Original Medicare & Coverage for Cataract Surgery Medicare is a health insurance program in place for Americans 65 years old and up, or for those with special qualifying circumstances or health conditions. Estimates show 10,000 people turn 65 every day, making them eligible to receive Medicare benefits.
Full Answer
Does Medicare cover prescription drugs after cataract surgery?
If a person with a Part D plan needs a prescription drug to take at home following cataract surgery, their plan will likely cover part of the cost. Medicare supplement plans, also known as Medigap plans, are private insurance policies that help people pay the 20% of costs excluded from Medicare coverage.
How much does cataract surgery cost on Medicare in 2020?
In 2020, the Part A deductible is $1,408, so keep that in mind if you get your surgery done in a hospital. Part B covers your outpatient care and is most likely what you will use to cover your cataract surgery.
Is your dispensary Medicare compliant for post-cataract eye care?
Make sure your dispensary is compliant with Medicare payment rules for post-cataract eyeglasses. Otherwise, you could be losing out on eyewear revenue and fully caring for your patients. You may already know this, but it’s worth emphasizing: Medicare does not cover refractions, eyeglasses, or contact lenses for beneficiaries.
When is a cataract attestation indicated?
When one or more concomitant ocular diseases are present that potentially affect visual function (e.g., macular degeneration or diabetic retinopathy), the attestation should indicate that cataract is believed to be significantly contributing to the patient’s visual impairment.

What is the criteria for Medicare to pay for cataract surgery?
How do I qualify? If you're 65-or older and your doctor has determined surgery for your cataracts to be medically necessary, Medicare will typically cover 80% of your expenses including post-surgery eyeglasses or contacts.
Does Medicare have to approve cataract surgery?
In general, Medicare covers traditional cataract surgeries if they are medically necessary and the treating doctor accepts Medicare for payment. About 50% of adults have cataracts or have undergone cataract surgery by the time they reach 80 years of age.
What is the criteria for cataract surgery?
Cataract surgery is considered “medically necessary” by some insurance companies (like Medicare) only when certain conditions are met. The service is often covered only after a cataract has caused visual acuity to be reduced to below 20/40 — the legal vision requirement for driving in most states.
Is cataract surgery considered pre-existing condition?
The court also rejected Unum's argument that the surgery for the right eye cataract “initiated the causal chain.” The court remarked: “The surgery cannot be a pre-existing condition; it is at most only a necessary consequence of the right-eye cataract pre-existing condition.” Moreover, the court found the anisometropia ...
Does Medicare A and B cover cataract surgery?
Cataract surgery is covered by Medicare when your medical provider performs the procedure using traditional surgical techniques or lasers. If your treatment includes laser surgery, premium lenses, and/or multifocal lenses, you could incur higher out-of-pocket costs.
How Much Does Medicare pay for cataract surgery in 2022?
Original Medicare Cataract Surgery Coverage Most cataract surgeries are performed in outpatient settings. Medicare covers 80 percent of the Medicare-approved costs for these medical services. You are responsible for the remaining 20 percent, plus your Part B deductible ($233 in 2022).
Why is cataract surgery considered elective?
Elective surgery includes procedures that are completely your choice to have or not to have; cosmetic procedures and even something like LASIK. In contrast, while considered elective and scheduled in advance, something like cataract surgery can be regarded as both urgent and necessary.
Who Cannot have cataract surgery?
For example, if you have advanced macular degeneration or a detached retina as well as cataracts, it's possible that removing the cataract and replacing it with a clear intraocular lens (IOL) might not improve your eyesight. In such cases, cataract surgery may not be recommended.
What qualifies as a pre-existing condition?
As defined most simply, a pre-existing condition is any health condition that a person has prior to enrolling in health coverage. A pre-existing condition could be known to the person – for example, if she knows she is pregnant already.
Can you be denied coverage for a pre-existing condition?
Health insurance companies cannot refuse coverage or charge you more just because you have a “pre-existing condition” — that is, a health problem you had before the date that new health coverage starts.
Is cataract surgery vision or medical?
Medicare, Medicaid and most private insurance programs deem cataract surgery to be “medically necessary,” assuming the development of the cataract (or cataracts) is such that it interferes with the patient's normal daily activities.
What percent of cataract surgery is covered by Medicare?
In fact, eighty percent of cataract surgery in the US is performed on Medicare beneficiaries! Here’s what else you need to know about Medicare coverage of cataract surgery.
What is the Medicare Part B for cataract surgery?
In general, Medicare Part B (Medical Insurance) covers the costs associated with cataract surgery including the pre-surgery exam where you discuss your cataracts and any post-surgery care as well as ophthalmologist and facility fees.
Does Medicare cover eyeglasses?
Although Original Medicare doesn’t cover vision exams – such as if you need everyday prescription glasses – it will cover one pair of eyeglasses or contact lenses after cataract surgery of an implanted intraocular lens (IOL).
Do you need glasses after cataract surgery?
