
What does APC stand for in Medicare?
What is Medicare APC? APC stands for Medicare’s ambulatory payment classification. Hospitals use Medicare APC codes to bill the federal government for hospital services given to Medicare and Medicaid patients.
What does APC stand for in payment?
- (1) Packaged APC payment if billed on the same claim as a HCPCS code assigned status indicator “S,” “T,” or “V.”
- (2) Composite APC payment if billed with specific combinations of services based on OPPS composite-specific payment criteria. ...
- (3) In other circumstances, payment is made through a separate APC payment. ...
What is Medicare optimum?
- Original Medicare will only pay 80 percent of the cost of doctor visits. With a Medicare Advantage plan you will pay a small copay for doctor visits.
- Original Medicare will only pay a certain amount per day for hospital stays up to 150 days. ...
- Medicare doesn’t cover regular vision exams, eyeglasses or contacts and it also doesn’t cover most dental care. ...
What is the CMS for Medicare?
The CARES Act also:
- Increases flexibility for Medicare to cover telehealth services.
- Authorizes Medicare certification for home health services by physician assistants, nurse practitioners, and certified nurse specialists.
- Increases Medicare payments for COVID-19-related hospital stays and durable medical equipment.
What is an APC code for Medicare?
Ambulatory Payment ClassificationsAPC Codes (Ambulatory Payment Classifications) APCs or Ambulatory Payment Classifications are the United States government's method of paying for facility outpatient services for the Medicare (United States) program.
What is an APC payment rate?
APC Payment Rate means CMS' hospital outpatient prospective payment system rate. The APC payment rate is specified in the Federal Register notices announcing revisions in the Medicare payment rates.
What is the purpose of an APC?
The APC protein acts as a tumor suppressor, which means that it keeps cells from growing and dividing too fast or in an uncontrolled way. It helps control how often a cell divides, how it attaches to other cells within a tissue, and whether a cell moves within or away from a tissue.
What does APC mean in medical terms?
A type of immune cell that boosts immune responses by showing antigens on its surface to other cells of the immune system. An APC is a type of phagocyte. Also called antigen-presenting cell.
What is the purpose of the ambulatory payment classification?
Ambulatory payment classification means a reimbursement method that categorizes outpatient visits into groups according to the clinical characteristics, the typical resource use, and the costs associated with the diagnoses and the procedures performed.
How are APC rates set?
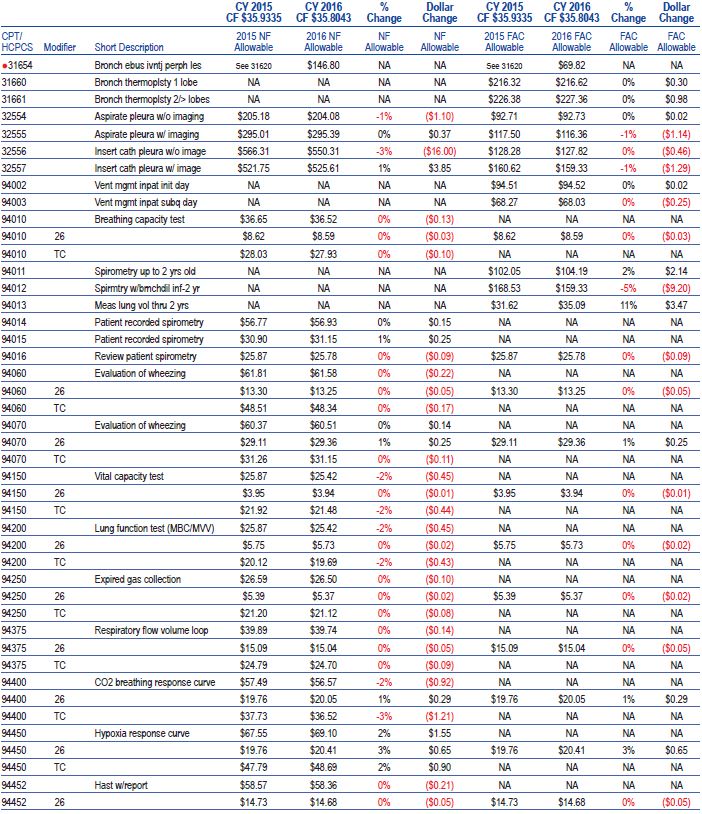
The payment rates for most separately payable medical and surgical services are determined by multiplying the prospectively established scaled relative weight for the service's clinical APC by a conversion factor (CF) to arrive at a national unadjusted payment rate for the APC.
