
Full Answer
How to get a temporary Medicaid card?
A temporary Medicaid card can be issued if you show proof of eligibility for the program and a medical problem that requires immediate treatment. If you are already approved for Medicaid, you may be able to request a temporary card from your county Human Services department, print one from an online account or simply use your patient number. The process varies by state and by county.
How much is the copay for Medicare?
There is a 20% copay of the Medicare-approved amount for outpatient services after the deductible. Medicare Advantage plans are required by law to provide—at minimum—the same coverage, benefits and rights provided by Original Medicare Part A and Part B, with the exception of hospice care.
Are retirement dates required on Medicare claim?
Providers must report collected retirement dates on their Medicare claims using occurrence code 18 for the beneficiary’s retirement date and occurrence code 19 for the spouse’s retirement date.
Is Medicare deducted from military retirement pay?
When a military retiree or spouse reaches 65, they are eligible for Medicare and TRICARE for Life medical coverage. TRICARE for Life is specifically for Medicare eligible military retirees. Medicare pays first for Medicare-covered services.
What is Medicare PLB?
Provider Level Adjustment. Provider-Level Adjustment (PLB) reason codes describe adjustments. the Medicare Contractor makes at the provider level, instead of a. specific claim or service line.
What is C5 temporary allowance?
C5 – Temporary Allowance This code is used to inform you that we have identified an overpayment of less than $50. We recommend checking your books to confirm details. You may elect to submit a refund to BCBSIL. If you disagree, overpayment disputes/appeals must be submitted within 90 days from the date of the report.
What is a PLB amount?
Page 1. Provider-Level Balance (PLB) Supplement to the Electronic Remittance Advice 835 Transaction Companion Guide. The PLB segment is used to transmit information about Provider-Level Adjustments - that is, payments and debts that are not specific to a particular claim or service.
What is an L3 penalty from Medicare?
L3. Provider Penalty - indicates an amount withheld from payment based on an established penalty. L6. Interest owed: - If the net interest is added to the "TOTAL PD" amount, then the offset detail will be a negative number.
What is a Medicare B2 rebate?
A negative value represents a payment. B2. Refund - Used to reflect accelerated payment amounts or withholdings. A positive value represents a withholding. A negative value represents a payment.
What is adjustment Code 72?
72. Provider refund amount. This adjustment acknowledges a refund received from a provider for previous overpayment.
What does PLB Reason code wo mean?
Overpayment amount deducted-WO in PLB reason code. -Overpayment amount deducted from remittance total.
How do I get Medicare Electronic Remittance Advice?
Please contact our Electronic Data Interchange (EDI) department at (866) 234-7331 for more information. Medicare also offers free software called Medicare Remit Easy Print (MREP), which allows providers to view and print the ERA.
What is Medicare offset?
Offset causes withholding of overpayment amounts on future Medicare payments. This is done in one of two ways: Contractor initiated when the money is not returned within the appropriate time frame after the initial notice of overpayment (see below) Provider requests immediate recoupment.
What is a claim payment remittance advice and check?
An electronic remittance advice, or ERA, is an explanation from a health plan to a provider about a claim payment. An ERA explains how a health plan has adjusted claim charges based on factors like: Contract agreements. Secondary payers. Benefit coverage.
What are adjustment reason codes?
Claim adjustment reason codes (CARCs) communicate an adjustment, meaning that they must communicate why a claim or service line was paid differently than it was billed.
How much does Medicare pay?
Medicare pays for 80 percent of your covered expenses. If you have original Medicare you are responsible for the remaining 20 percent by paying deductibles, copayments, and coinsurance. Some people buy supplementary insurance or Medigap through private insurance to help pay for some of the 20 percent.
What is Medicare reimbursement?
The Centers for Medicare and Medicaid (CMS) sets reimbursement rates for all medical services and equipment covered under Medicare. When a provider accepts assignment, they agree to accept Medicare-established fees. Providers cannot bill you for the difference between their normal rate and Medicare set fees.
What is Medicare Part D?
Medicare Part D or prescription drug coverage is provided through private insurance plans. Each plan has its own set of rules on what drugs are covered. These rules or lists are called a formulary and what you pay is based on a tier system (generic, brand, specialty medications, etc.).
Is Medicare Advantage private or public?
Medicare Advantage or Part C works a bit differently since it is private insurance. In addition to Part A and Part B coverage, you can get extra coverage like dental, vision, prescription drugs, and more.
Do providers have to file a claim for Medicare?
They agree to accept CMS set rates for covered services. Providers will bill Medicare directly, and you don’t have to file a claim for reimbursement.
Can you bill Medicare for a difference?
Providers cannot bill you for the difference between their normal rate and Medicare set fees. The majority of Medicare payments are sent to providers of for Part A and Part B services. Keep in mind, you are still responsible for paying any copayments, coinsurance, and deductibles you owe as part of your plan.
How long does Medicare pay for a fee for service?
When determining a payment amount to request, physicians should consider that their Medicare fee-for-service payments will be automatically reduced starting four months after the payment is issued for up to three months or until repayment is met.
How long do you have to bill Medicare for advance payments?
To qualify for advance/accelerated payments physicians, providers or suppliers must: Have billed Medicare for claims within 180 days immediately prior to the date of signature on the physician’s request form. Not be in bankruptcy. Not be under active medical review or program integrity investigation. Not have any outstanding delinquent Medicare ...
When will CMS expand the advance payment program?
Updated April 6, 2020. In order to help physicians and other providers, the Centers for Medicare & Medicaid Services (CMS) has expanded its Accelerated and Advance Payment Program for the duration of the public health emergency. CMS is authorized to provide accelerated or advance payments during the period of the public health emergency ...
How long does it take for a physician to receive a full payment?
Physicians will receive full payments for their claims during the 120-day delay period. At the end of the 120-day period, the recoupment process will begin and every claim submitted by the physician will be offset from the new claims to repay the accelerated/advanced payment.
Part A
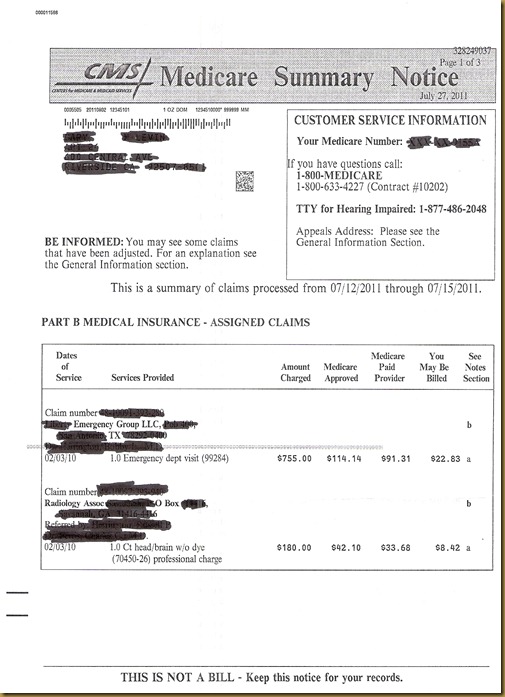
On page two of the provider remittance, information concerning offset is in the second and third columns. See illustration below. Offset information in bold.
Part B
The Medicare provider voucher has an "Offset Details" field. This field can be used for three different reasons:
