Choose MedEnvios Healthcare for Medicare-covered Diabetic Supplies Simplify the way you support your health by partnering with MedEnvios Healthcare, the nation’s premier provider of medical supplies. Whether you’re in need of diabetic supplies that are eligible for Medicare coverage or other necessities, we have you covered.
Full Answer
Does Medicare cover diabetic supplies?
If an individual has original Medicare, then Medicare Part B will cover some diabetic supplies, such as: However, Medicare does not cover the following supplies: In 2021, a person with Medicare Part B will pay 20% of the cost for diabetes self-management supplies such as glucose monitors, lancets, and test strips.
Does Medicare pay for diabetic self management supplies?
Costs for diabetic self-management supplies In 2020, a person with Medicare Part B will pay 20% of the cost for diabetes self-management supplies such as glucose monitors, lancets, and test strips. However, to ensure Medicare coverage, a person must get the prescription from their doctor, and use an in-network pharmacy or supplier.
Will Medicare pay for damaged medical equipment?
If Original Medicare already paid for durable medical equipment (like a wheelchair or walker) or supplies (like diabetic supplies) damaged or lost due to an emergency or disaster: • In certain cases, Medicare will cover the cost to repair or replace your equipment or supplies.
How do I order supplies for my diabetes care?
Supplies are delivered at no cost and can be ordered online 24/7. In addition to supplies, Byram Healthcare offers a Diabetes Careline and Clinical Support services, which can connect you to Certified Diabetes Care and Education Specialists between visits. It also provides reorder reminder calls when your supplies are due to be refilled.
What brand of glucose meter is covered by Medicare 2021?
A2: Starting January 1, 2021, covered meters include: OneTouch Verio Reflect ®, OneTouch Verio Flex®, OneTouch Verio® and OneTouch Ultra 2®. All OneTouch test strips will have preferred formulary status.
What brand of CGM is covered by Medicare?
This rule took effect at the beginning of this month, so people with Medicare now have access to Dexcom G6, Abbott Freestyle Libre, Senseonics Eversense and Medtronic Guardian, as long as these CGMs are used with an insulin pump or with use of a standalone receiver.
Is Livongo covered by Medicare?
Mountain View, CA – April 30, 2019 – Livongo, the leading Applied Health Signals company empowering people with chronic conditions to live better and healthier lives, today announced that it has been approved by the Centers for Medicare and Medicaid Services (CMS) as an enrolled provider for Medicare Advantage members.
Are diabetic test strips and lancets covered by Medicare?
Medicare Part B covers the same type of blood glucose testing supplies for people with diabetes whether or not they use insulin. However, the amount of supplies that are covered varies. Uses insulin, they may be able to get up to 100 test strips and lancets every month, and 1 lancet device every 6 months.
How much does dexcom cost with Medicare?
Q: How much does CGM cost for Medicare users? A: According to Dexcom's Medicare FAQ page, those covered by Medicare can expect to pay 20% of the costs of their G5 CGM, which is roughly $50 per month. (This may be covered by secondary insurance.) Medicare will cover the remaining 80%.
What brand of CGM does Medicare 2022 cover?
Beginning Feb. 28, 2022, those using a Medtronic CGM integrated with the company's MiniMed insulin pumps will be able to get Medicare coverage for their transmitters, sensors and supplies.
What brand of glucose meter does Medicare 2020 cover?
FreeStyle LibreAvailable to people with type 1 or type 2 diabetes on intensive insulin therapy. Another continuous glucose sensor option for people over 65 is now covered, in addition to Dexcom G5! This just in: Medicare will now cover Abbott's FreeStyle Libre real-time continuous glucose monitoring (CGM) system.
Is Accu Chek covered by Medicare?
Accu-Chek is ALWAYS COVERED on Medicare Part B Your patient pays only $1.66 for 50 test strips and may pay a $0 co-pay.
How much is Livongo?
$49.99 per monthThe Livongo plan costs $49.99 per month, with a minimum three-month commitment to start.
How do I get free diabetic supplies?
People who don't have insurance coverage for prescriptions may find their medicines and supplies for free or at low cost through PPARX.org. RxAssist.org lists drug-company assistance programs, state programs, discount drug cards, copay help, and more.
Is diabetes a disability?
Under most laws, diabetes is a protected as a disability. Both type 1 and type 2 diabetes are protected as disabilities.
Does Medicare pay for Libre FreeStyle?
Medicare covers CGMs like the FreeStyle Libre under the durable medical equipment (DME) portion of Medicare Part B, provided you meet eligibility criteria. If you qualify for coverage for the monitor, Medicare will also cover your supplies within certain limits.
What Diabetes Supplies Does Medicare Pay For?
There are 34.2 million Americans managing diabetes and an additional 88 million Americans who have prediabetes.[i] That’s why diabetic supplies are...
