What does RAC stand for?
Recovery Audit Contractor (RAC) Recovery Audit Contractors (RAC) identify improper Medicare payments made on healthcare claims. These audits may result in the identification of Medicare overpayments and/or underpayments.
What is a Medicare RAC audit?
RAC audits are run by the Centers for Medicare and Medicaid Services (CMS). Their goal is to uncover improper Medicaid and Medicare claim payments and get the money back. RAC auditors have collected back over $2 billion for CMS.
What is a Recovery Audit Contractor (RAC)?
What does a Recovery Audit Contractor (RAC) do? RAC's review claims on a post-payment basis. The RAC's detect and correct past improper payments so that CMS and Carriers, FIs, and MACs can implement actions that will prevent future improper payments. Who are Recovery Audit Contractors?
What is the role of the RACS?
The RACs will detect and correct past improper payments so that CMS and the Carriers/FIs/MACs can implement actions that will prevent future improper payments yProviders can avoid submitting claims that don’t comply with Medicare rules

What is a RAC in Medicare?
What does a Recovery Audit Contractor (RAC) do? RAC's review claims on a post-payment basis. The RAC's detect and correct past improper payments so that CMS and Carriers, FIs, and MACs can implement actions that will prevent future improper payments.
What is a RAC letter?
If your practice receives a RAC audit notification letter, it's generally to investigate suspicion of an improper payment on a claim (either an overpayment or an underpayment). RAC auditors will usually request medical records to complete the audit.
What is the RAC process?
First, the RAC identifies a risk pool of claims. Second, the RAC requests medical records from the provider. Once the records are received by the RAC, they will review the claim and medical records. Based on the review, the RAC will make a determination: overpayment, underpayment or correct payment.
How are RACs paid?
RACs are paid on a contingency fee basis, which means they are reimbursed based on a percentage of the improper payments they find or collect. The amount of the contingency fee is based on the amount of money from, or reimbursed to, providers.
What is a RAC claim?
Recovery Audit Contractors (RAC) identify improper Medicare payments made on healthcare claims. These audits may result in the identification of Medicare overpayments and/or underpayments.
How far back can Medicare RAC audits go?
three yearsMedicare RACs perform audit and recovery activities on a postpayment basis, and claims are reviewable up to three years from the date the claim was filed.
What is the RAC appeal process?
There are three levels of appeal: Level I: Request for Reconsideration; Level II: Request for CMS Hearing Official Review; and Level III: Request for CMS Administrator Review. This page will assist you in understanding this process and how to file an appeal.
What triggers a Medicare audit?
What Triggers a Medicare Audit? A key factor that often triggers an audit is claiming reimbursement for a higher than usual frequency of services over a period of time compared to other health professionals who provide similar services.
What triggers a RAC audit?
RAC audits are not one-time or intermittent reviews and can be triggered by anything from an innocent documentation error to outright fraud. They are part of a systematic and concurrent operating process that ensures compliance with Medicare's clinical payment criteria, documentation and billing requirements.
How do I prepare for a RAC audit?
5 Ways You Can Begin Preparing for a RAC AuditPerform an Internal Audit. This action will help you to determine the likelihood of coding and billing mistakes within your company.Identify and Correct Coding/Billing Issues. ... Review Problem Areas. ... Check Documentation. ... Find Assistance.
How effective are recovery audit contractors?
Contingency Fees Based on Denial Overturn Rates For starters, RACs have an average accuracy rate of 96.4 percent and 3 out of 4 RACs have accuracy rates above 95 percent (one was over 99 percent accurate!).
How do I become a Medicare auditor?
The qualifications you need to become a Medicare auditor include a degree or equivalent experience and knowledge of Medicare rules and regulations. This career involves analyzing large amounts of information, so you need organizational and analytical skills.
What is Recovery Audit Contractor (RAC) Audit?
As a combined effort to fight fraud, waste, and abuse in the Medicare program, Recovery Audit Contractor (RAC) audit was in place from January 1, 2010. The goal of the recovery audit contractor program is to identify improper payments made on claims for services provided to Medicare beneficiaries.
The goal of the Recovery Audit Contractor (RAC)
As discussed above, RAC contractors are tasked with identifying improper payments made on claims of health care services provided to Medicare beneficiaries. Under most circumstances, the RAC will request medical records from the provider to determine whether overpayment and/or underpayment have occurred. Payments will be deemed improper when:
Filing an Appeal
The RAC Contractor has the ability to perform extrapolation based on improper payments identified during a review. If you receive an overpayment demand letter, and if you believe the request for overpayment is unjustified, you must file an appeal.
To summarize
Outsourcing Medical billing is complex, and your staff must be knowledgeable about many areas pertaining to billing and reimbursement. You have to establish compliance and practice standards and need to conduct internal monitoring and auditing to evaluate adherence.
What is Medicare Recovery Audit?
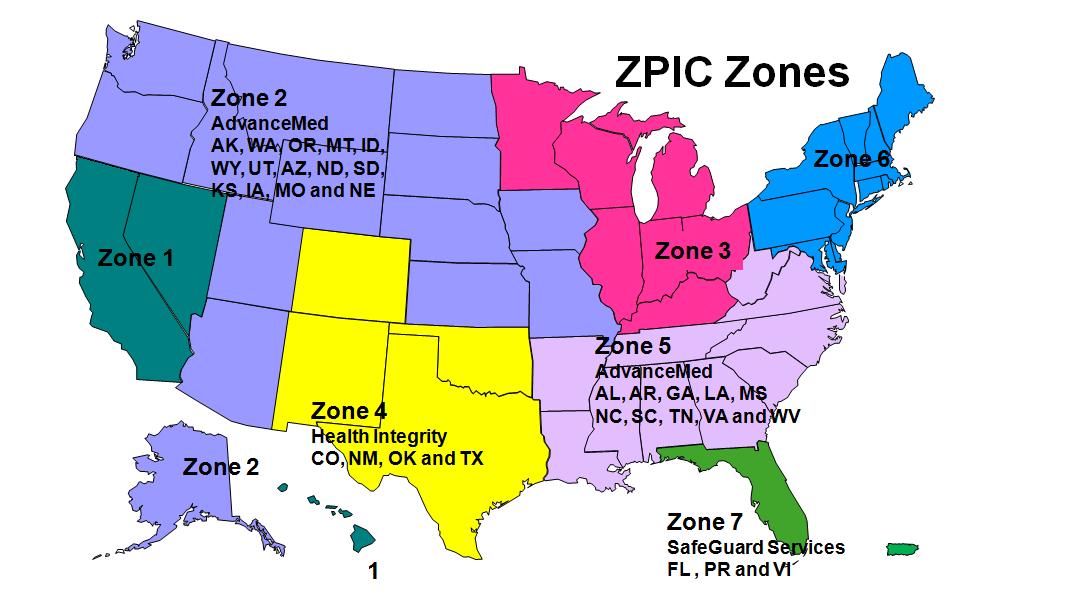
The Medicare Recovery Audit Program was designed to identify and reduce improper payments. Five RACs are each responsible for identifying overpayments and underpayments in approximately one quarter of the country, divided geographically.
Do RACs have to return fees?
The RACs must return the fee if an overpayment/underpayment is overturned at any level of appeal. The RACs offer a period of discussion to allow providers the opportunity to discuss or submit additional documentation prior to initiating the appeals process.
Introduction: What is a RAC Audit?
Medicare Recovery Audit Contractor Audits (RACs, or RAs) were introduced beginning in 2005 to identify and recover improper payments made in Medicare and Medicaid transactions between providers and payors. They were (and are) conducted by Recovery Audit Contractors (also known as RACs).
Chapter One: History of Recovery Audits
RAC audits were introduced in 2005, peaked around 2010 and experienced a slowdown from that point on. To understand the role of RAC audits in today’s healthcare finance space, it’s important to know how they started and why they have diminished.
Chapter Two: Types of RAC Audits
Before we look at the specific types of Recovery Audit Contractor audits, let’s review where they lie in the overall audit landscape.
Chapter Three: RAC Audit FAQ
With so many levels and types, it’s clear that audits can be complex. Adding in government legislation doesn’t necessarily make the process easier. The following frequently asked questions can provide additional clarity on the why and how of RAC audits.
Chapter Four: The Audit Process
The timing of an audit is dependent entirely upon the payor. If a RAC auditor wishes to conduct an audit, the provider must comply. Once an audit begins, the initial response process is largely the same regardless of whether it was triggered by a RAC auditor, commercial payor or other audit contractors.
Chapter Five: What Can You Do To Improve Your RAC Audit Process?
Before the ADR even arrives on your doorstep, you can take steps to train your team and implement processes designed to simplify your response process.
Chapter Six: Technology as an Audit Management Solution
When RAC audits were introduced, providers received an unmanageable volume of audit requests from payors. Now, changes in Recovery Audits have led to fewer audits and less paperwork, giving hospitals the opportunity to focus more broadly on all types of payor audits.
What are the two types of Medicare RAC audits?
Types of RAC Audits. Generally, there are two types of Medicare RAC audits – the automated audits and complex audits.
What is RAC audit?
What Are Recovery Audit Contractor (RAC) Audits? Also known as a Medicare audit or a MAC audit, the Recovery Audits Contract (RAC) program is an aggressive campaign seeking reimbursement from healthcare service providers. These audits have become increasingly frequent over the past few years, and they will continue to for the foreseeable future.
What is Medicare Recovery Audit Contractor?
These include services that are deemed “not reasonably necessary.”
What to do if you are subject to a RAC audit?
If you are subject to a RAC audit, make sure to make an informed decision selecting an attorney. You’ll need an experienced team well versed in this subject to effectively refute fraud claims, especially in complex RAC audits.
Is CMS still enforcing Medicare RAC audits?
All in all, the CMS is expected to continue enforcing standards for payments and Medicare RAC audits. Healthcare service providers will also be looking to minimize the risk that the Medicare recovery audit contractor program can have on them, both from a financial and reputational perspective.
What does RAC audit notification mean?
If your practice receives a RAC audit notification letter, it’s generally to investigate suspicion of an improper payment on a claim (either an overpayment or an underpayment). RAC auditors will usually request medical records to complete the audit.
How long does it take for RAC to determine if you have overpaid?
Once you submit the requested medical records, the RAC has 60 days to get a determination to you. If all goes well, this could be the end of the audit. If the RAC determines you received an overpayment, the process will continue, and you could be required to pay the money back.
How long does it take to get an overpayment letter from the RAC?
After receiving a demand letter, you are required to call the RAC within 15 days to discuss how you plan to proceed. In response to an overpayment demand letter, you essentially have three options:
How long do you have to respond to a RAC request?
If you receive a letter from a RAC contractor requesting medical records, don’t delay. You have 45 calendar days to either submit a response or file an extension. If you don’t respond at all, the RAC could simply make a determination that you were overpaid, and take their money back.
How long does it take to get a Medicare recoupment determination?
Level 1: The first appeal level is redetermination. You have 120 days to file the first appeal but if you get it in within 30 days you can avoid Medicare recoupment action. You should get a determination within 60 days of receipt of your redetermination request. Level 2: The second appeal level is reconsideration.