How to become Medicare certified?
- Provide Skilled Nursing services and other therapeutic services
- These services are supervised by a physician or RN
- Have established policies & procedures
- Maintain clinical records on all patients
- Have an overall plan and budget
- Meet the Medicare Conditions of Participation (CoPs)
- Meet capitalization requirements
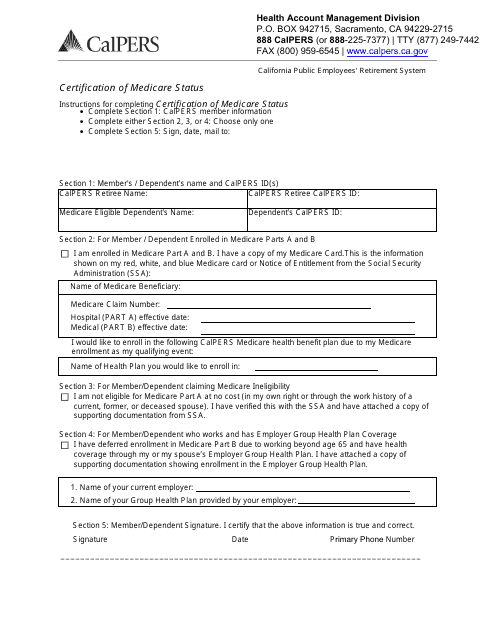
What are the requirements for Medicare certification?
- The date the plan of care being sent for certification becomes effective (the initial evaluation date is acceptable)
- Diagnoses
- Long term treatment goals
- Type, amount, duration and frequency of therapy services
- Signature, date and professional identity of the therapist who established the plan
What does it mean to be Medicare certified?
- Ambulatory Surgical Centers (ASC)
- Comprehensive Outpatient Rehabilitation Facilities (CORF)
- End-Stage Renal Dialysis (ESRD)
- Home Health Agencies (HHA) For more information about HHA Certification, please see Request Home Health Agency (HHA) Medicare certification
- Hospices
- Hospitals
- Laboratories (CLIA)
- Nursing Homes
How to get Medicaid certified?
“Medicare and Medicaid-certified facilities are expected to comply ... since they are less likely to get sick. Getting health care staff vaccinated, as well as getting individuals boosted ...

What happens if you don't revalidate Medicare?
Failing to revalidate on time could result in a hold on your Medicare reimbursement or deactivation of your Medicare billing privileges. If your Medicare billing privileges are deactivated, you’ll need to re-submit a complete Medicare enrollment application to reactivate your billing privileges.
Does Medicare reimburse you for deactivated services?
Medicare won’t reimburse you for any services during the period that you were deactivated. There are no exemptions from revalidation. Additionally, CMS doesn’t grant extensions; your notification email or letter will allow sufficient time to revalidate before your due date.
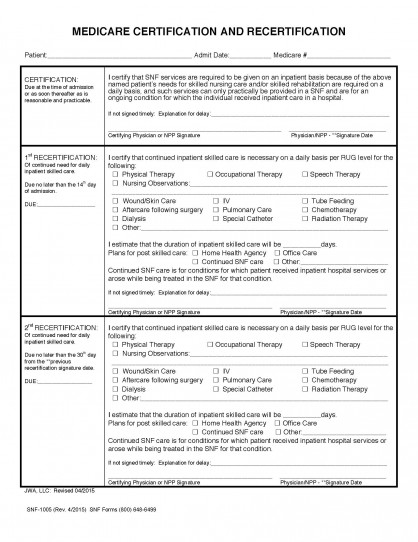
Who determines the method by which certifications and recertifications are to be obtained and the format of the
The individual hospital determines the method by which certifications and recertifications are to be obtained and the format of the statement. Thus, the medical and administrative staffs of each hospital may adopt the form and procedure they find most convenient and appropriate.
Who signs a recertification statement?
certification or recertification statement must be signed by the attending physician responsible for the case or by another physician who has knowledge of the case and is authorized to do so by the attending physician, or by a member of the hospital's medical staff with knowledge of the case.
Do skilled nursing facilities have to transmit recertification statements to the A/B MAC?
Skilled nursing facilities do not have to transmit certification and recertification statements to the A/B MAC (A); instead, the facility must itself certify, in the admission and billing form that the required physician certification and recertification statements have been obtained and are on file.
Do skilled nursing facilities have to get recertification?
Skilled nursing facilities are expected to obtain timely certification and recertification statements . However, delayed certifications and recertifications will be honored where, for example, there has been an isolated oversight or lapse.
Do you need a certification to be admitted to a hospital?
If an individual is admitted to a hospital (including a psychiatric hospital) before he/she is entitled to hospital insurance benefits (for example, before attainment of age 65), no certification is required as of the date of admission or entitlement. Certifications and recertifications are required as of the time they would be required if the patient had been admitted to the hospital on the day he/she became entitled. (The time limits for certification and recertification are computed from the date of entitlement instead of the date of admission.)
Do IPFs get recertifications?
IPFs are expected to obtain timely certifications and recertifications. However, delayed certifications and recertifications will be honored where, for instance, there have been an oversight or lapse, and a legitimate reason for the delay as noted in Pub. 100-01, §20.1. Denial of payment for lack of the required certification and recertification is considered a technical denial, which means a statutory requirement has not been met. Consequently, if an appropriate certification is later produced, the denial shall be overturned. Reopenings of technical denial decisions may be initiated by the contractor or the provider.
