
According to the new poll, 61 percent of Americans think Medicare is currently worth the costs. As many as 78 percent of Democrats and 57 percent of Independents say it is worth it, but just 45 percent of Republicans agree. Forty-four percent of Republicans say it's not worth it.
Full Answer
Do new Medicare plans have star ratings?
Star Ratings are also awarded for various discrete aspects of Medicare Part D and Medicare Advantage plans. New Medicare Part D or Medicare Advantage plans naturally do not have any historical information, so they will not have any Star or quality ratings for the first year.
What are the Medicare plan star ratings?
Plans are rated on a one-to-five scale, with one star representing poor performance and five stars representing excellent performance. Star Ratings are released annually and reflect the experiences of people enrolled in Medicare Advantage and Part D prescription drug plans.
How to use Medicare plan ratings?
Understanding the Medicare Star Rating
- Medicare rates Medicare Advantage and Part D (prescription drug plans) by stars.
- A 5-star rating is the best while a 1-star rating is the worst.
- Medicare takes a variety of variables into account when determining the rating, including plan participants’ ratings and member complaints.
What does Medicare star rating mean?
What Medicare star ratings mean. A Medicare star rating is a plan’s overall performance and quality score that's calculated across a wide range of criteria including customer satisfaction, access to health care and the rate of receiving preventative care.
Are seniors satisfied with Medicare?
Overall, the vast majority of adults 65 and older with Medicare coverage (94%) report being very satisfied or satisfied with the quality of their medical care and the availability of specialists.
Is Medicare a popular program?
Medicare remains one of the most popular of Federal programs.
Is Medicare more popular than Medicaid?
Similarly, about two-thirds (65 percent) know that Medicaid is the primary source of health insurance for low-income people, although nearly one in five (18 percent) say the program is Medicare, and about the same share (17 percent) say it's a different program or say they don't know.
What are the pros of Medicare for All?
Pros and Cons of Medicare for AllUniversal healthcare lowers healthcare costs for the economy overall, since the government controls the price of medication and medical services through regulation and negotiation.It would also eliminate the administrative cost of working with multiple private health insurers.More items...•
What do seniors think of Medicare?
Older Medicare recipients are happiest with their coverage. Nearly nine out of 10 people who are 80 years old or older say they're satisfied or very satisfied with Medicare. That's compared to 79% of people age 71 to 79, 71% of people 65-70 and 69% of those under 65.
How successful is the Medicare program?
Medicare's successes over the past 35 years include doubling the number of persons age 65 or over with health insurance, increasing access to mainstream health care services, and substantially reducing the financial burdens faced by older Americans.
Which is better PPO or HMO?
HMO plans typically have lower monthly premiums. You can also expect to pay less out of pocket. PPOs tend to have higher monthly premiums in exchange for the flexibility to use providers both in and out of network without a referral. Out-of-pocket medical costs can also run higher with a PPO plan.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
What is not covered by Medicaid?
Medicaid is not required to provide coverage for private nursing or for caregiving services provided by a household member. Things like bandages, adult diapers and other disposables are also not usually covered, and neither is cosmetic surgery or other elective procedures.
Why are Americans against universal healthcare?
Beyond individual and federal costs, other common arguments against universal healthcare include the potential for general system inefficiency, including lengthy wait-times for patients and a hampering of medical entrepreneurship and innovation [3,12,15,16].
What are the cons of Medicare for All?
Cons of Medicare for All:Providers can choose only private pay options unless mandated differently.Doesn't solve the shortage of doctors.Health insurance costs may not disappear.Requires a tax increase.Shifts costs of employer coverage.
How Medicare for All would hurt the economy?
The real trouble comes when Medicare for all is financed by deficits. With government borrowing, universal health care could shrink the economy by as much as 24% by 2060, as investments in private capital are reduced.
What are CMS Medicare star ratings based on?
Medicare star ratings are calculated using 40 criteria across Part C and Part D coverage. This includes survey data about member satisfaction, calc...
What does a CMS 5-star rating mean?
A 5-star Medicare plan has earned the best-possible rating for quality and performance. If a 5-star plan is available in your area, you can switch...
What is the highest rating for a Medicare Advantage plan?
A 5-star Medicare Advantage plan has the highest possible rating. Plans are ranked on a scale of 1 star to 5 stars. Only 16% of contracts have achi...