What Brand of Diabetic Testing Supplies Does Medicare Cover?
Wondering what brand of diabetic supplies is covered by Medicare? Major brands such as Contour Next, OneTouch, FreeStyle, and Accu-Check are all co...
Does Medicare Cover Continuous Glucose Monitors?
If you’re using insulin and you need to closely monitor your glucose levels, Medicare will cover a therapeutic continuous glucose monitor. You’ll n...
Does Medicare Cover Insulin Pumps for Type 2 Diabetes?
Medicare Part B covers insulin pumps if the pump is medically necessary. You’ll need a prescription from your doctor, and you’ll need to meet these...
How Do I Get Free Diabetic Supplies?
It’s no secret that diabetic supplies can get pricey. Buying glucose monitors, test strips, and insulin can add up fast. Thankfully Medicare has yo...
What Do I Have to Pay?
Remember that not all covered items are free. For most of your diabetic supplies, coinsurance and copayments still apply. Original Medicare Part B...
How Do I Get My Diabetic Supplies Through Medicare?
To get diabetes supplies through Medicare, start by talking to your doctor. You’ll need a prescription for all your medications and supplies. Once...
What Diabetic Supplies are Covered by Medicaid?
Do you qualify for both Medicare and Medicaid? If you’re dual-eligible, you can get expanded coverage for your diabetes supplies.
What Are the Most Common Supplies Needed by People with Diabetes?
The most common diabetes supplies are covered by Medicare. These include:
How Do I Cope with Finding Out I Have Diabetes?
If you’ve recently received a diabetes diagnosis, take a big breath. It’s easy to feel overwhelmed, but you’re not alone. There are several ways yo...
Medicare Eligibility For A Therapeutic Cgm
A therapeutic CGM is a medical device approved by the U.S. Food and Drug Administration as a replacement for home blood sugar monitors. It provides you and your doctor with the medically necessary information to make diabetes treatment decisions, such as changes in diet and your insulin dosage.
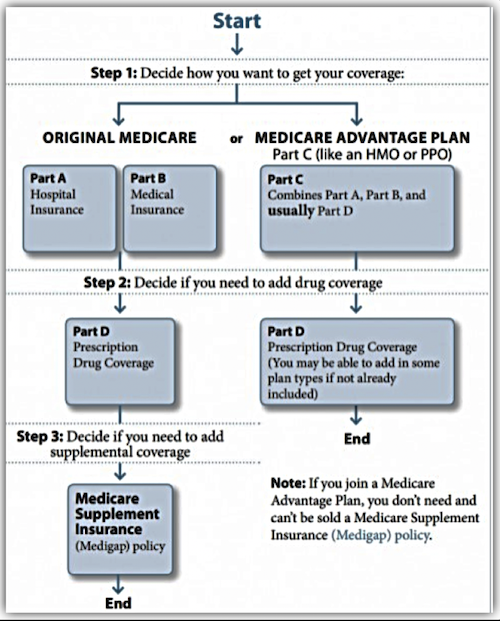
Medicare And Diabetes Coverage
Medicare and diabetes coverage is a concern for many Americans. Diabetes can cause a persons health and well-being to deteriorate over time. Close monitoring is often necessary because diabetes causes other health concerns and conditions. Below we go into full detail about what you need to know regarding Medicare and diabetes coverage.
Who Is It For
If you are prediabetic or experience Type 2 Diabetes, as well as you notice that you do not obtain enough high quality sleep during the night, Deep Sleep Diabetes Remedy program is most likely the program for you. Kill 2 birds with one rock: improve your sleep and also energy levels and also reverse your diabetic issues with this program.
How Much Do Testing Supplies Cost
If youve met your Part B deductible , you will pay 20 percent of the Medicare-approved amount for diabetic testing supplies. Medicare pays the other 80 percent.
