• CSC — Claim Status Code (required): Conveys the status of an entire claim or a specific service line. • EIC — Entity Identifier Code(when applicable) :Unique codes used to identify an entity (e.g., organization, facility, provider, and physical location, individual). Locate the Edit Information
Full Answer
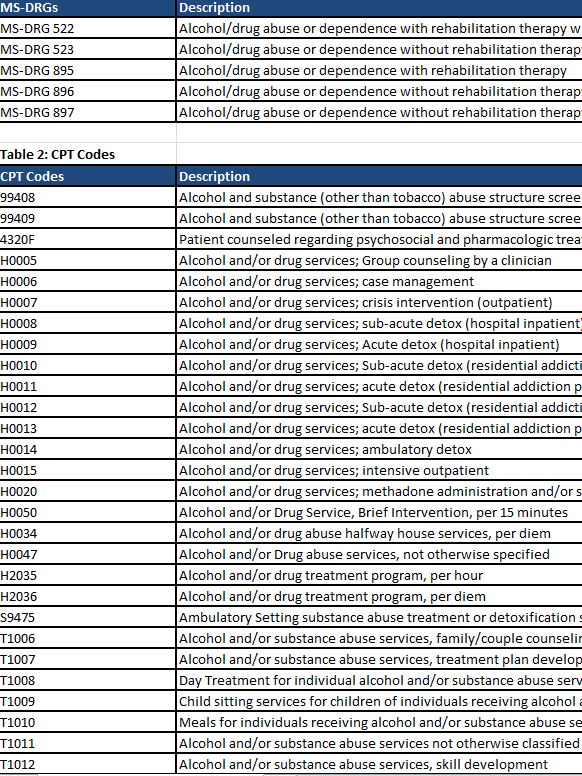
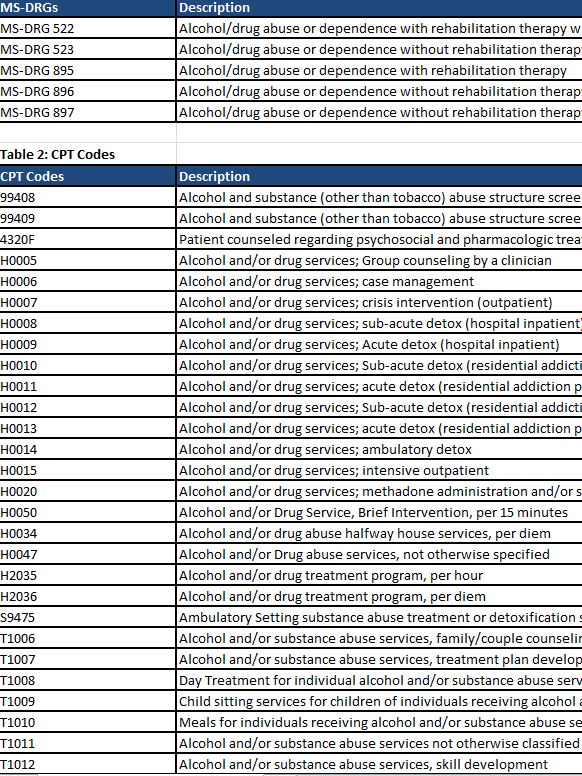
What diagnosis codes are covered by Medicare?
The entity in medical billing implies a relationship, any controlled liability company, that is directly or indirectly involved in the medical billing process. It involves the information of entities such as hospitals, doctors, patients, insurance companies, etc. The information on these factors is used in generating medical bills and codes for ...
What is an entity code on a medical claim?
Aug 13, 2018 · Any other message that was sent, such as "This code requires the use of an entity code (20)" is an extra message that is included but it doesn't mean much until the payer processes the claim. So, if your claims are in the Accepted status and have that message, you can ignore them until the payer processes the claims.
What is an entity code in medical billing?
Feb 25, 2020 · Definition: Secondary identification number for the provider or organization in whose name the bill is submitted and to whom payment should be made. What is rejection in medical billing? A rejected claim has been rejected because of errors.
What is a Medicare BIC code?
National Plan and Provider Enumeration System (NPPES) Data Dissemination – Code Values Prepared For Centers for Medicare and Medicaid Services
What is an Entity in Medical Billing?
An entity is a person or thing with an independent existence—hence an individual, or a corporation, would be an entity. The same is for medical billing, where the entity mentioned could be the patient, the provider, or even the medical billing service if the third-party biller medical billing company is used.
