How long to keep Medicare summary notices?
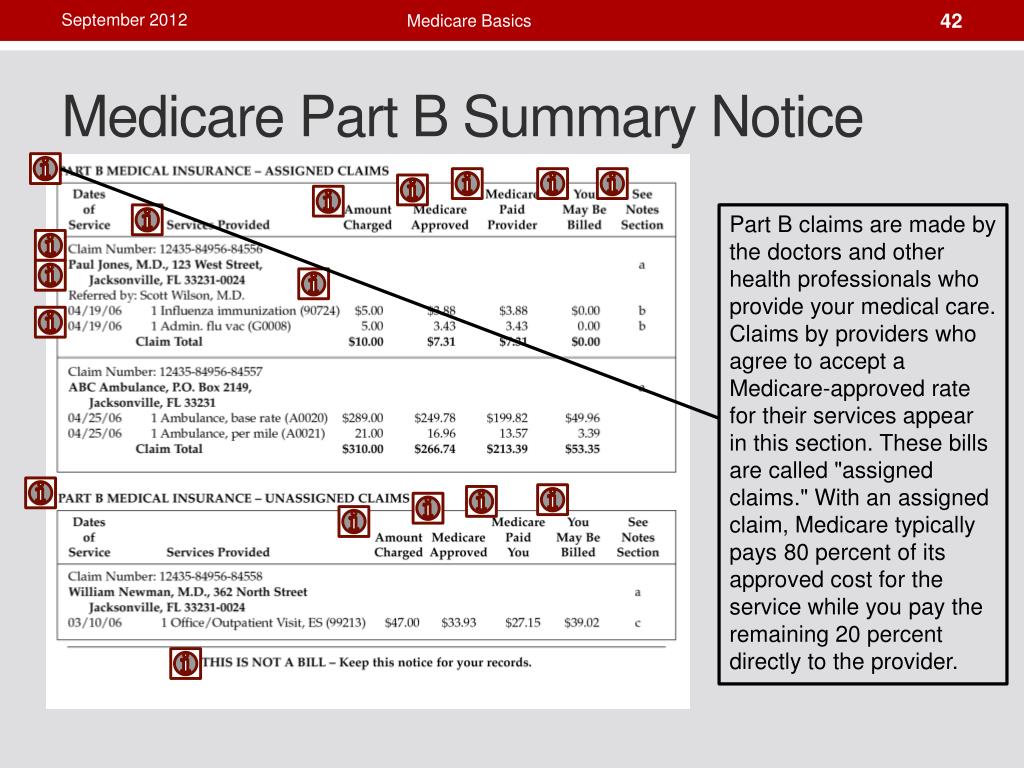
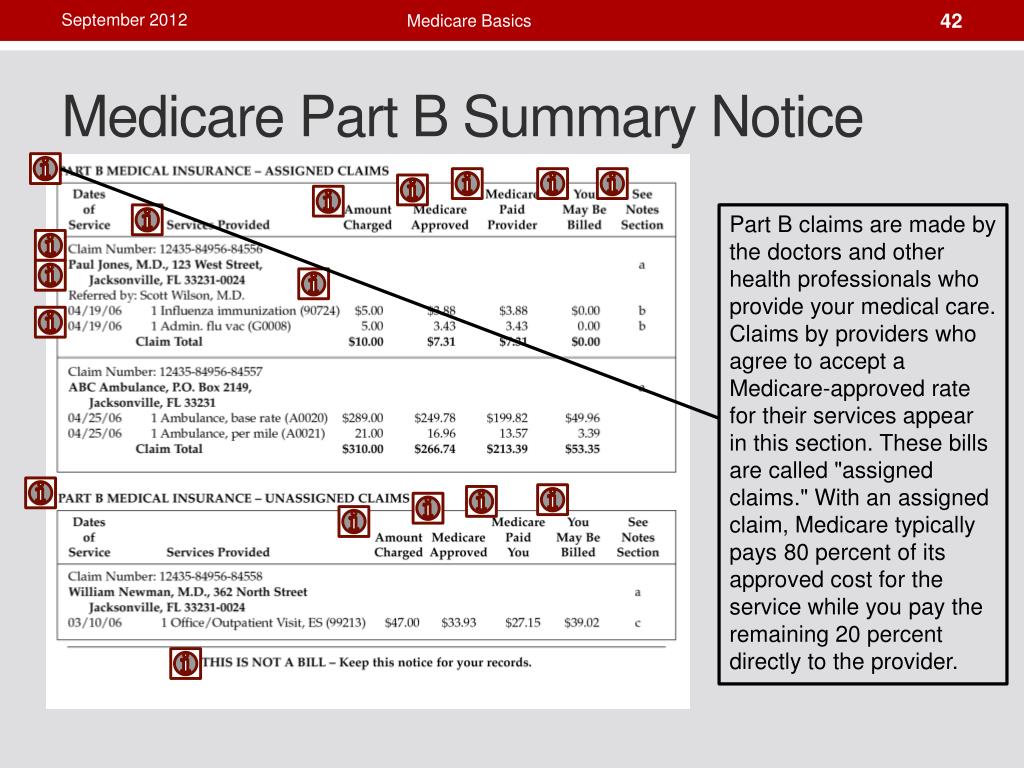
Mar 08, 2022 · The Medicare Summary Notice (MSN) is used to notify beneficiaries of decisions on claims for Medicare benefits. MSN Messages Messages are printed on the MSN to explain both general and claims-specific information to beneficiaries.
