If Medicare has approved, or fully or partially denied your medical claim (this is the initial determination, and it’s made by the Medicare Administrative Contractor (MAC), which processes Medicare claims) Read your MSN carefully. If you disagree with a Medicare coverage
Full Answer
What is the Medicare Coverage Determination process?
The Medicare contractor makes an initial determination when a claim for Medicare benefits under Part A or Part B is submitted. A beneficiary who is dissatisfied with the initial determination may request that the contractor perform a redetermination of the claim if the requirements for obtaining a redetermination are met.
What is a Medicare a redetermination?
National coverage determinations (NCDs) are made through an evidence-based process, with opportunities for public participation. In some cases, CMS' own research is supplemented by an outside technology assessment and/or consultation with the Medicare Evidence Development & Coverage Advisory Committee (MEDCAC). In the absence of a national coverage policy, an …
How do I request a coverage determination from my insurance?
(1) A determination with respect to entitlement to hospital insurance or supplementary medical insurance under Medicare . (2) A disallowance of an individual's application for entitlement to hospital or supplementary medical insurance, if the individual fails to submit evidence requested by SSA to support the application.
How do I know if my Medicare claim has been approved?
Initial IRMAA Determination What is it? You'll get this notice if you have Medicare Part B and/or Part D and Social Security determines that any Income Related Monthly Adjustment Amounts …

What is an initial determination Medicare?
The Medicare contractor makes an initial determination when a claim for Medicare benefits under Part A or Part B is submitted.
What is organization determination in Medicare?
An organization determination is any decision made by a Medicare health plan regarding: Authorization or payment for a health care item or service; The amount a health plan requires an enrollee to pay for an item or service; or. A limit on the quantity of items or services.Dec 1, 2021
What is a Medicare determination appeal?
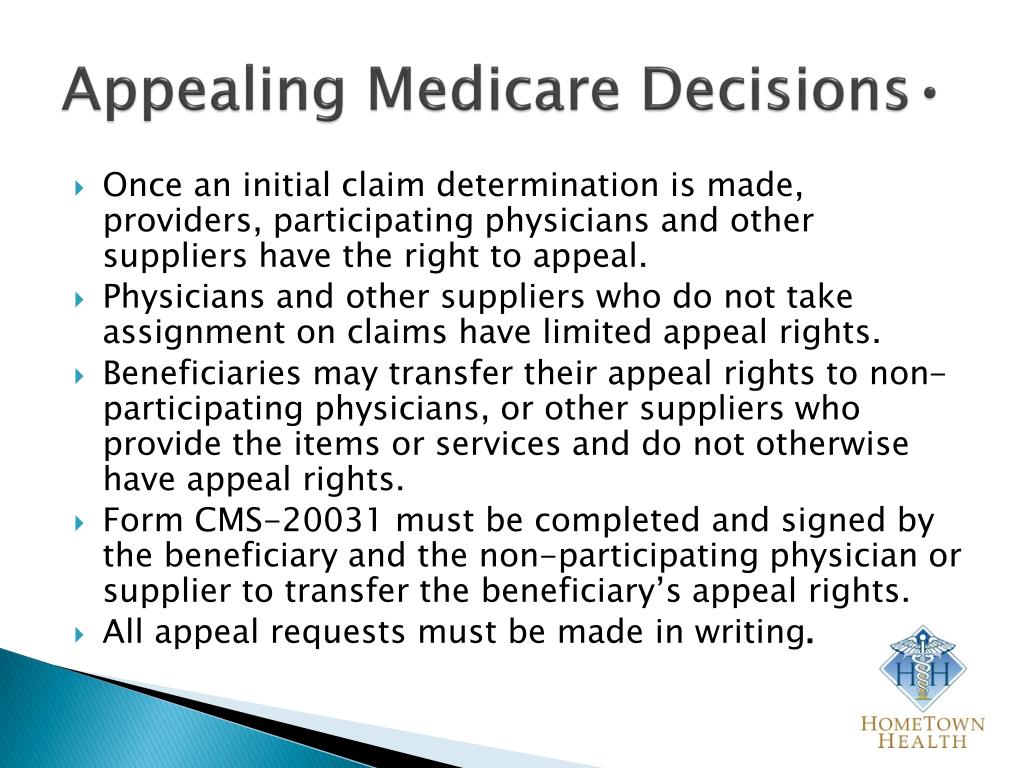
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
What are the five steps in the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
When an organization makes a decision to pay for medical care it is called?
An “organization determination,” or medical prior authorization, is a decision we make about your medical benefits and coverage or about the amount we will pay for your medical services.Oct 1, 2021
What is ODAG and CDAG?
Medicare Part C and Part D Program Audit Protocols (2020): Part C Organization Determinations, Appeals and Grievances (ODAG) and Part D Coverage Determinations, Appeals and Grievances (CDAG) Audit Protocols were released by CMS in June 2020.Oct 28, 2020
How successful are Medicare appeals?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.Jun 20, 2013
Why was my Medicare claim denied?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
What is the highest level of a Medicare Redetermination?
Medicare FFS has 5 appeal process levels:Level 1 - MAC Redetermination.Level 2 - Qualified Independent Contractor (QIC) Reconsideration.Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition.Level 4 - Medicare Appeals Council (Council) Review.
