How do you verify a Medicare number?
Medicare Beneficiary Identifier (MBI) Lookup through Novitasphere. Effective January 1, 2020, all claims and eligibility inquiries submitted to Medicare must use the new Medicare Beneficiary Identifier (MBI). If your patients are unable to provide you with their updated card, the MBI Lookup tool is available in Novitasphere, our free, secure internet portal!
How to find your Medicare number easily?
Just the essentials...
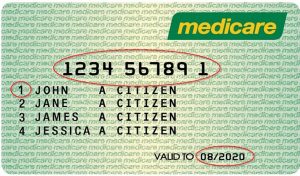
- Your Medicare number, also known as the Medicare Beneficiary Identifier (MBI), contains eleven random letters and numbers. ...
- You can also find it on paperwork you receive from the Social Security Administration. ...
- Formerly, the Medicare number consisted of a person’s Social Security Number along with an identifying letter at the end. ...
How to become Medicare Certified Provider?
- Public agency is an agency operated by a State or local government. Examples include State-operated HHAs and county hospitals. ...
- Nonprofit agency is a private (i.e., nongovernmental) agency exempt from Federal income taxation under §501 of the Internal Revenue Code of 1954. ...
- Proprietary agency is a private, profit-making agency or profit-making hospital.
What is a Dr NPI number?
Some of the organizations that require an NPI number include:
- Hospitals
- Nursing homes
- Labs
- Pharmacies
- Residential treatment facilities
- Medical equipment providers

Is Medicare number same as NPI?
What are the NPI and CCN numbers? The NPI is the National Provider Identifier, and is a unique identification number provided to facilities and other medical entities. The Medicare Provider Number is also known as the CCN (CMS Certification Number). This is the six-digit Medicare certification number for a facility.
Do you need a Medicare provider number?
A Medicare provider number is a unique number you can get if you're an eligible health professional recognised for Medicare services. You need a provider number to claim, bill, refer or request Medicare services.
Is Ptan the same as Medicare ID?
The Provider Transaction Access Number (PTAN) is your unique Medicare identification number. This number is assigned to providers once their enrollment has been approved.
How does Medicare define provider?
Provider is defined at 42 CFR 400.202 and generally means a hospital, critical access hospital, skilled nursing facility, comprehensive outpatient rehabilitation facility (CORF), home health agency or hospice, that has in effect an agreement to participate in Medicare; or a clinic, rehabilitation agency, or public ...
What documents do I need to apply for a Medicare provider number?
To apply for a Medicare Provider Number, you'll require:An offer of employment.Complete and sign the form HW019.AHPRA registration.A letter of support signed by the practice, and on practice letterhead stating why you require access to Medicare benefits and the period required.Identity documents including.More items...
Can I use a PO Box for Medicare?
You will be asked to supply a street address to remain eligible for insurance in a Medicare plan. P.O. Boxes are not acceptable as a home address.
What does a Medicare Ptan number look like?
The Provider Transaction Access Number (PTAN) is a Medicare-issued number given to providers upon enrollment with Medicare. This number is usually six digits and assigned based on the type and location of the provider. Upon enrollment, MAC providers should receive their assigned PTAN number in their approval letter.
What is a P10 Medicare number?
The "P10" number that Medicare may ask from a health-care provider over the phone is actually not "P10," but rather PTAN. It is an acronym Medicare uses that stands for "Provider Transaction Access Number."
What is a Pecos number?
The PECOS system is a database of providers who have registered with CMS. A National Provider Identifier (NPI) is necessary to register in PECOS. Use that identifier to search for the provider in the database. If you don't know the provider's NPI number, you can search for their information in the NPI registry.
What are the 3 different types of healthcare providers?
This article describes health care providers involved in primary care, nursing care, and specialty care.
What is an example of a healthcare provider?
Under federal regulations, a "health care provider" is defined as: a doctor of medicine or osteopathy, podiatrist, dentist, chiropractor, clinical psychologist, optometrist, nurse practitioner, nurse-midwife, or a clinical social worker who is authorized to practice by the State and performing within the scope of their ...
How do providers submit claims to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What is a Medicare provider number?
The article states that “A Medicare provider number is known as a “national provider identifier,” a ten-digit identification number for covered health care providers”. Obviously whoever wrote the article doesn’t understand the US Healthcare industry. Click here for an accurate description of how to obtain a Medicare Provider Number.
Do I need an NPI to enroll in Medicare?
Different provider types have varying enrollment requirements so become familiar with what your carrier needs to properly enroll you and/or your group. Yes, you must have an NPI to do business with any health insurance company including Medicare. But, your NPI is NOT your Medicare provider number.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
Medicare provider number applications
Most Medicare provider number applications are taking up to 22 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health.
About Medicare provider numbers
A Medicare provider number is a unique number you can get if you’re an eligible health professional recognised for Medicare services. You need a provider number to claim, bill, refer or request Medicare services.
When does Medicare use the term "secondary payer"?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare.
What information do you need to release a private health insurance beneficiary?
Prior to releasing any Private Health Information about a beneficiary, you will need the beneficiary's last name and first initial, date of birth, Medicare Number, and gender. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
Can a Medicare claim be terminated?
Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office.
