
Full Answer
What are the different prospective payment systems?
What is a Prospective Payment System?
- Comparing the PPS Payment System. Although the PPS payment system may sound somewhat like a health maintenance organization (HMO), there are differences.
- PPS Classifications. PPS determines payment based on a classification of service. ...
- PPS Payment Adjustments. ...
- From Volume to Value. ...
What is an example of a prospective payment system?
Skilled nursing facilities (SNFs) that provide services—including audiology and speech-language pathology services—to Medicare beneficiaries are paid under a prospective payment system (PPS) through Part A of the Medicare benefit.
What does prospective payment system mean?
The prospective payment system (PPS) is defined as Medicare’s predetermined pricing structure to pay for medical treatment and services. An example of the prospective payment system is the amount a hospital will be reimbursed for an MRI for a Medicare patient. noun.
What is it the payment for the prospective payment system?
Prospective Payment System: A healthcare payment system used by the federal government since 1983 for reimbursing healthcare providers/agencies for medical care provided to Medicare and Medicaid participants. The payment is fixed and based on the operating costs of the patient’s diagnosis.

What is a prospective payment system for Medicare patients?
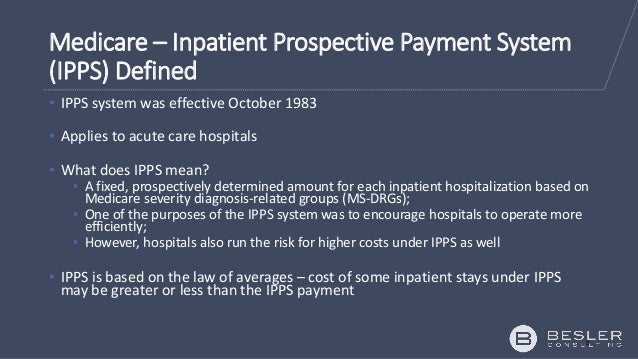
A Prospective Payment System (PPS) is a method of reimbursement in which Medicare payment is made based on a predetermined, fixed amount. The payment amount for a particular service is derived based on the classification system of that service (for example, diagnosis-related groups for inpatient hospital services).
Why did Medicare move to a prospective payment system?
The idea was to encourage hospitals to lower their prices for expensive hospital care. In 2000, CMS changed the reimbursement system for outpatient care at Federally Qualified Health Centers (FQHCs) to include a prospective payment system for Medicaid and Medicare.
What is the purpose of prospective payment system?
PPS is intended to motivate healthcare providers to structure cost-effective, efficient patient care that avoids unnecessary services. The goal is to provide quality patient care that engages patients, and strives for faster diagnosis and treatment, shorter hospital stays, and lower costs.
What's a prospective payment system for Medicare patients quizlet?
When a health care facility provides services to a patient fully expecting to be paid but the payer does not pay, the amount for the service is charged off to this account. A specific patient condition that is secondary to a patient's principal diagnosis.
When did Medicare Move to prospective payment system?
1986By fiscal year 1986, 48 States and the District of Columbia were under prospective payment, including some 84 percent of all Medicare participating hospitals. In addition, Puerto Rico was brought under the nationwide system in fiscal year 1988.
What are the different types of prospective payment systems?
The PPS is the DRG. The DRG is based on the patient diagnosis. The DRG payment is per stay. The amount of reimbursement is based on the relative weight of the DRG....HospiceRoutine home care.Continuous home care.Inpatient respite care.General inpatient care.
Is prospective payment system good or bad?
Key Findings Medicare's prospective payment system (PPS) did not lead to significant declines in the quality of hospital care. Mortality rates declined for all patient groups examined, and other outcome measures also showed improvement.
What are the disadvantages of a prospective payment system?
Prospective payment plans also come with drawbacks. Because providers only receive fixed rates, some might seek to employ cost-cutting measures to maximize profits while not necessarily keeping their patients' best interests in mind.
What was the impact of the Medicare prospective payment system on healthcare and hospitals?
Under this system, hospitals were paid whatever they spent; there was little incentive to control costs, because higher costs brought about higher levels of reimbursement. Partly as a result of this system of incentives, hospital costs increased at a rate much higher than the overall rate of inflation.
What is the prospective payment system quizlet?
Under the prospective payment system (PPS), hospitals are paid a set fee for treating patients in a single DRG category, regardless of the actual cost of care for the individual.
What does PPS stand for quizlet?
What does "PPS" stand for? Prospective payment system.
When was the first prospective payment system established?
October, 1983Introduction. The Medicare Inpatient Prospective Payment System ( IPPS ) was introduced by the federal government in October, 1983, as a way to change hospital behavior through financial incentives that encourage more cost-efficient management of medical care.