Medicare Part B Covered Diabetes Testing Supplies
Part B covers a number of blood sugar self-testing supplies and equipment, even if you dont use insulin. These include:
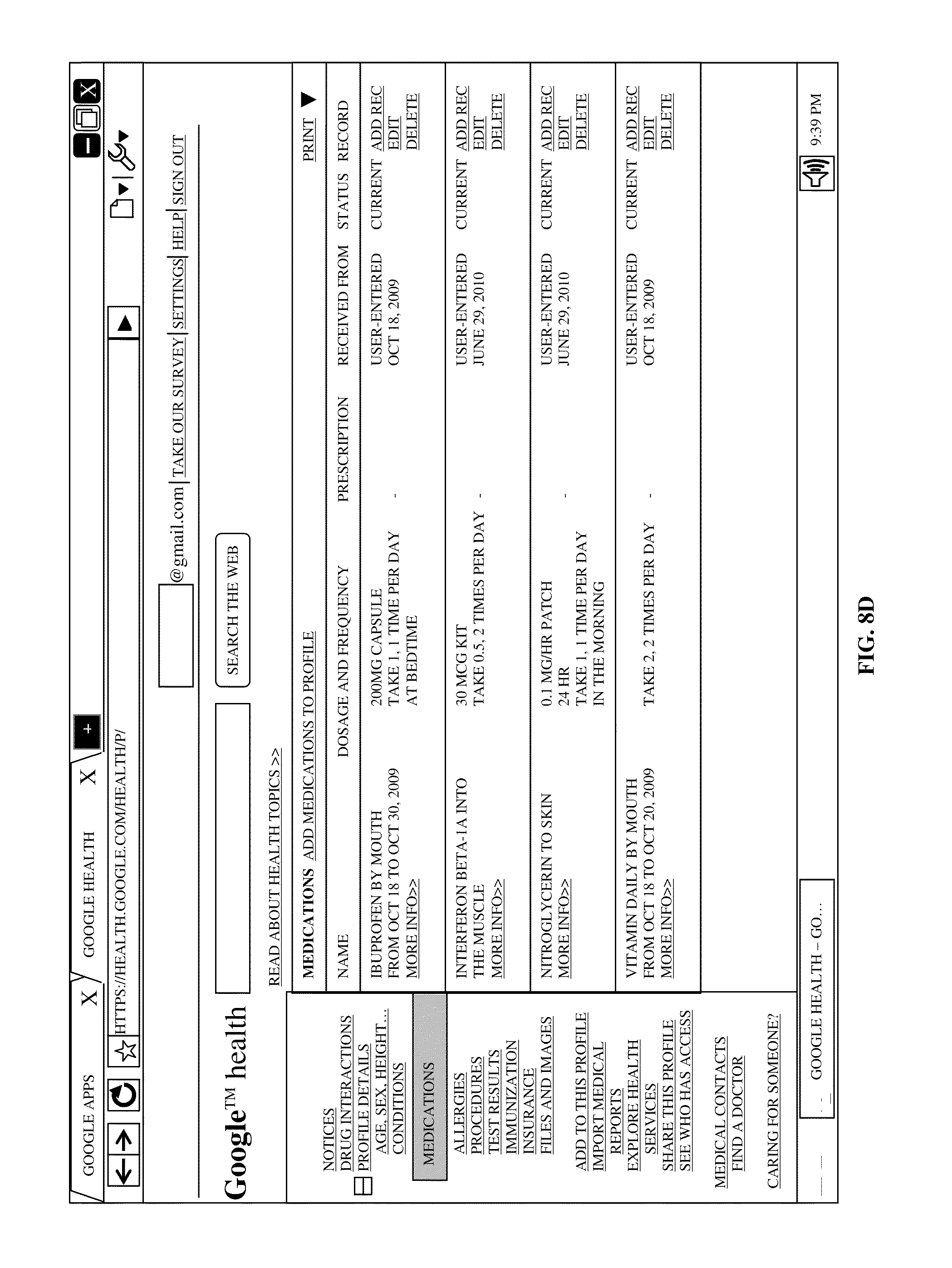
How Do I Get My Medicare Diabetes Supplies
You can order and pick up supplies from your pharmacy, or you can order them from a DME supplier.
About Insulin And Medicare Part D
Medicare Part B does not cover insulin unless you use an insulin pump that is considered medically necessary. It also does not cover insulin pens, syringes, needles, alcohol swabs, or gauze.
How long can you have Medicare Part B?
If you’ve had Medicare Part B for longer than 12 months , you can get a yearly “Wellness” visit to develop or update a personalized prevention plan based on your current health and risk factors. This includes:
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
Does Medicare cover diabetes?
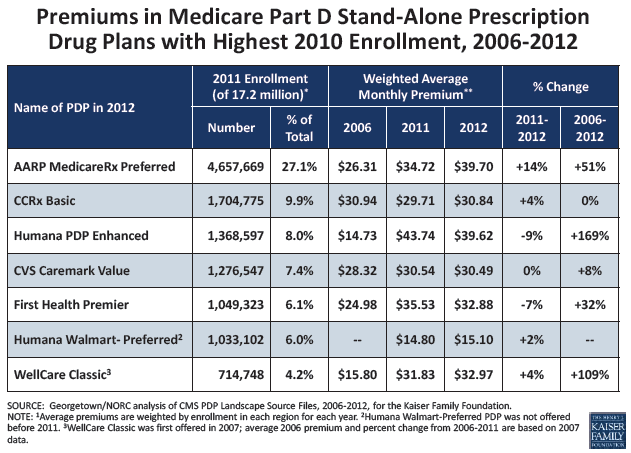
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
Does Part B cover insulin pumps?
Part B may cover insulin pumps worn outside the body (external), including the insulin used with the pump for some people with Part B who have diabetes and who meet certain conditions. Certain insulin pumps are considered durable medical equipment.
