What is a Medicare Advantage special election period?
A special election period , also known as a special enrollment period, is a time period during which Medicare beneficiaries can change their Medicare Advantage or Part D coverage outside of the normal annual open enrollment period and after their initial enrollment period has ended.
What is a special election period (Sep)?
Special Election Periods (SEPs) exist for Part C (Medicare Advantage) and Part D (Prescription Drug) plans under certain circumstances. SEPs allow you to enroll in or disenroll from a Medicare Advantage (MA) plan or Part D plan depending on your situation:
What is the Medicare initial coverage election period (ICEP)?
Your Medicare Initial Coverage Election Period (ICEP) provides your first opportunity to enroll in a Medicare Advantage (Part C) plan. This guide looks at what you can do during the ICEP and how it differs from other Medicare enrollment periods.
Are there any Medicare State special elections in 2022?
There are a number of Medicare state special elections 2022 due to various situations. Most of them are weather emergencies and other FEMA designated emergencies. Below are a list of the most current SEP elections available by state. The emergencies/disasters listed as “open” means they have not yet set an end date for the election.

What is an example of a special election period?
The Special Election Period (SEP), also called a Special Enrollment Period, for Medicare Advantage and prescription drug plans is generally somewhat different from the Original Medicare SEP. Typically, the Medicare Advantage/prescription drug SEP applies to those who have lost their coverage.
What is a valid election period for Medicare?
A popular time to make Medicare coverage changes is during the Annual Election Period, also called Fall Open Enrollment. It runs from October 15 to December 7 every year. You can make changes like: Enrolling in a stand-alone Medicare prescription drug plan for the first time.
How many different types of election periods are there for Medicare Advantage?
three enrollment periodsUnderstanding the Different Medicare Enrollment Periods There are three enrollment periods for people signing up for benefits who are already enrolled in Original Medicare. During open enrollment, you can make changes to your Medicare plans and add additional coverage.
Which of the following is a qualifying life event for a Medicare Advantage Special Enrollment Period?
You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
What is an election period?
(1) Election period The term “election period” means the period which— (A) begins not later than the date on which coverage terminates under the plan by reason of a qualifying event, (B) is of at least 60 days' duration, and (C) ends not earlier than 60 days after the later of— (i) the date described in subparagraph (A ...
What is a special enrollment period for Medicare Part B?
What is the Medicare Part B special enrollment period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse's current job. You usually have 8 months from when employment ends to enroll in Part B.
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
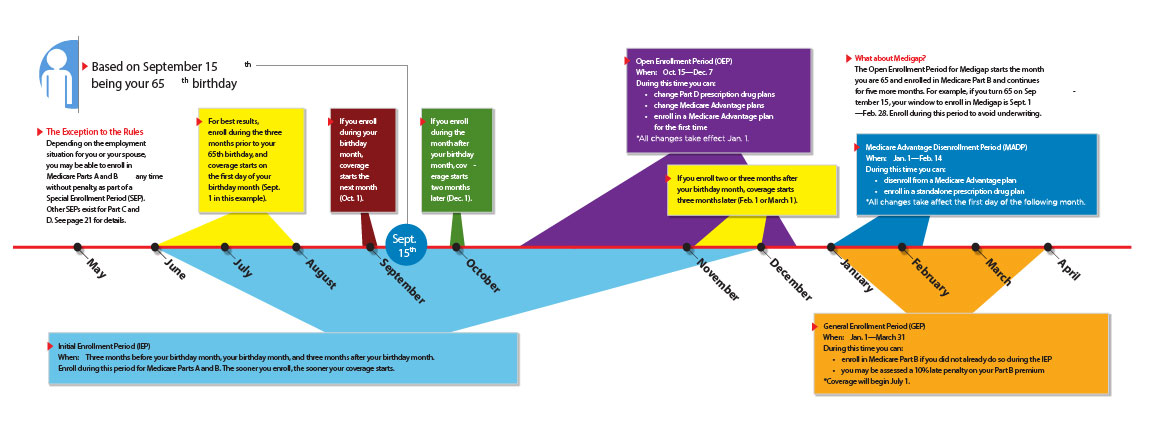
Is it too late to change Medicare Advantage plans?