How is Medicare APC payment calculated?
In order to calculate the wage adjusted payment, you must first separate the APC payment amount into 60 percent and 40 percent. For example: for CPT Code 70553, MRI brain w/o and w/dye, the APC payment amount is $506. Multiply the $506 amount by 60% = $304. Next, multiply the $506 amount by 40% = $202.
How is APC calculated?
Average propensity to consume is calculated by dividing an entity's consumption by the entity's total income. It is a ratio between what is spent and what is earned.
Which service is reimbursed based on the APC payment method?
CardsTerm DRGsDefinition Diagnosis related groups. Determine Medicare inpatient hospital reimbursement.Term Medicare reimbursable drugs are found in this code book?Definition HCPCS Level IITerm Which Service is reimbursed based on the APC payment method?Definition Patient X-ray of left foot in the outpatient department117 more rows•Mar 6, 2017
What is the difference between APC and DRG?
APCs are similar to DRGs. Both APCs and DRGs cover only the hospital fees, and not the professional fees, associated with a hospital outpatient visit or inpatient stay. DRGs have 497 groups, and APCs have 346 groups. APCs use only ICD-9-CM diagnoses and CPT-4 procedures.
What is an Advanced Practice Clinician (APC)?
Advanced practice clinicians are clinicians who are not doctors, but provide a role that is very similar to a doctor. Advanced practice clinicians typically refers to advanced practice registered nurses (APRNs) and to physician assistants (PAs).
Types of Advanced Practice Clinicians
While there are only two types of clinical doctors, doctors of medicine (MDs) and doctors of osteopathic medicine (DOs), there are several types of APCs. MDs and DOs function almost identically in the medical setting, but the many different types of APCs can work in very different roles.
What is an Ambulatory Payment Classification (APC)?
While the abbreviation APC in healthcare typically refers to advanced practice providers, it can also refer to ambulatory payment classification. Ambulatory payment classification is a system for billing the federal government for outpatient services provided to Medicare and Medicaid patients.
What is an APC code?
APC Codes (Ambulatory Payment Classifications) APCs or Ambulatory Payment Classifications are the United States government's method of paying for facility outpatient services for the Medicare (Uni ted States) program. A part of the Federal Balanced Budget Act of 1997 made the Centers for Medicare and Medicaid Services create a new Medicare ...
Where is APC paid?
APC payments are made to hospitals when the Medicare outpatient is discharged from the Emergency Department or clinic or is transferred to another hospital (or other facility) which is not affiliated with the initial hospital where the patient received outpatient services.
What is OPPS in Medicare?
A part of the Federal Balanced Budget Act of 1997 made the Centers for Medicare and Medicaid Services create a new Medicare "Outpatient Prospective Payment System " (OPPS) for hospital outpatient services -analogous to the Medicare prospective payment system for hospital inpatients known as Diagnosis-related group or DRGs.
What is a C code in Medicare?
Medicare created C codes for use by Outpatient Prospective Payment System (OPPS) hospitals. OPPS hospitals are not limited to reporting C codes, but they use these codes to report drugs, biologicals, devices, and new technology procedures that do not have other specific HCPCS Level II codes that apply.
What is CPT code?
The CPT ® code set, developed and maintained by the American Medical Association (AMA), is used to capture medical services and procedures performed in the outpatient hospital setting or to capture pro-fee services, meaning the work of the physician or other qualified healthcare provider.
What is the primary outpatient hospital reimbursement method?
However, the primary outpatient hospital reimbursement method used is the OPPS.
What is an ambulatory surgery center?
An ambulatory surgery center (ASC) is a distinct entity that operates to provide same-day surgical care for patients who do not require inpatient hospitalization. An ASC is a type of outpatient facility that can be an extension of a hospital or an independent freestanding ASC.
What is the official coding guidelines?
Official coding guidelines provide detailed instructions on how to code correctly; however, it is important for facility coders to understand that guidelines may differ based on who is billing (inpatient facility, outpatient facility, or physician office).
What is a patient registered?
1. Patient is registered by the admitting office, clinic, or hospital outpatient department. This includes validating the patient’s demographic and insurance information, type of service, and any preauthorization for procedures required by the insurance company, if not already completed prior to the visit. 2.
Do facility coders submit claims?
However, the facility coders also would submit claims to bring in reimbursement for the facility resources used (such as the room cost, nursing personnel, drugs, supplies, etc.), which is separate from the professional fee.