Can you get a $0 Medicare Advantage plan with 5-stars?
Yes, in 92% of the counties where 5-star plans are available, you can get a free Medicare Advantage plan that also has 5 stars. However, the cost o...
Why are star ratings important when choosing a Medicare plan?
Medicare star ratings tell you about a plan's quality and performance across a range of criteria. This can tell you the rate of customer satisfacti...
What does Medicare rating mean?
What the Ratings Mean. What Medicare Evaluates to Rate Quality. Medicare rates the quality of Medicare Advantage plans, which cover hospitalization, outpatient care, and often prescription-drug coverage. It also rates Part D drug plans, which help to pay for the cost of prescription medications for people not enrolled in a Medicare Advantage plan.
How to check Medicare plan ratings?
You can compare up to three plans at a time. Or you can call 800-MEDICARE (1-800-633-4227) to get a plan’s ratings.
What does Medicare evaluate to rate quality?
What Medicare Evaluates to Rate Quality. Medicare uses information from many sources to do the ratings. This includes surveys filled out by members of a health plan as well as required data reporting from the health plan. Medicare also uses information from health care providers.
What is Medicare based on?
In general, Medicare rates plans based on member health, member complaints, receipt of recommended care, and member satisfaction. Some of the factors used to rate plans may be important to your health and satisfaction with the plan, others less so.
Is 5 stars good or bad for Medicare?
Five stars is excellent. Four stars is above average. Three stars is average. Two stars is below average. One star is poor. Continued. If a plan has no rating, it's new. Or there might not be enough information for a rating to be done. Find a Medicare Plan that Fits Your Needs Get a Free Medicare Plan Review.
Key Takeaways
Medicare Star Ratings were developed to give people more information to consider when choosing a health or prescription drug plan.
Let's keep in touch
Subscribe to receive important updates from NCOA about programs, benefits, and services for people like you.
Top 5-star Medicare Advantage plans
Medicare Advantage plans with five stars are top-tier plans that are considered "excellent" by the Medicare's administering agency, the Centers for Medicare & Medicaid Services (CMS).
5-star special enrollment period
If a 5-star plan is available in your location, you qualify for a 5-star special enrollment period (SEP) that allows you to switch to a 5-star plan at any time during the year.
How Medicare star ratings are calculated
Each Medicare plan's overall star rating is a weighted average of several different data points. This means it's a robust measurement that can help you understand which are the best-performing Medicare plans in your area.
Frequently asked questions
Medicare star ratings are calculated using 40 criteria across Part C and Part D coverage. This includes survey data about member satisfaction, calculations about the number of complaints, outcomes such as how often those with diabetes fill their prescriptions and more.
Methodology
Data and analysis is based on Centers for Medicare & Medicaid Services (CMS) public use files, fact sheets and technical notes. Medicare Advantage analysis only includes plans that include prescription drug coverage and excludes employer-sponsored plans, special needs plans, PACE plans, sanctioned plans and health care prepayment plans (HCPPs).
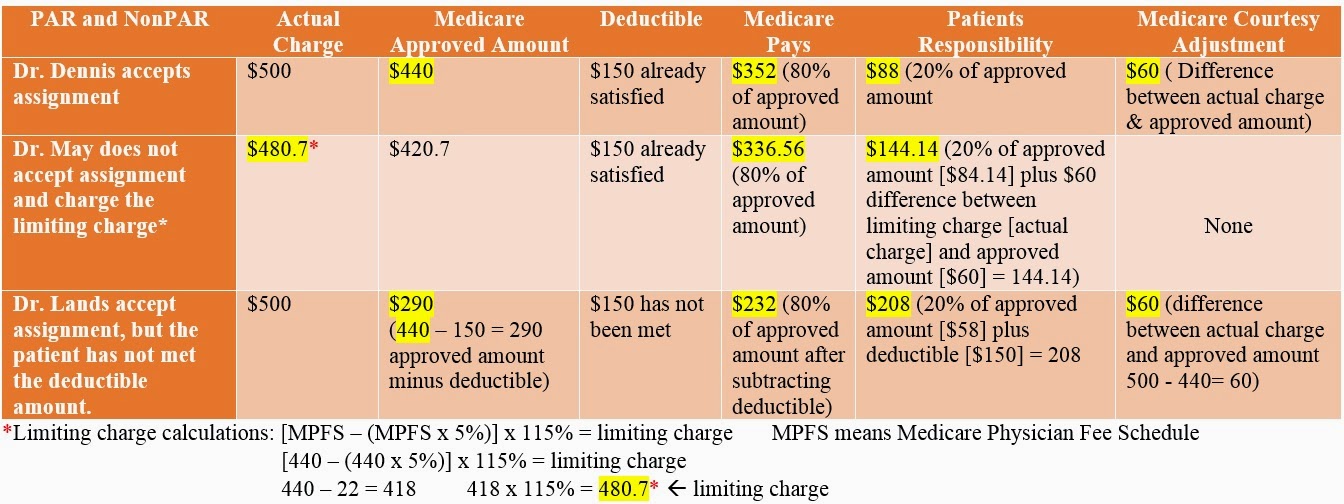
What is Medicare approved amount?