You can change Medicare Advantage plans anytime during your Initial Enrollment Period. If you qualify for Medicare by age, your Initial Enrollment Period starts 3 months before the month you turn 65, includes the month you turn 65, and ends 3 months after the month you turn 65.
When can you switch from Medicare to Original Medicare?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
What are the 3 enrollment periods for Medicare?
This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month....When your coverage starts.If you sign up:Coverage starts:2 or 3 months after you turn 653 months after you sign up3 more rows
Can you lose Medicare benefits?
In most cases, you won't lose your Medicare eligibility. But if you move out of the country, or if you qualify for Medicare by disability or health problem, you could lose your Medicare eligibility.
Can you join Medicare mid year?
If you miss your first chance, generally you have to wait until fall for Medicare's annual Open Enrollment Period (October 15–December 7) to join a plan. During this time each year, you can also drop or switch your plan coverage.
What is Sep LEC?
Special Election Period SEP-LEC. Loss of Employer Coverage. SEP-MDE. Medicare/Medicaid Dual Enrollment.
What does MDE stand for in Medicare?
Medicare Direct Entry (MDE) Page 1. ® MDE accelerates your cash flow by providing comprehensive front-end edits and expedited claim processing, enabling you to process Medicare A and B claims earlier and with fewer rejections.
What is Medicare election period?
In Medicare terms, the word “election” means enrollment. A Medicare election period refers to the time when a person can enroll in the programs. A person may sign up for Medicare parts A and B during the initial enrollment period, when they first become eligible for Medicare. This is determined by the person’s birthday.
When is the Medicare enrollment period?
This runs from January 1 to March 31 every year.
How long does Medicare enrollment last?
They are insured with a group health plan or union through the employer. A special enrollment period lasts 8 months.
How long does it take to get Medicare?
The initial enrollment period, also called the initial Medicare election period, refers to the 7-month time frame when a person first becomes eligible for Medicare. During this period, a person can enroll in original Medicare. This includes Part A, which covers care in ...
How long does it take to enroll in Advantage?
A person can enroll in an Advantage plan during the initial enrollment period. The initial 7-month enrollment period includes: the 3 months before a person turns 65. the month in which they turn 65. the 3 months after they turn 65.
When is Medicare open enrollment?
Medicare offers two open enrollment periods each year. One is from January 1 to March 31, and the other is from October 15 to December 7. The rules for signing up during these periods differ.
When is it best to sign up for Medicare?
This period is when a person first becomes eligible for Medicare. It is best to sign up during the initial period. Doing so later on may require a person to face late penalties in the form of higher premiums. Due to various circumstances, an individual may miss signing up when they first become eligible.
You Moved
One of the most common reasons is changing where you live. Moving may take you out of your current provider’s service area, or it may open up one or more new plan options from the same provider.
You Lost Your Coverage
Another common reason is losing your current health coverage. If you’re no longer eligible for Medicaid or end coverage you used to have through your employer or union, including COBRA coverage, you typically will receive a two-month window to join a MA Plan or PDP.
Other Options Opened Up
Similarly, when you receive the opportunity to get other health coverage, whether it’s Medicaid, TRICARE, VA, offered by an employer or union, or provided by PACE or another program, you generally have the chance to drop whatever health plan you’re currently on and enroll in the new one as soon as it’s available.
Medicare Made a Move
Sometimes the government itself creates a special opportunity to change your plan, but it’s not usually for a good reason. Medicare may levy a sanction against a problematic health plan, suddenly terminate the plan’s contract or choose not to renew the plan’s contract when it expires.
Something Else
There are several other special cases when a SEP may be applicable to you, including if you become eligible for both Medicare and Medicaid, qualify for Extra Help to pay for prescription drugs, join or leave a State Pharmaceutical Assistance Program (SPAP), drop a Medigap policy to enroll in a MA Plan for the first time, are diagnosed with a severe or disabling condition for which there is a Medicare Chronic Care Special Needs Plan (SNP), experience a change in diagnosis that makes you no longer qualified for a SNP, discover your enrollment or change was affected by an error by a federal employee or you weren’t properly told your health coverage either was or wasn’t as good as Medicare drug coverage..
