A formulary is the list of drugs covered by a Part D plan. Medicare requires all Part D plans to cover at least two drugs in each therapeutic drug category. Some types of drugs are not covered by Medicare Part D, such as drugs for weight loss or cosmetic purposes.
What is the meaning of formulary drugs?
The formulary is maintained by an independent committee of practicing physicians and pharmacists. In simple terms, a formulary drug is a list of drugs for which your health insurer agrees to pay (at least partially) for a predefined or specified health condition or disease.
What are Tier 6 drugs?
during the forecast period. The growth of this market is majorly driven by the rising number of organ transplant procedures, the use of TDM across various therapeutic fields, the increasing preference for precision medicine, a growing focus on R&D related to TDM, and technological advancements in immunoassay instruments.
What is the Medicare Part D formulary?
- Tier 1: Preferred generic drugs
- Tier 2: Generic drugs
- Tier 3: Preferred brand drugs and select insulin drugs
- Tier 4: Non-preferred drugs
- Tier 5: Specialty drugs
Does Medicare cover Tier 5 drugs?
Specialty drugs are used to treat complex conditions like cancer and multiple sclerosis. They can be generic or brand name. For most plans, you’ll pay 25% to 33% of the retail cost for drugs in this tier. Select care. These are generic drugs used to treat diabetes and high cholesterol. For most plans, you'll pay $0-$5 for drugs in this tier.

How are formularies established for Medicare?
The health plan generally creates this list by forming a pharmacy and therapeutics committee consisting of pharmacists and physicians from various medical specialties. This committee evaluates and selects new and existing medications for what is called the (health plan's) formulary.
What is in a formulary?
A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
What are the two types of formularies?
Types of FormulariesOpen Formulary: The payer may provide coverage for all formulary and non-formulary drugs. The payers include the health plan, the employer, or a PBM acting on behalf of the health plan or employer. ... Closed Formulary: Non-formulary drugs are not reimbursed by the payer.
What type of medications are not covered on a formulary?
However, plans usually do not cover:Weight loss or weight gain drugs.Drugs for cosmetic purposes or hair growth.Fertility drugs.Drugs for sexual or erectile dysfunction.Over-the-counter drugs.
What is the purpose of a formulary?
The primary purpose of the formulary is to encourage the use of safe, effective and most affordable medications. A formulary system is much more than a list of medications approved for use by a managed health care organization.
What are the three types of formulary systems?
An open formulary has no limitation to access to a medication. Open formularies are generally large. A closed formulary is a limited list of medications. A closed formulary may limit drugs to specific physicians, patient care areas, or disease states via formulary restrictions.
What is a formulary product?
A formulary is the list of generic and brand-name prescription drugs covered by a specific health insurance plan. Sometimes, health plan formularies are also referred to as preferred drug lists (PDLs).
What is the difference between formulary and non formulary drugs?
A drug formulary is a listing of prescription medications in different categories that determines how much you will pay for the medication. If a medication is “non-formulary,” it means it is not included on the insurance company's “formulary” or list of covered medications.
What is formulary system?
A formulary system is the ongoing process through which a healthcare organization establishes policies regarding the use of drugs, therapies, and drug-related prod- ucts, including medication delivery devices, and identifies those that are most medically appropriate, safe, and cost-effective to best serve the health ...
What medication does Medicare not cover?
Medicare does not cover:Drugs used to treat anorexia, weight loss, or weight gain. ... Fertility drugs.Drugs used for cosmetic purposes or hair growth. ... Drugs that are only for the relief of cold or cough symptoms.Drugs used to treat erectile dysfunction.More items...
What does it mean if a drug is non-formulary?
Drugs that are usually considered non-formulary are ones that are not as cost effective and that usually have generic equivalents available.
Why are drugs removed from formulary?
Your health insurance plan's Pharmacy & Therapeutics Committee might exclude a drug from its drug formulary a few common reasons: The health plan wants you to use a different drug in that same therapeutic class. The drug is available over-the-counter. The drug hasn't been approved by the U.S. FDA or is experimental.
What is a formulary in Medicare?
The Medicare & You handbook defines a formulary as “a list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits.”. Most people simply refer to it as a drug list.
Why is formulary inclusive?
Cost savings is the reason a formulary inclusive of your medications is important. The drugs on these lists reflect those for which plans negotiate for the best price. The consequence of non-compliance with the list of covered drugs may result in your responsibility for full price versus a copayment or coinsurance.
What is Medicare Part D?
Medicare Part D is the prescription drug coverage for Medicare recipients. Part D plans are designed to defray the cost of your medications, but they do not kick in automatically when you enroll in Medicare Parts A and B. Once eligible, you would apply for the coverage through a private insurance company. Though all Part D plans are required ...
How long do you have to give a prescription drug plan to change the formulary?
Coverage rules and costs can change. Brand name drugs can be replaced by generic drugs. In these cases, the plan should give you at least 30 days of notice in writing before the effective date.