Not everyone needs glasses after cataract surgery , but if you need post-cataract glasses for reading and other close-up tasks, you pay 20% of the Medicare-approved amount and Medicare Part B will pay for the contact lenses or eyeglasses from a supplier enrolled in Medicare.
Does Medicare cover laser cataract surgery?
While this newer laser technology may have certain benefits, such as greater accuracy, it may not necessarily be an improvement in safety and visual outcome for everyone. However, whether you and your ophthalmologist select laser-assisted cataract surgery (LACS) or phacoemulsification, Medicare will cover either.
General Information
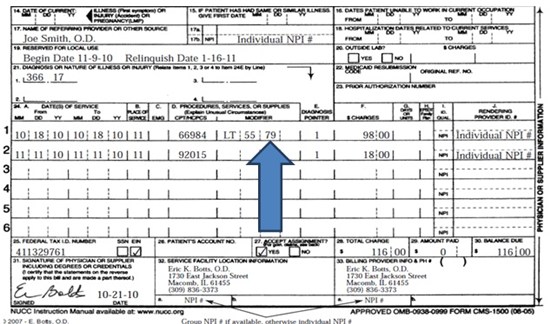
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act §1862 (a) (7) excludes routine physical examinations.
Article Guidance
Documentation Requirements: The following documentation must be present in the medical chart: For Visually-Symptomatic Cataract:
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
How Can I Know if My Lens Implant is Covered?
There are multiple types of cataract surgeries, and some of the more complex or involved procedures that will not be covered by Original Medicare. With most cataract surgeries, the type of lens that is used is called a monofocal lens. It is important to note that Medicare will only cover monofocal lens implants.
Cataract Surgery: Is it Medically Necessary?
Medicare will only cover your cataract surgery if it is deemed as being medically necessary. In the majority of instances, procedures like cataract surgery will be deemed medically necessary. However, it will be useful to make sure that this is the case before you proceed with the surgery.
Which Parts of Medicare Do You Need For Cataract Surgery?
Medicare is divided into various parts, each of which covers different types of services. Cataract surgery, like many surgeries, can be done in an outpatient setting or a hospital, and can also involve additional follow-up services and prescription drugs.
What Next?
In general, cataract surgery is fairly simple when it comes to Medicare coverage. This is because the coverage provided is consistent, and most people will be covered comprehensively with just their basic Original Medicare.
Does Medicare Advantage cover cataract surgery?
Does Medicare cover cataract surgery? Original Medicare will cover the removal of a cataract and lens implantation. Depending on how the procedure is done, different parts of Medicare will cover the surgery.
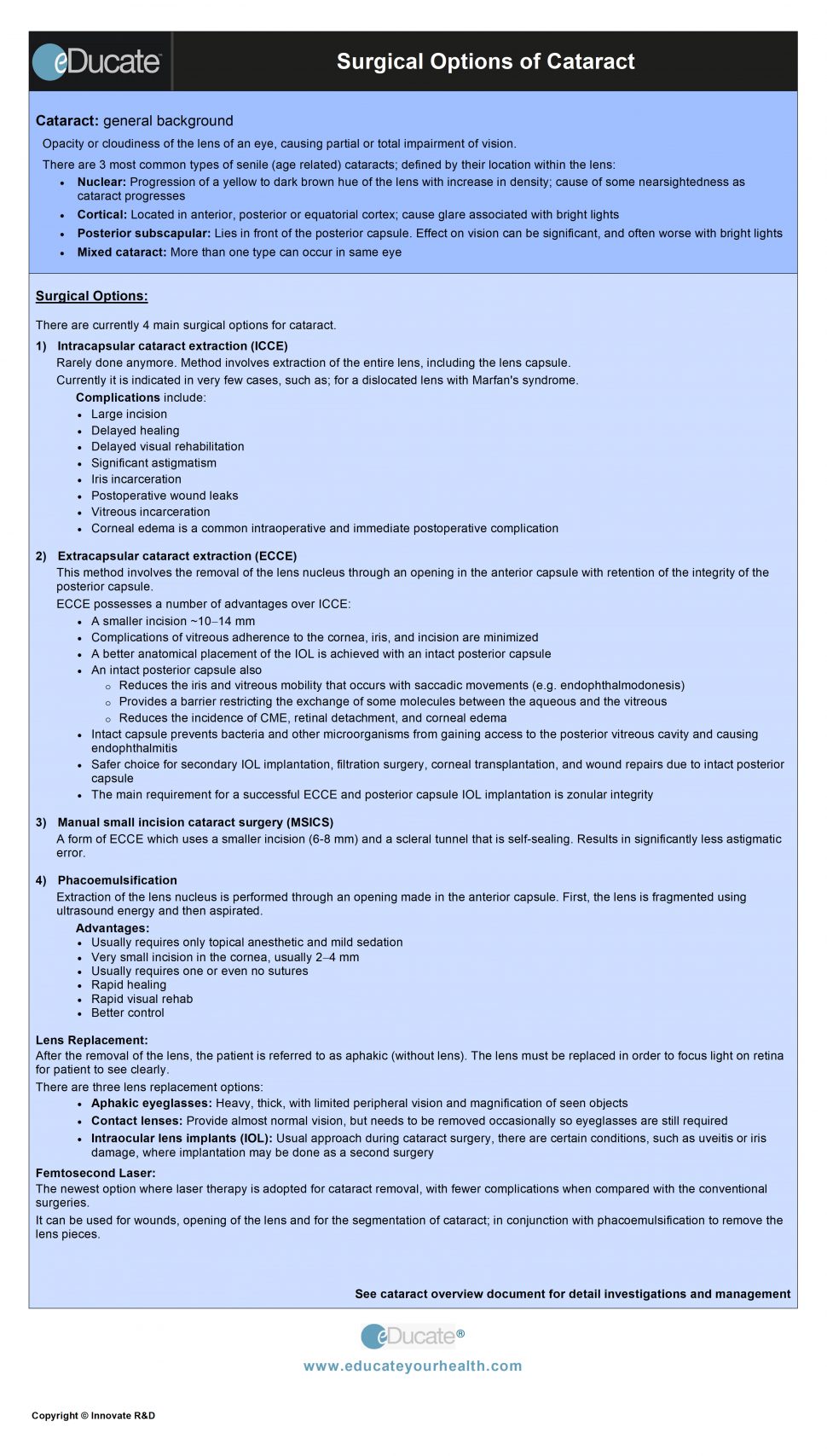
What is a cataract and cataract surgery?