What is a SEP in Medicare?
Special Election Periods (SEPs) exist for Part C (Medicare Advantage) and Part D (Prescription Drug) plans under certain circumstances. SEPs allow you to enroll in or disenroll from a Medicare Advantage (MA) plan or Part D plan depending on your situation: If you are unable to make needed coverage changes during a given Medicare election period ...
When does Medicare Part D become effective?
If you enroll in a Part D plan during this SEP, your plan becomes effective July 1. If you enroll in Part B during the General Enrollment Period (GEP), and already have Part A, you have a SEP to sign up for a Medicare Advantage plan (with or without drug coverage) between April 1 and June 30. Your plan becomes effective July 1.
How long do you have to enroll in Medicare Part D?
If your creditable prescription drug coverage through your employer health plan ends, you have a 2-month SEP to enroll in a Part D plan, starting the day you lose coverage. If you live in an area with a Medicare Advantage and/or Part D plan (s) that has an overall plan performance rating of 5 stars, and you’re otherwise eligible to enroll in ...
How often do you have to change Medicare Advantage plans?
If you are eligible for full Medi-Cal benefits, you have an ongoing SEP to enroll in or change Medicare Advantage Prescription Drug plans (MA-PDs) or Part D plans once a quarter for the first 3 quarters of the year. Your coverage will be effective the first of the following month.
How long do you have to give Medicare a notice before a termination?
If Medicare terminates its contract with your MA or Part D plan because of misconduct and/or other reasons, your plan must give you 30 days notice before the termination date. Your SEP to switch to another plan begins 1 month before the termination happens and lasts for 2 months afterward.
How long does it take to get a SEP for a new insurance plan?
If you move out of your plan’s service area, you have a 2-month SEP to enroll in a new plan offered in your new residence area. This SEP begins either the date of your permanent move or the date you notify your plan of your move, whichever is later.
When does Medicare open enrollment start?
You can also make one change during the Annual Election Period (AEP), also known as Medicare’s Open Enrollment that runs from October 15 – December 7. Your coverage will be effective January 1. Note that beneficiaries who have been identified as “at risk” for opioid abuse, may be further restricted from changing plans.
When does Medicare start?
Medicare coverage begins 24 months after SS or RRB disability benefits. If you’re already eligible for Medicare because of a disability and you turned 65, you can sign up for a Medicare Advantage Plan or a Prescription Drug Plan.
How many enrollment periods are there for Medicare?
There are three enrollment periods for people signing up for benefits who are already enrolled in Original Medicare. During open enrollment, you can make changes to your Medicare plans and add additional coverage.
What is the ICEP period?
The ICEP is your first opportunity to choose a Medicare Advantage plan instead of Original Medicare. During the ICEP, you can also sign up for prescription drug coverage. If you enroll in Part B when you turn 65, your ICEP is the same as your IEP.
What is a SEP in Medicare?
A SEP is when you can make changes to your Medicare Advantage and Prescription Drug coverage when certain events happen in your life. Events include situations such as if you move or lose other insurance coverage. An example is losing health insurance ...
Why is Medicare enrollment confusing?
Medicare Enrollment Periods can be confusing because different enrollment periods have different dates for various purposes. There are many enrollment periods for people signing up for benefits for the first time. If you’re receiving Social Security or Railroad Retirement benefits when you turn 65, you’ll automatically be enrolled in Medicare.
What is open enrollment for Medicare 2021?
These enrollment periods fall into two categories. First, open enrollment is available to anyone eligible for Medicare. Then, Special Enrollment Periods. If you want to change the coverage you currently have, you can do so during one ...
How long does an OEP last?
Your OEP lasts for six months; you’ll be granted Medicare Supplement Guaranteed Issue Rights. During this time, you can sign up for a Medicare Supplement Plan, also known as Medigap. If you didn’t sign up for a Medicare Advantage or a drug plan during your IEP, the AEP is your next chance to make changes.
When does Medicare end?
You have a 7-month window to enroll in Medicare, beginning three months before coverage ends in November, including November, and ending on February 28, 2021 – three months after your employer or union coverage ends.
When can I apply for medicare?