How Do I Find My Medicare Provider Number?
The Centers for Medicare and Medicaid Services (CMS) uses something called the National Provider Identifier Standard to keep track of physicians who serve Medicare patients. As a result, each provider is assigned something called an NPI number. All Medicare providers are required to supply their NPI numbers to Medicare providers and third-party companies for billing purposes.
How many digits are in Medicare number?
The provider Medicare number format consists of nine numeric digits followed by a single numeric check digit.
How to get Medicare number?
Call your Medicare provider to request your number. This will require you to establish your identity. Have your full name, date of birth and Social Security number ready to share.
What is the Medicare number format?
The Medicare number format typically consists of your Social Security number followed by a special identifying code. It's also helpful to know what the "A" and "B" on your Medicare benefits signify. The A represents Medicare Part A benefits; these are your inpatient hospital benefits. The B represents Medicare Part B;
Do Medicare providers need to supply NPI?
All Medicare providers are required to supply their NPI numbers to Medicare providers and third-party companies for billing purposes. When doing a Medicare provider number lookup, you can utilize a Medicare provider number database.
Can you use NPI to look up a provider?
In addition, you can also simply call up a provider's office to ask to be given the NPI directly.
Is Medicare provider number private?
That means that you can easily call or look online to obtain this information. However, your personal Medicare number is private. That means that you'll need to supply the right information to verify your identification before you can recover your ...
What are Medicare providers and suppliers?
Medicare provider and supplier organizations have business structures, such as corporations, partnerships, Professional Associations (PAs), or Limited Liability Companies (LLCs) that meet the “provider” and “supplier” definitions. Provider and supplier organizations don’t include organizations the IRS defines as sole proprietorships.
How long does it take to become a Medicare provider?
You’ve 90 days after your initial enrollment approval letter is sent to decide if you want to be a participating provider or supplier.
How to change Medicare enrollment after getting an NPI?
Before applying, be sure you have the necessary enrollment information. Complete the actions using PECOS or the paper enrollment form.
How to request hardship exception for Medicare?
You may request a hardship exception when submitting your Medicare enrollment application via either PECOS or CMS paper form. You must submit a written request with supporting documentation with your enrollment that describes the hardship and justifies an exception instead of paying the application fee.
What form do MDPP suppliers use?
MDPP suppliers must use Form CMS-20134 to enroll in the Medicare Program.
What is Medicare 855I?
Medicare Enrollment Application: Physicians and Non-Physician Practitioners (Form CMS-855I): Individual physicians or NPPs, as well as individual physicians and NPPs that are sole proprietors or sole owners of a corporation that provides services, use this form to begin the Medicare enrollment/revalidation process or change Medicare enrollment information.
How much is the Medicare application fee for 2021?
Application Fee Amount. The enrollment application fee sent January 1, 2021, through December 31, 2021, is $599. For more information, refer to the Medicare Application Fee webpage. How to Pay the Application Fee ⤵. Whether you apply for Medicare enrollment online or use the paper application, you must pay the application fee online:

Coordination of Benefits Overview
- The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken ...
Information Gathering
- Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare. For example, information submitted on a medical claim or from other sour…
Provider Requests and Questions Regarding Claims Payment
- MACs, intermediaries, and carriers will continue to process claims submitted for primary or secondary payment. Claims processing is not a function of the BCRC. Questions concerning how to bill for payment (e.g., value codes, occurrence codes) should continue to be directed to your local Medicare claims paying office. In addition, continue to return inappropriate Medicare paym…
Medicare Secondary Payer Records in CMS's Database
- The BCRC is the sole authority to ensure the accuracy and integrity of the MSP information contained in CMS's database (i.e., Common Working File (CWF)). Information received because of MSP data gathering and investigation is stored on the CWF. MSP data may be updated, as necessary, based on additional information received from external parties (e.g., beneficiaries, pr…
Termination and Deletion of MSP Records in CMS's Database
- Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office. MSP records that you have identified as invalid are reported to the BCRC for investigation and deletion.
Contacting The BCRC
- The BCRC’s trained staff will help you with your COB questions. Whether you need a question answered or assistance completing a questionnaire, the Customer Service Representatives are available to provide you with quality service. Click the Contactslink for BCRC contact information. In order to better serve you, please have the following information available when you call: 1. Yo…
Contacting The Medicare Claims Office
- Contact your local Medicare Claims Office to: 1. Answer your questions regarding Medicare claim or service denials and adjustments. 2. Answer your questions concerning how to bill for payment. 3. Process claims for primary or secondary payment. 4. Accept the return of inappropriate Medicare payment.
Coba Trading Partner Contact Information
- The Coordination of Benefits Agreement (COBA) Program establishes a nationally standard contract between CMS and other health insurance organizations that defines the criteria for transmitting enrollee eligibility data and Medicare adjudicated claim data. CMS has provided a COBA Trading Partners customer service contact list as an avenue for providers to contact the t…
mln Matters Articles - Provider Education
- The Medicare Learning Network (MLN) is a CMS initiative to ensure Medicare physicians, providers and supplies have immediate access to Medicare coverage and reimbursement rules in a brief, accurate, and easy to understand format. To access MLN Matters articles, click on the MLN Matterslink.