What is the last level of appeal for Medicare?
The levels are: First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA)
How do you win a Medicare appeal?
To increase your chance of success, you may want to try the following tips: Read denial letters carefully. Every denial letter should explain the reasons Medicare or an appeals board has denied your claim. If you don't understand the letter or the reasons, call 800-MEDICARE (800-633-4227) and ask for an explanation.Nov 12, 2020
What is an initial determination for Medicare?
The Medicare contractor makes initial determinations regarding claims for benefits under Medicare Part A and Part B. A finding that a request for payment or other submission does not meet the requirements for a Medicare claim as defined in § 424.32 of this chapter, is not considered an initial determination. An initial determination ...
What is a reconsideration in SSA?
SSA makes initial determinations and processes reconsiderations with respect to an individual on the following: (1) A determination with respect to entitlement to hospital insurance or supplementary medical insurance under Medicare . (2) A disallowance of an individual's application for entitlement to hospital or supplementary medical insurance, ...
How to determine Part D coverage?
A coverage determination is any decision made by the Part D plan sponsor regarding: 1 Receipt of, or payment for, a prescription drug that an enrollee believes may be covered; 2 A tiering or formulary exception request (for more information about exceptions, click on the link to "Exceptions" located on the left hand side of this page); 3 The amount that the plan sponsor requires an enrollee to pay for a Part D prescription drug and the enrollee disagrees with the plan sponsor; 4 A limit on the quantity (or dose) of a requested drug and the enrollee disagrees with the requirement or dosage limitation; 5 A requirement that an enrollee try another drug before the plan sponsor will pay for the requested drug and the enrollee disagrees with the requirement; or 6 A decision whether an enrollee has, or has not, satisfied a prior authorization or other utilization management requirement.
What is a prior authorization?
A requirement that an enrollee try another drug before the plan sponsor will pay for the requested drug and the enrollee disagrees with the requirement; or. A decision whether an enrollee has, or has not, satisfied a prior authorization or other utilization management requirement.
What is a redetermination in Medicare?
A redetermination is a review of the claim by Medicare Administrative Contractor (MAC) personnel not involved in the initial claim determination.
How long does it take for a MAC to send a decision?
Generally, the MAC will send its decision (either in a letter, an RA, and/or an MSN) to all parties within 60 days of receipt of the request for redetermination. The decision will contain detailed information on further appeals rights, where applicable.
What does Q7 mean in hospice?
Q7. A beneficiary is in a hospice and is no longer considered to be terminally ill. The hospice tells the beneficiary that Medicare coverage of hospice services will be ending and that he can continue his care under a HHA. Should the beneficiary receive a generic notice?
What is a QIO review?
Through this expedited determination process, beneficiaries may obtain a QIO review a provider’s decision to discharge them, or end all their covered care , for medical necessity reasons.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
What is a QIC?
QIC is an independent contractor that didn’t take part in the level 1 decision. The QIC will review your request for a reconsideration and will make a decision.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Can you request a fast reconsideration?
If you disagree with the plan’s redetermination, you, your representative, or your doctor or other prescriber can request a standard or expedited (fast) reconsideration by an IRE. You can’t request a fast reconsideration if it’s an appeal about payment for a drug you already got.
What to do if you are not satisfied with QIC?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or , in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
How to appeal a Medicare redetermination?
There are 3 ways to file an appeal: 1 Fill out a " Redetermination Request Form [PDF, 100 KB] " and send it to the Medicare contractor at the address listed on the MSN. 2 Follow the instructions for sending an appeal. You must send your request for redetermination to the company that handles claims for Medicare (their address is listed in the "Appeals Information" section of the MSN).#N#Circle the item (s) and/or services you disagree with on the MSN.#N#Explain in writing why you disagree with the decision or write it on a separate piece of paper, along with your Medicare number, and attach it to the MSN.#N#Include your name, phone number, and Medicare Number on the MSN.#N#Include any other information you have about your appeal with the MSN. Ask your doctor, other health care provider, or supplier for any information that may help your case. 3 Send a written request to the company that handles claims for Medicare (their address is listed in the "Appeals Information" section of the MSN.) Your request must include:#N#Your name and Medicare Number.#N#The specific item (s) and/or service (s) for which you're requesting a redetermination and the specific date (s) of service.#N#An explanation of why you don't agree with the initial determination.#N#If you've appointed a representative, include the name of your representative.
How long does it take to appeal a Medicare payment?
The MSN contains information about your appeal rights. You'll get a MSN in the mail every 3 months, and you must file your appeal within 120 days of the date you get the MSN.
How long does it take for Medicare to make a decision?
You can submit additional information or evidence after the filing redetermination request, but, it may take longer than 60 days for the Medicare Administrator Contractor (MAC) that processes claims for Medicare to make a decision. If you submit additional information or evidence after filing, the MAC will get an extra 14 calendar days ...
What is a redetermination request?
The specific item (s) and/or service (s) for which you're requesting a redetermination and the specific date (s) of service. An explanation of why you don't agree with the initial determination. If you've appointed a representative, include the name of your representative.
