What are the Medicare treatment authorization field requirements for tracking numbers?
Unique Tracking Number Field Requirements for Prior Authorization For all Medicare Part A providers submitting electronic claims, the Medicare Treatment Authorization field must contain blanks or valid Medicare data in the first 14 bytes of the treatment authorization field at the loop 2300 REF02 (REF01=G1) segment for the ASC X12 837 claim.
What is a Medicare claim number and what does it mean?
On a Medicare card received before 2015, your Medicare Claim Number consisted of your Social Security number followed by a code of letters and sometimes numbers that have a specific meaning. In more recent years, a randomly-generated combination of letters and numbers replaced this Medicare Claim number.
How do I Look Up my Medicare number?
Due to the sensitive nature of your Medicare number, it can be looked up online after making an account with “ my Social Security “. If you lose your Medicare card with your number on it, you can request that the Social Security Administration replace your card at no charge
What is a Medicare provider number?
Your Medicare provider number is used for billing and identification purposes and typically consists of your social security number followed by a code of letters and sometimes numbers that have a specific meaning.

What is a UTN for Medicare?
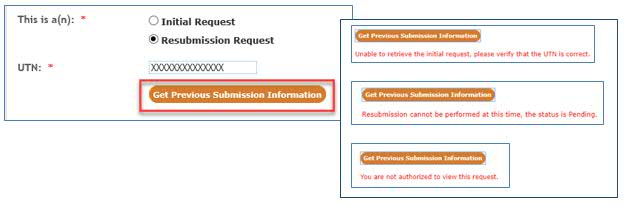
o A Unique Tracking Number (UTN) will be included on the decision notice from First Coast. The UTN must be submitted on the hospital claim to receive payment. Claims billed without a UTN will be denied. The UTN should be included on your booking sheet in order to schedule the surgery.
What is the UTN?
The aim of the Universal Trial Number (UTN) is to facilitate the unambiguous identification of clinical trials. The UTN is not a registration number. The UTN is a number that should be obtained early in the history of the trial. The UTN should: become permanently attached to the trial.
What is a pre Claim Review Determination Letter?
Pre-claim review is a process through which a request for provisional affirmation of coverage is submitted for review before a final claim is submitted for payment. Pre-claim review helps make sure that applicable coverage, payment, and coding rules are met before the final claim is submitted.
Which of the following is a common reason why insurance claims are rejected?
Minor data errors are the most common reason for claim denials. Sometimes, a provider may code the submission wrong, leave information out, misspell your name or have your birth date wrong. Your explanation of benefits (EOB) will give you clues, so check there first.
When did pre-claim review start?
The initial three-year pre-claim review demonstration begins in Illinois on August 1, 2016 and then will roll out to Florida, Texas, Michigan and Massachusetts.
What is pre-claim investigation?
Pre-Claim Inquiry means a verifiable request, demand or summons to an Insured Person by an Enforcement Entity or the Insured Entity to appear at a meeting or requisite place of confine- ment or detention, or produce documents to, an Enforcement Entity regarding such Insured Person's capacity in the business of the ...
What information is on my Medicare card?
There is additional important information located on your Medicare card for you and your doctor. This includes your name and sex. Additionally, it states whether you have Medicare Part A (inpatient hospital) and Medicare Part B (outpatient medical), and lists the dates that Part A and B first started.
How long does it take for Medicare to arrive in the mail?
After your replacement request, the card typically arrives in the mail in about 30 days, at no cost to the beneficiary. Social Security will mail your Medicare card to the address they have on file for you, so it is important to keep your information with them up to date.
What happens if you lose your Medicare card?
If you lose your Medicare card with your number on it, you can request that the Social Security Administration replace your card at no charge. The Medicare Beneficiary Identifier is for claims, billing and identification purposes.
What does it mean when you have an A on your Social Security card?
If you have an A on your card, it means that you are the primary beneficiary. That means you earned Medicare insurance based on your working history and tax credits.
What do the codes after my Social Security number mean?
After the Social Security number, there is a letter and sometimes a number. These codes all have different meanings.
What is a B1 on Medicare?
There are several variations to the B code: B1 is for a husband of a primary beneficiary at age 62 or over. B2 is for a young wife with a child in her care,
Can I use my Social Security number on my Medicare card?
Removing Social Security numbers from Medicare cards further protects the identities of Medicare beneficiaries. The replacement number is called the Medicare Beneficiary Identifier, or MBI number. Moreover, if you still have a Medicare card with your Social Security number on it, you can still use it. Nonetheless, getting a new Medicare card is ...
Review Decisions and Timeframes
Timeframes for conducting PAR will be dependent upon the service (s) and documentation submitted for PAR. There are three types of review timeframes:
Decision Letter (s)
The MAC will send decision letters with the UTN to the requester using the method the PAR was received postmarked within the timeframes described above. The MAC will have the option to send a copy of the decision to the requester via fax if a valid fax number was provided, even if the submission was sent via mail.
Decisions
A provisional affirmation PA decision is a preliminary finding that a future claim submitted to Medicare for the service (s) likely meets Medicare’s coverage, coding, and payment requirements.
Suspension of a PA Process
CMS may suspend the OPD services PA process requirement generally or for a particular service (s) at any time by issuing a notification on the CMS website.
Claim Submission
Cases where a PAR was submitted and a provisional affirmation PA decision was granted, including any service (s) that was part of a partially affirmed decision.
Insurance
NOTE: Whether Medicare is listed as primary or secondary, a prior authorization is required.
Advance Beneficiary Notice of Non-coverage (ABN)
If an applicable claim is submitted without a PAR decision and is flagged as having an ABN, it will be stopped for additional documentation to be request and a review of the ABN will be performed (to determine the validity of the ABN) following standard claim review guidelines and timelines.
What is a change request for Medicare?
I. SUMMARY OF CHANGES: The purpose of this change request (CR) is to inform the Medicare Administrative Contractors (MACs) about the prior authorization process. Also, this CR will direct the MACs to individualized Operational instruction(s) that will highlight the specifications for each new prior author ization program that the Centers for Medicare & Medicaid Services (CMS) will implement as applicable. This CR also provides an overview of 42 C.F.R. 414.234 for the Durable Medical Equipment (DME) MACs.
What is Medicare Administrative Contractor?
The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC Statement of Work. The contractor is not obligated to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer. If the contractor considers anything provided, as described above, to be outside the current scope of work, the contractor shall withhold performance on the part(s) in question and immediately notify the Contracting Officer, in writing or by e-mail, and request formal directions regarding continued performance requirements.
What is prior authorization?
Prior authorization is a process through which a request for provisional affirmation of coverage is submitted to CMS or its contractors for review before the item or service is furnished to the beneficiary and before the claim is submitted for processing. It is a process that permits the submitter (e.g., provider, supplier, beneficiary, etc.) to send in medical documentation in advance of providing and billing for an item or service, to verify its eligibility for Medicare claim payment. Contractors shall, at the direction of CMS or other authorizing entity, conduct prior authorizations and alert the submitter of any potential issues with the information, as submitted.