What is Rx blue?
Blue MedicareRx (PDP) is a Prescription Drug Plan with a Medicare contract. Blue MedicareRx Value Plus (PDP) and Blue MedicareRx Premier (PDP) are two Medicare Prescription Drug Plans available to service residents of Connecticut, Massachusetts, Rhode Island, and Vermont.
What is Medicare D blue?
Medicare Part D is drug coverage that can help lower the costs of your current and future Medicare-covered medications. You can only enroll in a Part D plan offered by private insurance companies such as Blue Cross.
What is the annual deductible in 2022 for Blue Medicare Rx value?
How much is the deductible? $480.00 per year for Part D prescription drugs except for drugs listed on Tier 1 and Tier 2, which are excluded from the deductible. This plan doesn't have a deductible. After you pay your yearly deductible, you pay the following until your total yearly drug costs reach $4,430.
How many Medicare Part D stages are there for Blue Medicare Rx?
four stagesMedicare Part D coverage includes four stages: Deductible, Initial Coverage Stage, Coverage Gap (or Donut Hole) and Catastrophic Coverage. It's important to understand each stage and how they may affect what you pay for your prescription drugs.
What are the 4 prescription drug coverage stages?
Throughout the year, your prescription drug plan costs may change depending on the coverage stage you are in. If you have a Part D plan, you move through the CMS coverage stages in this order: deductible (if applicable), initial coverage, coverage gap, and catastrophic coverage.
What is the difference between Medigap and Part D?
The names “Medicare Plan D”, “Medicare Supplement Plan D”, and “Medigap Plan D all mean the same thing. But these plans are not the same thing as Medicare Part D, which is for prescription drug coverage. Medicare Supplement Plan D policies do not cover prescription drugs.
What is the maximum out-of-pocket for Medicare Part D?
Medicare Part D, the outpatient prescription drug benefit for Medicare beneficiaries, provides coverage above a catastrophic threshold for high out-of-pocket drug costs, but there is no cap on total out-of-pocket drug costs that beneficiaries pay each year.
Is Medicare going to do away with the donut hole?
The Part D coverage gap (or "donut hole") officially closed in 2020, but that doesn't mean people won't pay anything once they pass the Initial Coverage Period spending threshold. See what your clients, the drug plans, and government will pay in each spending phase of Part D.
How does Part D Medicare work?
You pay a monthly premium to an insurance carrier for your Part D plan. In return, you use the insurance carrier's network of pharmacies to purchase your prescription medications. Instead of paying full price, you will pay a copay or percentage of the drug's cost. The insurance company will pay the rest.
See plans side-by-side
Your prescriptions work for you; so should your Medicare prescription drug plan. Whether you take many or high-cost medications, just a few generics, or no medications at all – we have the plan for you.
The power of Blue
We’re powered by Blue Cross Blue Shield. Our Blue foundation helps us give the residents of New England more personalized prescription drug coverage.
Enroll the way you want
It’s quick and easy to enroll! You can sign up with Blue MedicareRx using the method you’re most comfortable with.
Lower costs with Extra Help
Are you on a fixed, limited income? If you qualify for Medicare Part D Extra Help, you’ll have a lower premium and pay less for your prescription drugs.
Want to enroll?
Blue Medicare Rx coverage is Medicare insurance that covers prescription drugs. Like most people, you probably know that the cost of prescription drugs is rising. This coverage makes it easier for you to fill your prescriptions by making them more affordable.
A company you can trust
BCBSNC offers dependable coverage for Medicare beneficiaries living in North Carolina. North Carolina is our home, and we’re its largest insurer. 3 We have over 70 years of experience in the health care industry, so you can count on our expertise and helpful service.
Quick facts about Blue Medicare Rx coverage
If you enroll for the first time this year, you may see your prescription drug costs drop by up to 50% 1
How long does it take to get a prescription from CVS?
Call Customer Care for specific pricing of your medications. Typically, you should expect to receive your prescription within 10 calendar days from the time the mail service pharmacy receives your order. Back
What are the stages of Medicare Part D?