Does Medicare cover diabetic foot care?
Medicare may cover more frequent visits if you’ve had a non-traumatic ( not because of an injury ) amputation of all or part of your foot, or your feet have changed in appearance which may indicate you have serious foot disease. Remember, you should be under the care of your primary care doctor or diabetes specialist when getting foot care.
What is the Medicare Part B copayment?
For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What are the factors that affect Medicare Part B screening?
high blood pressure. history of high blood sugar. history of abnormal cholesterol levels. obesity. Medicare Part B also covers an annual diabetes screening if at least two of the following factors apply: a person is 65 years of age or older. a person has overweight. a person’s family has a history of diabetes.
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
What is the number to call for insulin pump?
For questions about Part B’s coverage of insulin and insulin pumps, a person can call 1-800-MEDICARE.
Does Medicare pay for glucose monitors?
In 2020, a person with Medicare Part B will pay 20% of the cost for diabetes self-management suppli es such as glucose monitors, lancets, and test strips. However, to ensure Medicare coverage, a person must get the prescription from their doctor, and use an in-network pharmacy or supplier.
Does Medicare cover diabetic supplies?
Share on Pinterest. Medicare may cover some diabetic supplies, including some preventive services. Medicare Part D, which is prescription drug coverage, may cover a person for some diabet ic supplies used for inhaling or injecting insulin.
Does Medicare pay for diabetic eye exams?
Costs of diabetic eye exams. If a person has original Medicare, they may pay 20% of the Medicare-approved amount for the eye doctor’s services. A Part B deductible may also apply. If the eye exam takes place in a hospital outpatient setting, a person may have to pay a copay.
What Diabetes Supplies Does Medicare Pay For?
There are 34.2 million Americans managing diabetes and an additional 88 million Americans who have prediabetes. That’s why diabetic supplies are covered by Medicare.
What Brand of Diabetic Testing Supplies Does Medicare Cover?
Wondering what brand of diabetic supplies is covered by Medicare? Major brands such as Contour Next, OneTouch, FreeStyle, and Accu-Check are all covered by Medicare.
How Do I Get Free Diabetic Supplies?
It’s no secret that diabetic supplies can get pricey. Buying glucose monitors, test strips, and insulin can add up fast. Thankfully Medicare has you covered — if you know how to get the right supplies.
How Do I Get My Diabetic Supplies Through Medicare?
To get diabetes supplies through Medicare, start by talking to your doctor. You’ll need a prescription for all your medications and supplies. Once you have a prescription, you can fill the prescription at your local pharmacy or find a local Medicare supplier.
What Diabetic Supplies are Covered by Medicaid?
Do you qualify for both Medicare and Medicaid? If you’re dual-eligible, you can get expanded coverage for your diabetes supplies.
What Are the Most Common Supplies Needed by People with Diabetes?
The most common diabetes supplies are covered by Medicare. These include:
How Do I Cope with Finding Out I Have Diabetes?
If you’ve recently received a diabetes diagnosis, take a big breath. It’s easy to feel overwhelmed, but you’re not alone. There are several ways you can cope with finding out you have diabetes and help you focus on maintaining your health.
Not all diabetic supplies are covered by Medicare
If you are new to Medicare you may be surprised to learn that not all diabetic supplies are covered by Medicare. Knowing which supplies are covered and where to get them will allow you to maximize your benefits and relieve any strain on your budget.
Diabetic supplies covered by original Medicare
When reviewing what’s covered and what’s not covered, it’s best to remember that Medicare was originally enacted to be a safety net and not a comprehensive solution to all health care costs.
Diabetic supplies covered by Part D
Many diabetics rely on Medicare Part D to help pay for their medications. While original Medicare doesn’t cover insulin and related supplies, a Part D plan will. But not all plans are created equal and you must compare plans to find the best benefits for your circumstances.
What is a copayment?
Copayment: The amount you personally are required to pay for a specific supply, medical service, or prescription drug. The copayment is “your share” of the cost, and is most commonly a set dollar amount rather than a percentage of a cost.
Does Medicare cover diabetes supplies?
If you’ve recently been diagnosed with diabetes, or are making the switch to Medicare, understanding the complexities of Medicare coverage for diabetes supplies can feel overwhelming. However, making sense of these details is vital to effectively finding and purchasing supplies for diabetes that will be covered by your Medicare insurance plan.
Can I get additional Medicare for diabetes?
If you have an additional insurance plan that serves as a supplement to Original Medicare, such as a Medigap policy, you may be eligible for additional coverage for diabetes-related services and supplies. Additionally, keep in mind that Medicare Advantage Plans (such as a PPO or HMO) and other Medicare health plans may implement different rules and restrictions in terms of diabetes supplies coverage. Individuals enrolled in these plans may also have extra benefits when compared to Original Medicare.