What to do if your insurance does not include your drug?
If the list of covered drugs does not include your specific drug, it will usually include one that is comparable. Consult with your physician in this case . If necessary, submit an exception request to your plan administrator.
How long do you have to give a drug plan before the effective date?
Brand name drugs can be replaced by generic drugs. In these cases, the plan should give you at least 30 days of notice in writing before the effective date. Sometimes, the Food and Drug Administration (FDA) decides certain drugs are unsafe.
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
What is a tier in prescription drug coverage?
Tiers. To lower costs, many plans offering prescription drug coverage place drugs into different “. tiers. Groups of drugs that have a different cost for each group. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. ” on their formularies. Each plan can divide its tiers in different ways.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
The basics
Navigating your health insurance coverage can feel like a drive through dense fog or heavy rain. It’s hard to see due to lack of clarity and visibility — especially when it comes to medication coverage. That’s why understanding your plan’s prescription drug formulary is critical on your journey to better health and saving money.
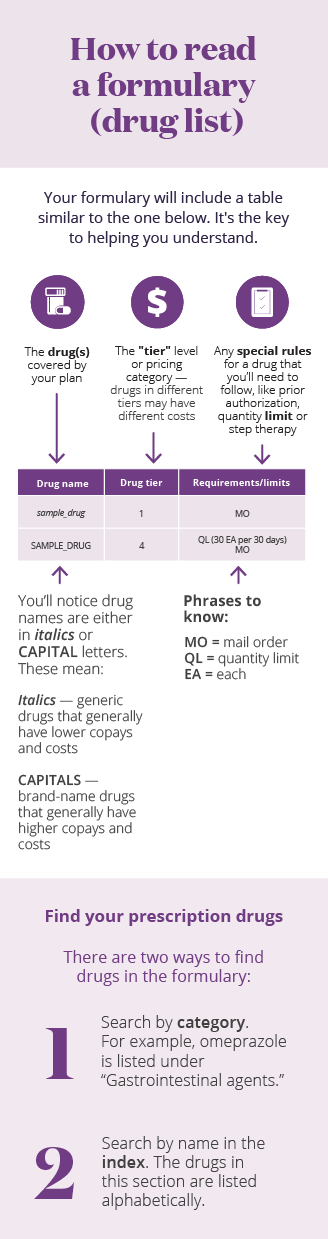
What is a drug formulary?
A formulary is a list of generic and brand name prescription drugs covered by your health plan. Your health plan may only help you pay for the drugs listed on its formulary. It’s their way of providing a wide range of effective medications at the lowest possible cost.
What is a tier?
Your health plan’s formulary is divided into three or four categories. These categories are called tiers. Drugs are placed in tiers based on the type of drug: generic, preferred brand, non-preferred brand, and specialty. Here’s what typical formulary tiers look like:
How are they created and why do they change?
Typically, a team of medical professionals approves the drugs on a health plan’s formulary based on safety, quality, and cost-effectiveness. The team is made up of pharmacists and physicians who review new and existing medications.
Can my healthcare provider access my formulary?
Yes and no. Many health plans share their formularies with healthcare providers. Others don’t, leaving it up to you to take your prescription needs into your own hands. Here’s what you can do:
What should I consider when choosing a health plan?
When shopping for a health plan, there’s a wide range of variables to consider. You may ask questions like, “Can I afford the monthly premium?” and “Can I continue to see my favorite healthcare provider?”
What is a formulary in Medicare?
A formulary is a list of prescription drugs covered by a plan. Because Medicare Part D is provided by private insurance companies such as Aetna and SilverScript, each company can decide which drugs to cover. However, a formulary must meet the minimum standards and requirements of Medicare Part D coverage. Do the drugs listed on a formulary change? ...
What are the tiers of a drug plan?
What are drug tiers? Formularies are set up in tiers. A drug in a lower tier usually costs less than a drug in a higher tier. Use a plan’s formulary to tell you which drugs are covered and which tier they are in. The tiers are numbered and include: Tier 1, Preferred Generic: These are commonly prescribed generic drugs.
What is Tier 4 drug?
Tier 4, Non-Preferred Drug: These are higher-priced brand-name and generic drugs, less commonly prescribed than drugs in the preferred tiers. Tier 5, Specialty: These are the most expensive drugs on the list. They may require special handling and/or close monitoring. Check our formulary.
Does Medicare Part D cover a drug?
Medicare Part D formularies are approved by Medicare and updated throughout the plan year, and may change if: The plan no longer covers a drug. A new drug is added. A drug is moved to a different cost-sharing tier. A prior authorization, step therapy restriction or quantity limit has been added or changed for a drug.
Does Medicare cover vitamins and minerals?
Prescription vitamins and minerals (some exceptions for drugs like fluoride preparations) Drugs when used for the treatment of sexual or erectile dysfunction (ED) In addition, Medicare Part D plans are unable to cover the following: Drugs that would be covered under Medicare Part A or Part B.