Medicare Certification means certification of a facility by CMS The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…Centers for Medicare and Medicaid Services
Full Answer
How to obtain a CMS certification number?
- Public agency is an agency operated by a State or local government. Examples include State-operated HHAs and county hospitals. ...
- Nonprofit agency is a private (i.e., nongovernmental) agency exempt from Federal income taxation under §501 of the Internal Revenue Code of 1954. ...
- Proprietary agency is a private, profit-making agency or profit-making hospital.
How do I Find my CMS certification number?
Where do I find my CMS certification number?
- Where do I find my CMS certification number?
- What is the maximum number of days of skilled nursing facility care for which Medicare will pay benefits?
- What is a skilled nursing facility Medicare?
- How many days does Medicare cover in a skilled nursing facility?
- What modifier is used for skilled nursing facility?
What is CMS certification?
“CMS is working with the New Jersey State Department of Health regarding the serious issues identified at Woodland Behavioral Health and Nursing Center, formerly known as the Andover Subacute and Rehabilitation Center.”
Is CMS accredited?
Is CMS an accrediting body? Accreditation is voluntary and seeking deemed status through accreditation is an option, not a requirement. Organizations seeking CMS approval may choose to be surveyed either by an accrediting body, such as the Joint Commission, DNV, and HFAP, or by state surveyors on behalf of CMS.

What is a CMS certificate?
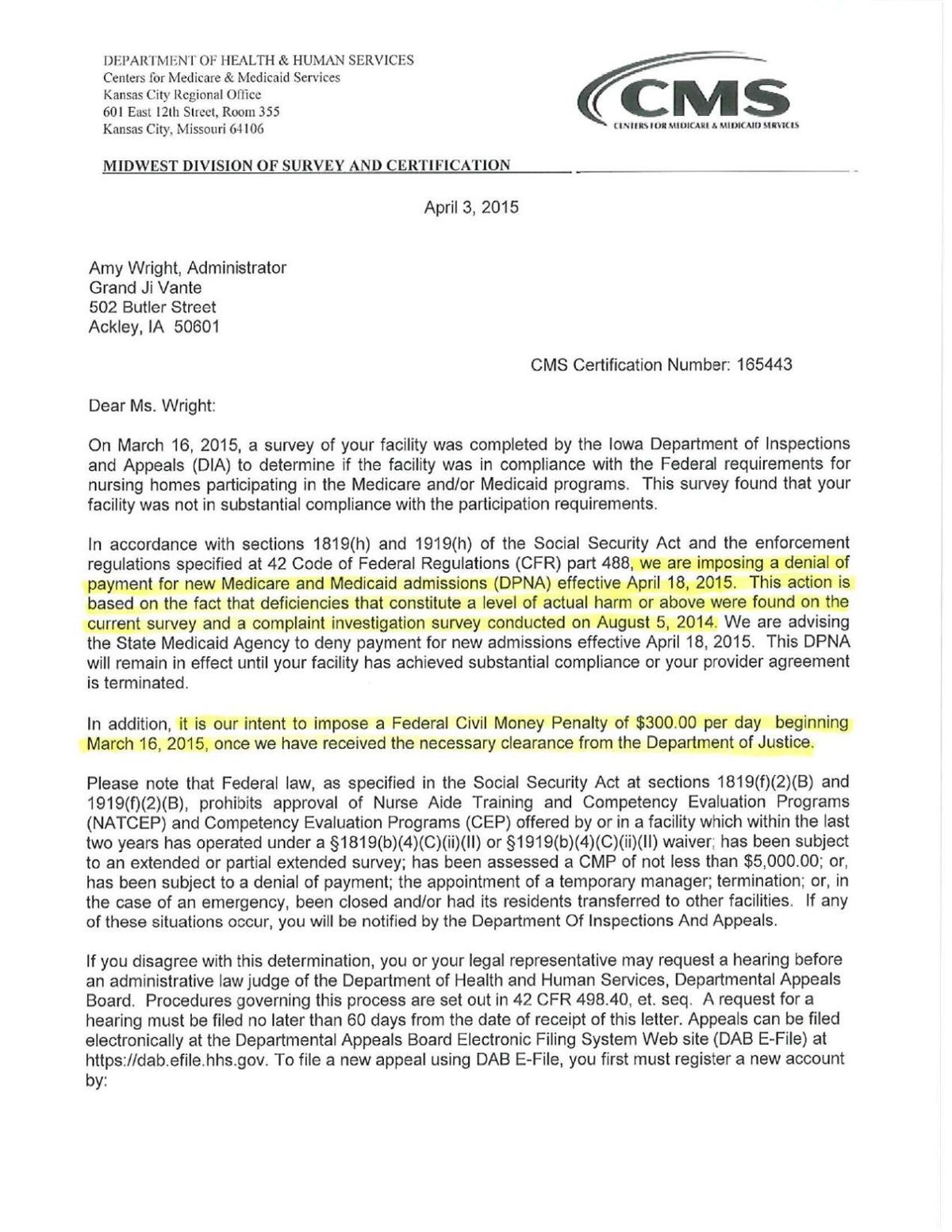
The CMS Certification number (CCN) replaces the term Medicare Provider Number, Medicare Identification Number or OSCAR Number. The CCN is used to verify Medicare/Medicaid certification for survey and certification, assessment-related activities and communications. The RO assigns the CCN and maintains adequate controls.