Medicare Part D Coverage Stages & the Coverage Gap. Medicare Part D coverage includes four stages: Deductible, Initial Coverage Stage, Coverage Gap (or Donut Hole) and Catastrophic Coverage. It’s important to understand each stage and how they may affect what you pay for your prescription drugs. Learn more.
Compare Blue MedicareRx 2022
Blue MedicareRx has two plans that offer you comprehensive Medicare Part D coverage. Whether you take brand-name prescription medications or just a few generics, you can count on Blue for quality, affordable prescription drug plans.
See plans side-by-side
Answer three quick questions to help you get started. Based on your answers, we'll point out the plan you may want to consider.
What are the formulary tiers?
Formulary tiers. Tier. Description. Tier 1. Certain generic drugs that are available at the lowest copayment for our members. Tier 2. Higher cost generic drugs available at a higher copayment than Tier 1 generic drugs. Tier 3. Common brand-name and some higher cost generic drugs.
How far in advance do you have to notify Medicare about a change in medication?
If a change affects a drug you take, we will notify you at least 60 days in advance, as required by Medicare. Sometimes, we must remove a drug immediately for safety reasons or due to its discontinuation by the manufacturer. If a sudden removal occurs, we will notify our affected members as soon as possible.
What does "off label" mean?
Food and Drug Administration (FDA). Off-label drug use, which means using a drug for treatments not specifically mentioned on the drug’s label.
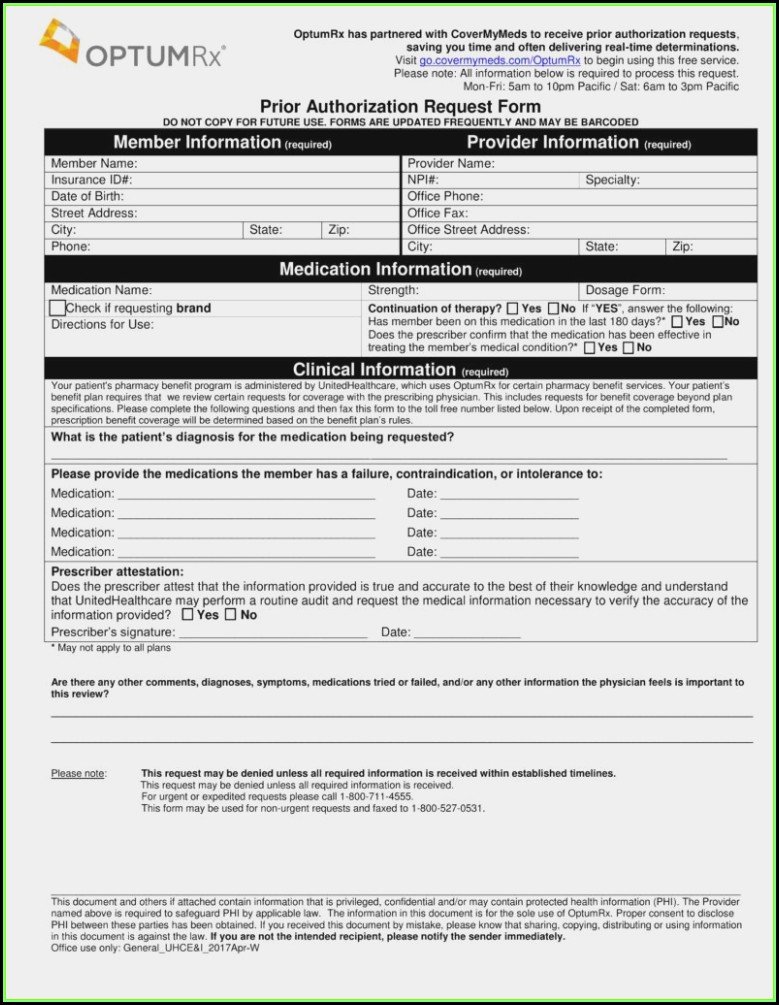
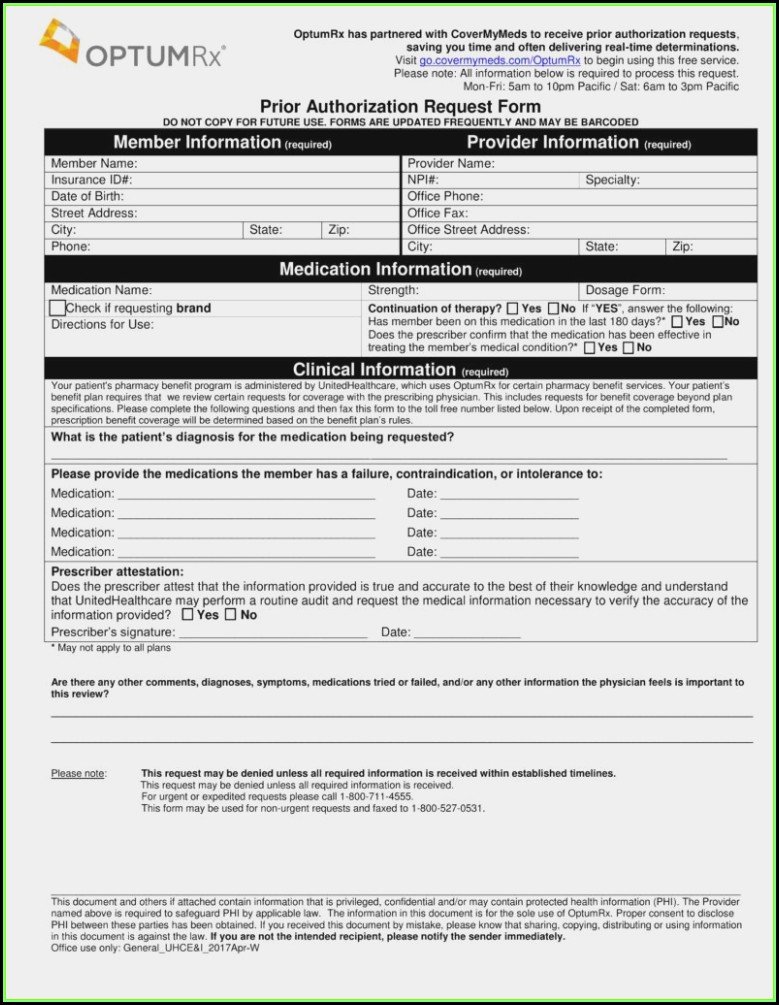
What are the requirements for a drug plan?
These requirements include: Prior authorization – you will need to obtain approval before you fill your prescription. Quantity limit – There is a limit to the amount of the drug the plan will cover with each prescription filled. Step therapy – You may be required to try an alternative drug before this drug is covered.