As soon as you have lawful presence status, you become eligible for Medicare, assuming you are 65 years of age or older, or you meet one of the other criteria – for instance, disability. You should apply within three months of obtaining the status, or you may incur a penalty. So, in your case, be sure to apply for Medicare before November 30, 2020.
How long do you have to switch to Medicare Advantage?
If you notify your current plan now, you will have two more months – a total of three months – to choose a new Advantage plan.
How long do you have to enroll in Part B?
So, upon your return, you have three months to enroll in Part B (as well as Part A, if you haven’t done that yet). That would include the months of August, September and October. If you try to enroll after that, you may have to pay a penalty, and you will probably have to wait until January 1 of the following year.
Does Medicare pay for custodial care?
If you currently live in a nursing home, Medicare will pay for the first 100 days, provided that your health is improving. Medicare does not pay for custodial care, so if you stop improving, Medicare stops paying for your room and board.
Can I choose a Medicare Advantage plan?
You can choose a Medicare Advantage plan if available in your area, or a stand-alone plan. You are allowed to stay with the plan you have, also, if it fits your needs.
What is a SEP for Medicare?
What is the Medicare Part B Special Enrollment Period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 months from when employment ends to enroll in Part B. Coverage that isn’t through a current job – such as COBRA benefits, ...
What is a Part B SEP?
The Part B SEP allows beneficiaries to delay enrollment if they have health coverage through their own or a spouse’s current employer. SEP eligibility depends on three factors. Beneficiaries must submit two forms to get approval for the SEP. Coverage an employer helps you buy on your own won’t qualify you for this SEP.
When do you have to take Part B?
You have to take Part B once your or your spouse’s employment ends. Medicare becomes your primary insurer once you stop working, even if you’re still covered by the employer-based plan or COBRA. If you don’t enroll in Part B, your insurer will “claw back” the amount it paid for your care when it finds out.
How long can you delay Part B?
You can delay your Part B effective date up to three months if you enroll while you still have employer-sponsored coverage or within one month after that coverage ends. Otherwise, your Part B coverage will begin the month after you enroll.
When is Medicare open enrollment?
The Medicare Advantage Open Enrollment Period (MAOEP) runs from January 1 through March 31.
When do you turn 65 and get Medicare?
As before, let’s imagine you turn 65 on August 16 and are newly eligible for Medicare. However, because you’re still employed and have employer group health plan coverage, you decide to enroll in Part A during the IEP and delay joining Part B.
How to qualify for ICEP?
How Do I qualify for an ICEP? To trigger an ICEP and join a Medicare Advantage plan, you must have both Medicare Part A and Medicare Part B coverage . Also, your permanent residence must be within the service area of your chosen Medicare Advantage plan. If you don’t enroll in Part B during the IEP, you cannot enroll in a Medicare Advantage plan ...
How long does an IEP last?
Your IEP lasts for seven months, beginning three months before your 65th birthday. If you enroll in Medicare parts A and B during the IEP, then your ICEP runs simultaneously. Some people choose not to enroll in Medicare Part B during their IEP.
What is an IEP and an ICEP?
What are IEP and ICEP? The IEP and ICEP are both one-time Medicare enrollment periods. For many beneficiaries, these periods happen at the same time. The Medicare Initial Enrollment Period (IEP) is your first opportunity to enroll in Original Medicare, which consists of Part A and Part B and is administered by the federal government.
What is Medicare OEP?
What is the Medicare OEP? 1 The Medicare Advantage Open Enrollment Period (MAOEP) runs from January 1 through March 31. It allows people currently enrolled in a Medicare Advantage plan to make a one-time change. For example, you could switch to a different Medicare Advantage plan or disenroll from your Medicare Advantage plan and return to Original Medicare. You cannot change from one Part D plan to another. 2 There is also the fall Medicare Open Enrollment Period (OEP) mentioned earlier, which runs from October 15 through December 7 each year. During the OEP, you can join, switch or leave a plan, with changes to coverage beginning on January 1 of the following year.
What is Medicare Advantage?
Private insurance companies sell Medicare Advantage plans that replace your Original Medicare coverage. These options provide at least the same healthcare coverage as Original Medicare. Many people prefer them because they often offer additional benefits, such as prescription drug coverage and wellness benefits.