What is a CMS letter?
Children's Medical Services (CMS) Letters
What is a CMS approval letter?
This letter is to inform you that the Centers for Medicare and Medicaid Services (CMS) has approved the attached evaluation design for the Whole Person Care (WPC) Pilots authorized under the section 111 S(a) demonstration entitled "Medi-Cal 2020" (11-W-00193/9), as submitted by the state and as modified through our ...
Why would I get a letter from CMS?
In general, CMS issues the demand letter directly to: The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment.
What is the role of CMS?
The Centers for Medicare and Medicaid Services (CMS) provides health coverage to more than 100 million people through Medicare, Medicaid, the Children's Health Insurance Program, and the Health Insurance Marketplace.
What is CMS policy?
The CMS oversees programs including Medicare, Medicaid, the Children's Health Insurance Program (CHIP), and the state and federal health insurance marketplaces. CMS collects and analyzes data, produces research reports, and works to eliminate instances of fraud and abuse within the healthcare system.
Do Medicare benefits have to be repaid?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
Is CMS legitimate?
The Centers for Medicare & Medicaid Services (CMS), is a federal agency within the United States Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid, the Children's Health Insurance Program (CHIP), and health ...
What is CMS Healthcare?
The federal agency that runs the Medicare, Medicaid, and Children's Health Insurance Programs, and the federally facilitated Marketplace.
What does CMS termination mean?
If you have received a CMS Termination Letter, it has been determined that your hospital has a condition-level deficiency. This means your hospital is not in substantial compliance with one or more of the CMS Conditions of Participation.
What is a Medicare certification letter?
Medicare certification letter is issued by a central insurance program to provide great range of reimbursement for definite periods of time. In the terminology of Medicare, providers are normally patient care institutions such as medical centers, hospitals, nursing homes, and other health agencies providing services at home.
What is a supplier in Medicare?
Suppliers are diagnosis or therapy provides by pathology laboratori es, clinics, and ambulatory agencies. At the time of services furnished through these providers or suppliers, must be certified for Medicare. This certification letter is most likely written by a senior medical officer for a patient. It gives details of the patient’s condition.
What is AO in Medicare?
Section 1865 (a) (1) of the Social Security Act (the Act) permits providers and suppliers "accredited" by an approved national accreditation organization (AO) to be exempt from routine surveys by State survey agencies to determine compliance with Medicare conditions.
Is AO required for Medicare?
Accreditation by an AO is voluntary and is not required for Medicare certification or participation in the Medicare Program. A provider’s or supplier’s ability to bill Medicare for covered services is not impacted if it chooses to discontinue accreditation from a CMS-approved AO or change AOs.
How to get a CMS certification number?
1. Gather all relevant governmental documentation. The process for getting a new CMS Certification Number usually requires many legal documents. Before you begin, make sure you know where to find all legal documentation of your organization so that you can avoid delays during the application process. Now is a good time to sort through your file ...
How to send a form as a PDF?
1. Prepare the form for sending. If you have completed the form as a pdf file you will need to print it out. Make sure you print if from a good quality printer so that the ink contrast is strong and place it in a neat pile.
Is CMS 855A encompassing?
CMS-855A is widely encompassing, so if none of the other forms apply to you, make sure to check this one. ...
Does Medicare cover operations?
Medicare may be available to cover the costs of your operations, such as if you’re providing care to those over 65. The CMS Certification Number application process is simple once you know what you're doing and the various websites associated with CMS and Medicare hold plenty of FAQ's the answer any questions. Steps.
What is the authority of CMS to question state determinations regarding Medicaid facilities' compliance with Federal requirements?
Section 1902(a)(33) gives CMS the authority to question State determinations regarding Medicaid facilities' compliance with Federal requirements and authorizes CMS to make independent and binding determinations concerning the extent to which individual institutions and agencies meet requirements for participation.
When to enter Medicare code?
Enter code 1 when the provider/supplier is found eligible to participate in the Medicare and/or Medicaid programs. Also enter code 1 when a denial of payment for new admissions is imposed, continued, or lifted. Enter code 2 when a facility is not eligible to participate.
What does Section 1919(g)(3)(A) mean?
Section 1919(g)(3)(A) states that if the State determines that an individual NF meets Federal requirements, but CMS determines that the facility does not meet such requirements, CMS’ determination as to the facility's noncompliance is binding and supersedes that of the State.
What is CMS 2005?
Section 2005 has been revised to reflect the following: an applicant who is denied certification by the Centers for Medicare & Medicaid Services (CMS), based on a finding of substantial noncompliance from the initial survey, may reapply for certification.
What is the code for a facility that closes?
Code 1 - Enter when a facility closes or merges. Code 2 - Enter when a provider or supplier is voluntarily withdrawing because of dissatisfaction with reimbursement. Code 3 - Enter when a facility is leaving the program because it is at risk of being involuntarily terminated.
How to fill out and sign nade online?
Get your online template and fill it in using progressive features. Enjoy smart fillable fields and interactivity. Follow the simple instructions below:
Accredited Business
Guarantees that a business meets BBB accreditation standards in the US and Canada.