What is the prospective per diem rate for Medicare?
The prospective rate is based upon a case-mix system, with the reimbursement premised upon measuring the type and intensity of the care required by each resident and the amount of resources which are utilized to provide the care required.
Why are SNFs reluctant to accept Medicare?
Many SNFs have informally communicated a reluctance to accept such individuals when Medicare is the apparent payment source, because of the costs involved. As a result, it appears that individuals who have these needs encounter difficulties to obtaining SNF placement.
What are the most critical nursing activities that can invoke Medicare coverage?
Three of the most critical nursing activities that can invoke Medicare coverage included in the administrative criteria are as follows: 1. Overall management and evaluation of an individual's care plan ( 42 CFR 409.33 (a) (1)); 2. Observation and assessment of the patient's changing condition.
When did nursing homes get reimbursed?
Until July, 1998, nursing homes used to be reimbursed for care provided to Medicare Part A-covered residents residing in Medicare-certified beds through a retrospective cost-based system. The rate received by a nursing home for a Medicare covered resident was based on three components:
Is physical therapy covered by Medicare?
Physical therapy, for example, was covered separately by Medicare based upon a determination regarding medical necessity . There was, therefore, a fiscal incentive for nursing homes to provide such therapy to Medicare Part A covered residents; Capital costs: costs of land, buildings and equipment.
What is a prospective payment system?
Prospective Payment Systems (PPS) was established by the Centers for Medicare and Medicaid Services (CMS). PPS refers to a fixed healthcare payment system. This is based on the operating and capital-related costs of a medical diagnosis and determines reimbursement for care provided to Medicare and Medicaid participants.
What is PPS in Medicare?
Instead of a monthly payment amount for all services, like an HMO provides, PPS provides the healthcare facility with a single predetermined payment for each Medicare patient. This prepayment is based on the patient diagnosis and standardized assessments and covers a defined time such as an inpatient hospital stay, or a 60-day Home Health episode.
What is PPS in home health?
Home Health PPS classifications are based on Home Health Resource Groups (HHRG) determined by the Outcome and Assessment Information Set (OASIS). Medicare pays a predetermined base rate that is adjusted based on the patient’s health condition and service needs, which is considered the case-mix adjustment.
Zipcode to Carrier Locality File
This file is primarily intended to map Zip Codes to CMS carriers and localities. This file will also map Zip Codes to their State. In addition, this file contains an urban, rural or a low density (qualified) area Zip Code indicator.
Provider Center
For a one-stop resource web page focused on the informational needs and interests of Medicare Fee-for-Service (FFS) providers, including physicians, other practitioners and suppliers, go to the Provider Center (see under "Related Links" below).
How many days does Medicare cover?
Medicare allows 90 covered benefit days for an episode of care under the inpatient hospital benefit. Each patient has an additional 60 lifetime reserve days. The patient may use these lifetime reserve days to cover additional non-covered days of an episode of care exceeding 90 days. High Cost Outlier.
How long does Medicare cover inpatient hospital care?
The inpatient hospital benefit covers 90 days of care per episode of illness with an additional 60-day lifetime reserve.
When does home health care begin?
Home health care, when the patient gets clinically related care that begins within 3 days after a hospital stay. Rehabilitation distinct part units located in an acute care hospital or a CAH. Psychiatric distinct part units located in an acute care hospital or a CAH. Cancer hospitals.
What is a physician order?
The physician order meets 42 CFR Section 412.3 (b), which states: A qualified, licensed physician must order the patient’s admission and have admitting privileges at the hospital as permitted by state law. The physician is knowledgeable about the patient’s hospital course, medical plan of care, and current condition.
Comparing The PPS Payment System
PPS Classifications
- PPS determines payment based on a classification of service. For example, for inpatient hospital services, CMS uses separate PPSs for reimbursement related to diagnosis-related groups (DRGs). This patient classification method indicates groups of patients that would incur similar resource consumption, length of stay, and the costs generally incurred with this diagnosis to classify inpa…
PPS Payment Adjustments
- There is a potential for add-on payment adjustments for PPS classifications. Payment adjustments can be based on area wage adjustments, outliers in cost, disproportionate share adjustments, DRG weights, case mix and geographic variation in wages. Hospitals may be eligible for an add-on payment if they are considered a disproportionate share hospital (DSH), in that the…
from Volume to Value
- PPS continues to focus on many of the principles of value-based care. To continue the shift from fee-for-service care, healthcare providers are striving to optimize technologyto increase their productivity. This may assist in the shift from volume to value, and support incentives for the provision of quality, holistic, preventative patient care. DUMMYTEXT Article Sources 1. 2018 Wh…