How to understand Medicare summary notices?
The Medicare Summary Notice (MSN) is a notice that Medicare sends out every three months to people with Original Medicare (Part A and/or Part B). It outlines: It outlines: All services and supplies that providers/suppliers billed to Medicare during the …
How to read your Medicare summary Notice (MSN)?
The Medicare Summary Notice, also called an MSN, is a report of doctor visits, services or supplies billed to Medicare in your name. It is mailed every 3 months and is also available online. The MSN explains the charges that will be paid by Medicare and those that will be paid by you or other insurance (like Medigap or employer insurance).
What is a concern about the future of Medicare?
The Medicare Summary Notice (MSN) is a summary of health care services and items you have received during the previous three months. The MSN is not a bill. The MSN is not a bill. The contractor that processes your claims for Medicare will send you the MSN, so it may have the name and address of a private company on it.
What is the purpose of the Medicare Summary Notice?
Medicare Summary Notice. A Medicare summary notice is a claims statement you receive in the mail from Medicare every three months. It contains information about the services you received, explains the charges Medicare will pay and states the maximum amount you may owe.
Is it necessary to keep Medicare summary notices?
Medicare rules require all claims for services be filed with Medicare within one calendar year after the date of service. Keeping your MSNs for at least one year allows you to monitor Medicare's payment activity. You may also monitor your MSNs by logging onto mymedicare.gov.Sep 30, 2012
How do I get a Medicare Summary Notice?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage. You'll come to the "My communication preferences" page where you can select "Yes" under "Change eMSN preference," then "Submit."
Is a Medicare Summary Notice the same as an EOB?
An EOB is not the same as a Medicare Summary Notice. It is also important to remember that an EOB is not a bill. EOBs are usually mailed once per month. Some plans give you the option of accessing your EOB online.
How often does Medicare mail Paper Summary Medicare notices?
You'll get your MSN every 3 months if you get any services or medical supplies during that 3-month period.
How often are Medicare summary notices mailed?
four times a yearMSNs are usually mailed four times a year (quarterly) and contain information about charges billed to Medicare, the amount that Medicare paid, and the amount you are responsible for. Note that you may receive additional MSNs if you receive reimbursement for a bill you paid.
How do I get my Medicare explanation of benefits?
claims:Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. ... Use Medicare's Blue Button by logging into your secure Medicare account to download and save your Part D claims information. ... For more up-to-date Part D claims information, contact your plan.
Does Medicare send a year end statement?
A Medicare benefit tax statement is mailed each year between December and January. It shows Medicare Part A as qualifying healthcare coverage, meaning Part A meets the Affordable Care Act rules for health insurance.Aug 31, 2020
Can you go paperless with Medicare?
Medicare has been improving its paperless billing options, and you can now choose to receive your Medicare Summary Notices and the Medicare & You handbook electronically.
How do I get an explanation of benefits?
After you visit your provider, you may receive an Explanations of Benefits (EOB) from your insurer. This is an overview of the total charges for your visit and how much you and your health plan will have to pay. An EOB is NOT A BILL and helps to make sure that only you and your family are using your coverage.