Entity Code Error in a Billing Claim
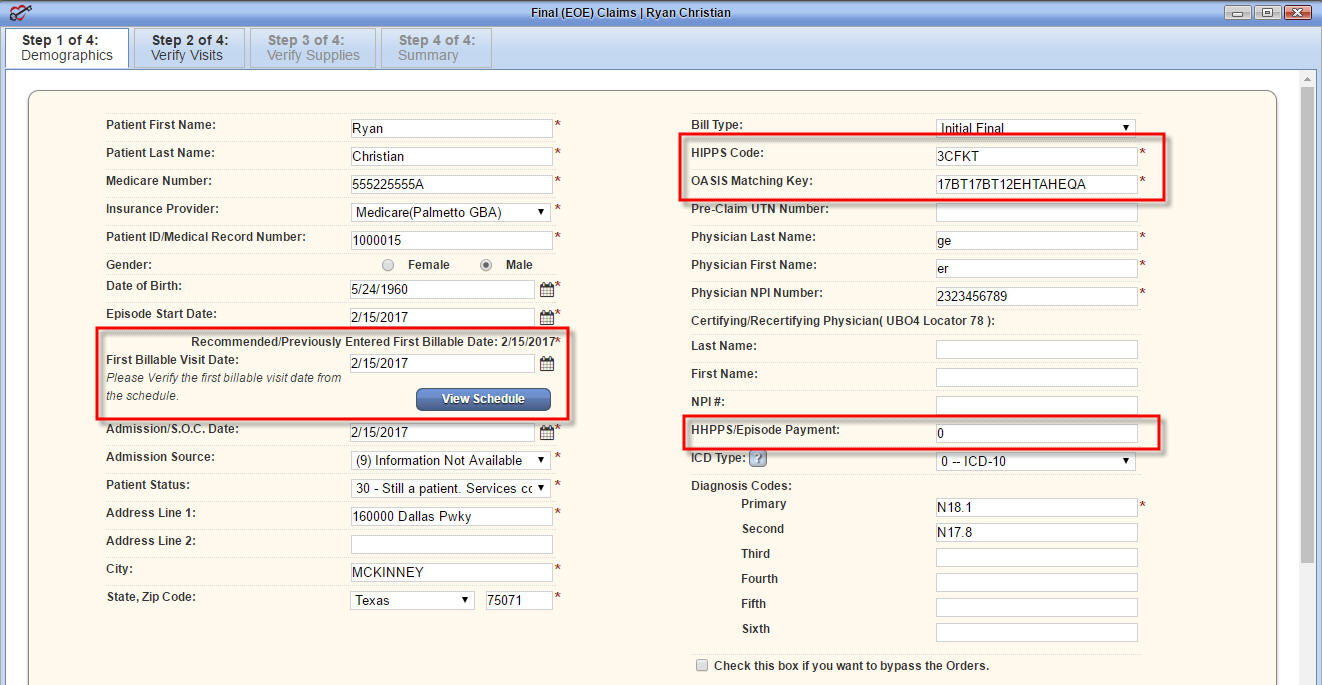
The entity code error is probably due to submitting a medical claim with the wrong billing NPI (the equivalent of Box 33 on the CMS-1500). Most payers have the NPI shared with them on file. After receiving a medical claim, they verify the NPI in their system to see if they have the billing NPI on file.
Billing Provider
Rendering Provider address, phone, do not go on claim, even so, they may be referencing the NPI.
Background
Section 1877 of the Social Security Act, also known as the physician self-referral law, prohibits the following: (1) a physician from making referrals for certain designated health services (''DHS'') payable by Medicare to an "entity" with which he or she (or an immediate family member) has a direct or indirect financial relationship (an ownership/investment interest or a compensation arrangement), unless an exception applies; and (2) the entity from presenting or causing a claim to be presented to Medicare (or billing another individual, entity, or third party payor) for those referred services.
Solicitation of Comments
Following the publication of the IPPS final rule, we received a number of inquiries concerning whether we planned to issue additional guidance on the revised definition of entity, including the meaning of "performed services that are billed as DHS." To determine if further guidance was necessary, we solicited comments in the CY 2010 Physician Fee Schedule final rule (74 FR 61933–34).
Comments Received
We received only nine comments responding to our solicitation, and there was no consistent approach regarding whether we should revise the definition of entity and if we did, the manner in which the definition should change.
CMS Response
The comments we received did not convince us to provide additional guidance or to engage in rulemaking to amend the definition of entity.
When was the self referral law enacted?
When enacted in 1989, Section 1877 of the Social Security Act (the Act) applied only to physician referrals for clinical laboratory services. In 1993 and 1994, Congress expanded the prohibition to additional DHS and applied certain aspects of the physician self-referral law to the Medicaid program. In 1997, Congress added a provision permitting ...
What is SRDP in healthcare?
The SRDP sets forth a process to enable providers of services and suppliers to self-disclose actual or potential violations of the physician self-referral statute. Additionally, Section 6409 (b) of the ACA, gives the Secretary of HHS the authority to reduce the amount due and owing for violations of Section 1877.
Background
- Section 1877 of the Social Security Act, also known as the physician self-referral law, prohibits the following: (1) a physician from making referrals for certain designated health services (''DHS'') payable by Medicare to an "entity" with which he or she (or an immediate family member) has a direct or indirect financial relationship (an ownership/...
Solicitation of Comments
- Following the publication of the IPPS final rule, we received a number of inquiries concerning whether we planned to issue additional guidance on the revised definition of entity, including the meaning of "performed services that are billed as DHS." To determine if further guidance was necessary, we solicited comments in the CY 2010 Physician Fee Schedule final rule (74 FR 6193…
Comments Received
- We received only nine comments responding to our solicitation, and there was no consistent approach regarding whether we should revise the definition of entity and if we did, the manner in which the definition should change. Several commenters asserted that a bright-line rule should be established to determine when a provider or supplier has "performed services that are billed as …
CMS Response
- The comments we received did not convince us to provide additional guidance or to engage in rulemaking to amend the definition of entity. We believe the guidance provided in the IPPS final rule is sufficient in most cases to identify when a provider or supplier has "performed the DHS." Providers and suppliers may seek further guidance through the advisory opinion process (42 CF…