The Medicare-approved amount is the amount that Medicare pays your provider for your medical services. Since Medicare Part A has its own pricing structure in place, this approved amount generally refers to most Medicare Part B services. In this article, we’ll explore what the Medicare-approved amount means and it factors into what you’ll pay ...
What is Medicare Advantage?
Medicare Part B covers you for outpatient medical services. Medicare Advantage covers services provided by Medicare parts A and B, as well as: prescription drugs. dental.
What is a non-participating provider?
Nonparticipating provider. A nonparticipating provider accepts assignment for some Medicare services but not all. Nonparticipating providers may not offer discounts on services the way participating providers do. Even if the provider bills Medicare later for your covered services, you may still owe the full amount upfront.
How much is Medicare Part A deductible?
If you have original Medicare, you will owe the Medicare Part A deductible of $1,484 per benefit period and the Medicare Part B deductible of $203 per year. If you have Medicare Advantage (Part C), you may have an in-network deductible, out-of-network deductible, and drug plan deductible, depending on your plan.
What percentage of Medicare deductible is paid?
After you have met your Part B deductible, Medicare will pay its portion of the approved amount. However, under Part B, you still owe 20 percent of the Medicare-approved amount for all covered items and services.
What are the services covered by Medicare?
No matter what type of Medicare plan you enroll in, you can use Medicare’s coverage tool to find out if your plan covers a specific service, test, or item. Here are some of the most common Medicare-approved services: 1 mammograms 2 chemotherapy 3 cardiovascular screenings 4 bariatric surgery 5 physical therapy 6 durable medical equipment
What is excess charge for Medicare?
These excess charges can cost up to an additional 15 percent of the Medicare-approved amount. If you have a Medigap plan, this amount may be included in your coverage.
What does prior authorization mean?
Prior authorization means your doctor must get approval before providing a service or prescribing a medication. Now, when it comes to Advantage and Part D, coverage is often plan-specific. Meaning, you should contact your plan directly to confirm coverage.
Does Medicare require prior authorization?
Medicare Part A Prior Authorization. Medicare, including Part A, rarely requires prior authorization. If it does, you can obtain the forms to send to Medicare from your hospital or doctor. The list mostly includes durable hospital equipment and prosthetics.
Do you need prior authorization for Medicare Part B?
Part B covers the administration of certain drugs when given in an outpatient setting. As part of Medicare, you’ll rarely need to obtain prior authorization. Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form.
Does Medicare Advantage cover out of network care?
Unfortunately, if Medicare doesn’t approve the request, the Advantage plan typically doesn’t cover any costs, leaving the full cost to you.
Does Medicare cover CT scans?
If your CT scan is medically necessary and the provider (s) accept (s) Medicare assignment, Part B will cover it. Again, you might need prior authorization to see an out-of-network doctor if you have an Advantage plan.
What does it mean when your Medicare rating is lower?
Instead, a lower rating simply means that there may be better options available.
What does higher star rating mean?
Higher star ratings mean that a provider has either gone above and beyond the standard or that patient satisfaction is far greater for that provider compared to others.
What are the criteria used to measure quality?
The criteria used to measure quality include things like patient experience, but the ratings are also based on performance when measured against time. This means that things like readmission rates at hospitals, timeliness of care, and efficient use of medical imaging are all contributing factors to the facility’s overall star rating.