Can you remove a brand name from a drug list?
We may immediately remove a brand name drug on our Drug List if we are replacing it with a new generic drug that will appear on the same or lower cost sharing tier and with the same or fewer restrictions. Also, when adding the new generic drug, we may decide to keep the brand name drug on our Drug List, but immediately move it to a different cost-sharing tier or add new restrictions. We may not tell you in advance before we make that change-even if you are currently taking the brand name drug.
Is a lower tier drug cheaper than a higher tier?
Generally, a drug on a lower tier will cost less than a drug on a higher tier. If you’re interested in saving money on your prescriptions, discuss with your doctor whether switching to a similar drug on a lower tier might work for you.
Can you get a limited access prescription at a pharmacy?
Limited access – This prescription may be available only at certain pharmacies . If you believe your use of a drug meets all special requirements, or that you should be exempt from a requirement, you and/or your doctor must request a coverage determination before the plan will cover your drug.
Resources and Forms
Get essential resources for Medicare providers, including Medicare payer sheets, online provider manual and newsletters.
Medical Management Programs and Services
Get information on the programs and services designed to help maintain high quality care for Blue Medicare PPO and Blue Medicare HMO members.
Policies and Responsibilities
Review Blue Cross NC's Blue Medicare PPO and Blue Medicare HMO policies and provider responsibilities to our Medicare members.
Prior Plan Approval
Find out which services need prior plan approval and how to request it.
Provider Appeals
Get details and instructions for filing a post-service provider appeal.
Electronic Commerce
Connect with other providers online to research claims, benefits and eligibility information.
Contact Us
Questions about providing care for Blue Medicare PPO and Blue Medicare HMO members? Contact us for answers.