How long should you keep Medicare explanation of benefits?
Unlike medical bills, EOBs should be kept from three to eight years after your procedure, or indefinitely if you have a reoccurring condition.Oct 4, 2019
How do I know what Medicare has paid?
You can also contact your local Health Insurance Counseling & Advocacy Program (HICAP) office online or at 1-800-434-0222. You will also receive an Explanation of Benefits (EOB) from your Medigap company or retiree plan. The EOB will show you how much was paid.
What is Medicare Summary Notice?
The Medicare Summary Notice contains a summary of your benefits for Medicare, including Part A, Part B and Part C. In mid-2013, the federal government redesigned the Medicare Summary Notice. Based on the results of a study of Medicare recipients, several changes were made that make the MSN easier to read and understand.
How to report Medicare fraud?
If you suspect a charge you find on your MSN to be in error or fraudulent, first, report the error to your medical service provider. If the issue is not resolved by contacting your provider, contact a member of the Medicare support staff at (800) MEDICARE (633-4227).
What to do if you are not covered by Medicare?
If there are charges that are not covered by Medicare listed on the MSN, and you believe these charges should be covered, contact your healthcare provider’s office. Billing personnel can assist you with your questions about qualified charges. 1.)
Can you appeal a denied claim on Medicare?
1.) If you received a service from your healthcare provider, and the claim was denied by Medicare as an unnecessary service, you can appeal this decision . 2.) If you or your doctor has made a specific request for a healthcare service or product, you can appeal this decision.
What is the MSN statement?
And, MSN statements include definitions and clear instructions for procedures and descriptions; they’re provided in large type, as well.
How to review MSN?
To review your MSN, first , gather all receipts and paperwork from any healthcare services you have recently received. Next, sit down with the paperwork and the MSN and compare codes and charges. The charges and codes, though they may not be identical, should be similar enough to understand if the charge is valid.
Is MSN a bill?
The MSN is a not a bill to you, but you should spend some time reviewing the information, nonetheless. The MSN statement can provide you with the information to track your out-of-pocket charges for health services. Additionally, you can help combat fraud and catch errors by carefully reviewing your MSN.
What is Medicare Summary Notice?
To help, Medicare provides statements known as Medicare Summary Notices (MSN) to help you stay on top of your account. If you or a loved one are trying to make sense of your MSN, here’s an easy-to-follow guide.
What is Medicare Original?
Original Medicare is a fee-for-service health insurance program available to Americans aged 65 and older and some individuals with disabilities. Original Medicare is provided by the federal government and is made up of two parts: Part A (hospital insurance) and Part B (medical insurance). account. Each MSN includes instructions to file an appeal ...
Does Medicare Advantage have an EOB?
Private health insurance companies provide Medicare Advantage and Part D plans, and each company creates its own EOB to send to its customers. That means an EOB from one company can look very different from another company’s EOB. MSNs, however, are all formatted the same way.
Is Medicare Supplement endorsed by the government?
Medicare Supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. Our mission is to help every American get better health insurance and save money. If you’re looking for the government’s Medicare site, please navigate to www.medicare.gov.
Is MSN a bill?
An MSN is not a bill. Think of your MSNs as Medicare statements. As with your bank statements, you can use an MSN to verify that your account’s activity matches the services you received.
Medicare Summary Notice
Your Medicare Summary Notice is a basic report of all of the visits to your doctor, medical services, or supplies that have been billed to Medicare in your name. Your Medicare Summary notice is mailed to you every three months and it’s a great piece of information for you to review.
What is listed on the MSM?
The MSM lists more than just the health care services you received in the past 3 months.
can i get my medicare summary notice online?
Yes you can. Your MSM is available online at MyMedicare.gov. You’ll be able to login and see the charges that are going to be paid by Medicare as well as the charges that you’re responsible for (or your supplemental insurance if you have a separate plan).
What if a service was denied?
If you see that a service or item has been denied, contact your doctor or other health care provider and make sure that they have submitted the information correctly. If they haven’t, the doctor’s office can resubmit.
how long should i keep medicare summary notices?
Holding on to your MSNs for at least 12 months is a good rule of thumb. It allows you to keep track of Medicare’s payment activity. The main reason to save your MSM for 1 year is because Medicare requires that all claims for health care services need to be filed with Medicare within 12 months after the date of service.