Do you need a separate recertification statement for PPS?
For cases not subject to PPS and for PPS day outlier cases, a separate recertification statement is not necessary where the requirements for the second or subsequent recertification are satisfied by review of a stay of extended duration, pursuant to the hospital's UR plan. However, it is necessary to satisfy the certification and recertification content standards. It would be sufficient if records of the UR committee show that consideration was given to the three items required for certifications and recertifications: the reasons for continued hospitalization (e.g., consideration was given to the need for special or unusual care in cost outlier status under PPS), estimated time the patient will need to remain in the hospital (e.g., the time period during which such special or unusual care would be needed), and plans for posthospital care.
Where is the narrative located on a recertification form?
If the narrative is part of the form, it must be located immediately above the physician's signature. If the narrative is an addendum, the physician must also sign the addendum immediately following the narrative.
What is the hospice policy for Medicare?
100-02), Ch. 9, §20.1. In order for a patient to be eligible for the Medicare hospice benefit, the patient must be certified as being terminally ill. An individual is considered to be terminally ill if the medical prognosis is that the individual's life expectancy is 6 months or less if ...
How long does it take to get a hospice certificate?
Initial certifications may be completed up to 15 days before hospice care is elected. Recertifications may be completed up to 15 days before ...
What document must be included in a beneficiary encounter?
Documentation must include the date of the encounter, an attestation by the physician or nurse practitioner that he/she had an encounter with the beneficiary. If the encounter was done by a nurse practitioner, he/she must attest that clinical findings were provided to the certifying physician.
Does hospice require a written certification?
In addition, the hospice must ensure the written certification/recertification is signed and dated prior to billing Medicare, or their claim (s) may be denied.
Can Medicare make payments without signatures?
Medicare cannot make appropriate payment without correct dates, signatures and identifying roles of the physician (s). The following list identifies the common types of missing and inadequate information: Predating physician (s) certification signatures.
Can a nurse practitioner certify a terminally ill patient?
Nurse practitioners and physician assistants cannot certify or recertify an individual is terminally ill. If the patient’s attending physician is a nurse practitioner or a physician assistant, the hospice medical director or the physician member of the hospice IDG certifies the individual as terminally ill.
What is a physician certification?
A physician certification/recertification of patient eligibility for the Medicare home health benefit is a condition for Medicare payment per sections 1814 (a) and 1835 (a) of the Social Security Act (the “Act”). The regulations at 42 CFR 424.22 list the requirements for eligibility certification and recertification.
What is 42 CFR 409.43?
If the physician’s orders for home health services meet the requirements specified in 42 CFR 409.43 Plan of Care Requirements, this meets the requirement for establishing a plan of care as part of the certification of patient eligibility for the Medicare home health benefit. Under Physician Care.
Is recertification required for episodes of care?
The requirements differ for eligibility certification and recertification; however, if the requirements for certification are not met, then claims for subsequent episodes of care, which require a recertification, will be non-covered—even if the requirements for recertification are met.
What is Medicaid renewal?
Medicaid renewal, also called Medicaid redetermination or recertification, is a necessary part of being a Medicaid beneficiary, regardless of if you receive benefits through the regular state plan, get long-term home and community based services (HCBS) via a Medicaid waiver, or are on nursing home Medicaid. The Medicaid redetermination process ...
How often does Medicaid redetermination happen?
However, generally speaking, Medicaid redetermination is limited to once every 12 months. To be clear, adults aged 65 and over, persons eligible for Home and Community Based Services, those eligible for SSI, and institutionalized individuals in nursing homes all fall must renew their Medicaid.
What happens if you don't renew your medicaid?
Failure to renew can result in loss of benefits. If a Medicaid beneficiary does not complete the redetermination process in time, Medicaid benefits will cease and there will be a lack of coverage.
How long does it take for Medicaid to report changes?
Most states require Medicaid beneficiaries to report any change in income or assets within 30 days.
Can you still receive medicaid if you are disabled?
The Medicaid redetermination process ensures one is still eligible to receive Medicaid benefits, and in the case of many seniors and disabled persons, continue to receive Medicaid-funded long-term services and supports.
Can Medicaid recipients be verified electronically?
For example, in some situations, the Medicaid recipient’s income and / or assets may not be able to be verified electronically. As an example, rental income and self-employment are two types of income that cannot be verified via electronic databases.
Can a public benefits counselor assist a Medicaid recipient?
However, if a Medicaid recipient no longer meets the eligibility criteria, a public benefits counselor cannot assist. For example, if the beneficiary receives an inheritance and now have assets valued above the Medicaid limit, they will not receive assistance from a public benefits counselor.
What is delayed/lapsed certification?
Delayed/Lapsed Certification. Physicians are required to certify the medical necessity of inpatient services. This is required on admission and if the service is needed for an extended period of time, a recertification is necessary. When these requirements are not met during audits, payments for services are denied.
Do you need a form for a delayed certification?
No specific procedures or forms are required for certification, recertification and delayed certification. The format of all certification and recertifications and the method by which they are obtained is determined by the individual facility.
Can a delayed certification extend past discharge?
A delayed certification may be included with one or more recertifications on a single signed statement. Delayed certification may not extend past discharge.