A cataract occurs when the clear lens of your eye becomes cloudy or stiff. Some symptoms of a cataract may include cloudy or blurred vision, faded colors, double vision, difficult seeing in the dark, sensitivity to bright lights, and changes in vision.
How much does cataract surgery cost?
Does Medicare pay for cataract surgery? There are a few different factors that affect how much a cataract surgery costs. If you get your cataract surgery done in a surgery center or clinic, the total cost may be around $977. Medicare would pay $781, and you would have to pay $195.
Does Medicare cover glasses or other vision services?
Does Medicare pay for glasses? Medicare coverage for cataract surgery includes one pair of eyeglasses or contact lenses after the procedure. However, you may end up paying 20% out of pocket, and they must be provided by a Medicare-approved doctor.
Does Medicare cover glasses after second eye surgery?
What actually happens is that Medicare covers just one pair of glasses or contacts after the second surgery, says Tracy Holt, MHR, COPC, transformational services account manager for Eye Care Leaders.
Does Medicare cover eyeglasses?
Medicare will rarely cover tint, oversize lenses, A/R coating, polycarbonate, or high index, she adds. So does Medicare also pay for the eye exam? No. Medicare does not cover routine eye exams/refractions for eyeglasses or contact lenses.
Does Medicare cover cataract surgery?
Medicare Coverage of Post-Cataract Eyeglasses, Explained. You may already know this, but it’s worth emphasizing: Medicare does not cover refractions, eyeglasses, or contact lenses for beneficiaries. The exception is for post-cataract surgery or in cases when surgery results in the removal of the eye’s natural lens.
Can you collect from a patient for cataract eyewear?
You can collect directly from the patient for these items. To do that compliantly and to collect your full reimbursement, you’ll need to provide and have the patient sign an advance beneficiary notice of non-coverage (ABN) before you deliver the post-cataract eyewear. The ABN is CMS-required form, mandated by HIPAA.
How much does cataract surgery cost?
for one eye and slightly over $5,200 for two eyes. However, the cost of cataract surgery can vary among states and individuals. For example, it may cost more depending on the type of procedure a person undergoes and whether the surgery takes place at an outpatient surgical center or a hospital.
What is Medicare Advantage?
Medicare Advantage, or Medicare Part C, plans are the alternative to traditional Medicare. Because of this, they need to provide at least the same coverage for everything, including cataract surgery. Medicare Part D is a prescription drug plan available to people who have Medicare parts A and B.
Why do cataracts occur?
According to the American Academy of Ophthalmology, aging is the most common cause of cataracts. Normal proteins in the lens start to break down as a person becomes older. Over time, this breakdown causes cloudiness in the lens, which can interfere with vision. As of 2015, researchers estimate that about 3.6 million.
Does Medicare cover glasses?
Usually, Medicare pays 80% of the total surgical cost, consisting of the procedure itself and the facility charges. Medicare does not normally cover prescription glasses. The exception is one pair of spectacles or contact lenses after cataract surgery. The plan covers the following services:
Does Medicare cover intraocular lenses?
During cataract surgery, a surgeon inserts a type of lens called an intraocular lens (IOL). However, Medicare may not cover all types of IOL. It does pay for monofocal lenses, however, which surgeons typically use. Although other lenses, including multifocal and toric lenses, are available, Medicare may not cover these.
Does Medicare cover cataract surgery?
Although Medicare usually covers cataract surgery that a doctor deems medically necessary, the requirements for coverage vary between regions. Before undergoing the procedure, a person may wish to check the regulations of their local Medicare carrier. Medicare does not cover the remaining 20% of the cost of cataract surgery.