bill for medicaid or Medicare?
Billing for Medicaid. Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program ...
Can you bill Medicare for a patient with Part C?
Because Part C is actually a private insurance plan paid for, in part, by the federal government, billers are not allowed to bill Medicare for services delivered to a patient who has Part C coverage. Only those providers who are licensed to bill for Part D may bill Medicare for vaccines or prescription drugs provided under Part D.
Do you have to go through a clearinghouse for Medicare and Medicaid?
Since these two government programs are high-volume payers, billers send claims directly to Medicare and Medicaid. That means billers do not need to go through a clearinghouse for these claims, and it also means that the onus for “clean” claims is on the biller.
Who maintains CPT codes?
All these CPT codes describe the insurance payer company what services and procedures performed on patients and also show the exact fee or charges of services. The American Medical Association (AMA) is the responsible body to maintains the CPT coding and their fee structure.
How many categories are there in CPT codes?
CPT code s are five characters long codes and it may be in form of numeric or alphanumeric. CPT codes are divided into 3 Categories. 1- Category -1 – The first type of CPT codes are in category 1 codes. These are common codes and widely used in medical billing and coding and revenue cycle management. 2-Category II – These codes are supplemental and ...
What is CPT code 2021?
March 27, 2021. March 27, 2021 by medicalbillingrcm. CPT Codes stands for Current Procedure Terminology Codes and all these codes are used to describe medical services and procedures, tests, surgeries, etc, performed by a health professional or doctor on a patient.
What is the revenue code for inpatient admissions?
Revenue code – In relation to inpatient admissions. • Revenue Code 760 is not allowed because it fails to specify the nature of the services. • Revenue Code 761 is acceptable when an exam or relatively minor treatment or procedure is performed.
Why is it important to bill with the correct NPI?
It is important to bill with the correct NPI for the service you provided or this could delay payment or even result in a denial of a claim. Patient Status The appropriate patient status is required on an inpatient claim. An incorrect patient status could result in inaccurate payments or a denial.
