What drugs are covered in Part D?
- Oral cancer drugs: Medicare helps pay for some oral cancer drugs you take by mouth if the same drug is available in injectable form or the drug is a prodrug ...
- Oral anti-nausea drugs: Medicare helps pay for oral anti-nausea drugs used as part of an anti-cancer chemotherapeutic regimen if they’re administered before, at, or within 48 hours of chemotherapy or ...
- Self-administered drugs in hospital outpatient settings: Medicare may pay for some self-administered drugs, like drugs given through an IV. ...
What are the rules of Medicare Part D?
What it means to pay primary/secondary
- The insurance that pays first (primary payer) pays up to the limits of its coverage.
- The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover.
- The secondary payer (which may be Medicare) may not pay all the uncovered costs.
What plans are available for Medicare Part D?
- Monthly premiums
- Annual deductible (maximum of $445 in 2021)
- Copayments (flat fee you pay for each prescription)
- Coinsurance (percentage of the actual cost of the medication)
What is included in Medicare Part D?
Part D — Prescription drugs. This is the part of Medicare that pays for some of your prescription drugs. You buy a Part D plan through a private insurer. Each generally has premiums and other out-of-pocket costs, either flat copays for each medication or a percentage of the prescription costs. It also may have an annual deductible.
What is covered under Medicare Part D?
The Medicare Part D program provides an outpatient prescription drug benefit to older adults and people with long-term disabilities in Medicare who enroll in private plans, including stand-alone prescription drug plans (PDPs) to supplement traditional Medicare and Medicare Advantage prescription drug plans (MA-PDs) ...
What is not covered under Medicare Part D?
Drugs not covered under Medicare Part D Weight loss or weight gain drugs. Drugs for cosmetic purposes or hair growth. Fertility drugs. Drugs for sexual or erectile dysfunction.
Is Medicare Part D worth getting?
Most people will need Medicare Part D prescription drug coverage. Even if you're fortunate enough to be in good health now, you may need significant prescription drugs in the future. A relatively small Part D payment entitles you to outsized benefits once you need them, just like with a car or home insurance.
Do Part D plans have to cover all drugs?
Part D plans are required to cover all drugs in six so-called “protected” classes: immunosuppressants, antidepressants, antipsychotics, anticonvulsants, antiretrovirals, and antineoplastics.
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
What is a tier in prescription drug coverage?
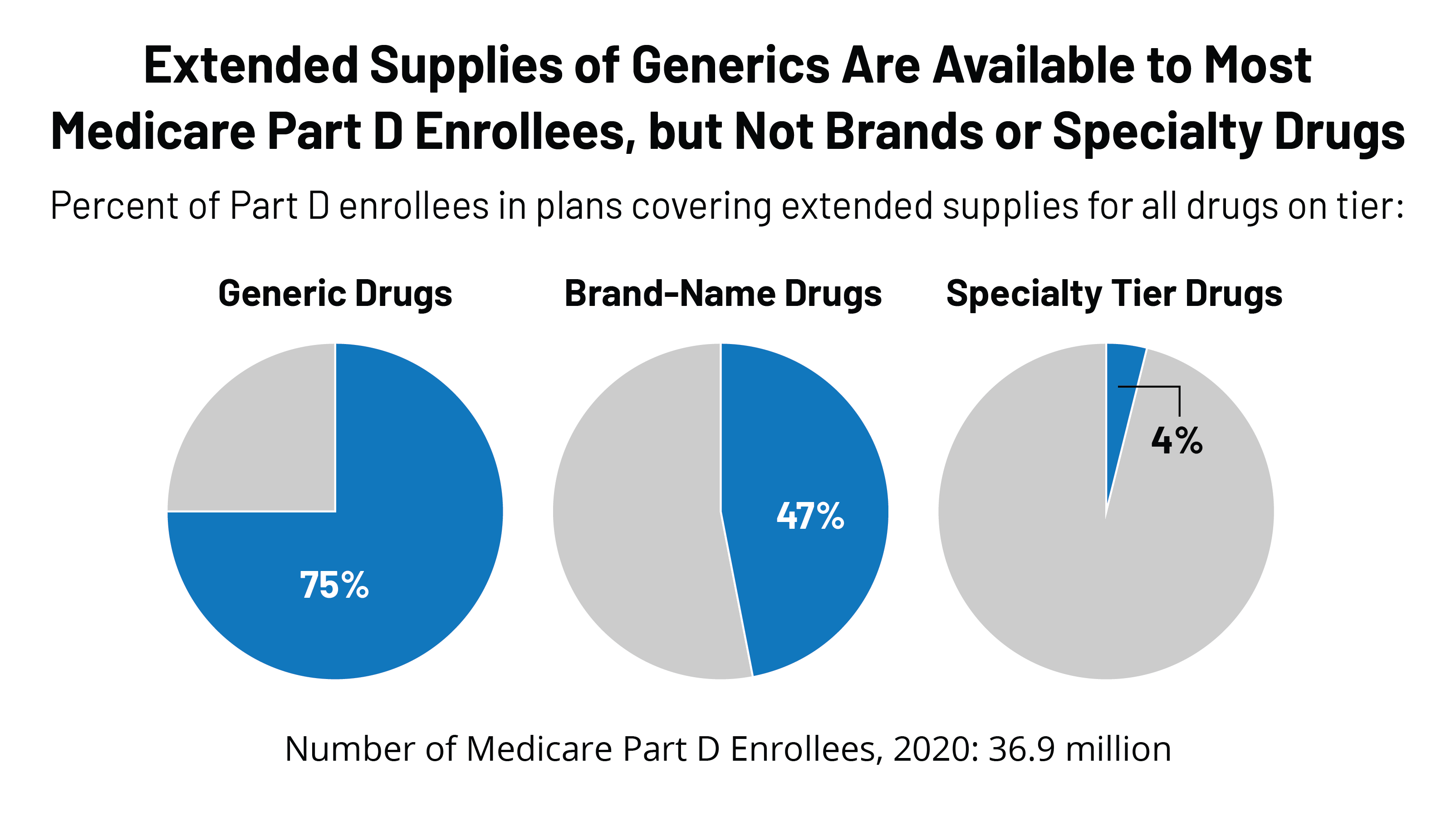
Tiers. To lower costs, many plans offering prescription drug coverage place drugs into different “. tiers. Groups of drugs that have a different cost for each group. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. ” on their formularies. Each plan can divide its tiers in different ways.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
What are the tiers of Medicare?
Here's an example of a Medicare drug plan's tiers (your plan’s tiers may be different): Tier 1—lowest. copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug.
What drugs are covered by Part D?
Drugs covered by each Part D plan are listed in their “formulary,” and each formulary is generally required to include drugs in six categories or protected classes: antidepressants, antipsychotics, anticonvulsants, immunosuppressants for treatment of transplant rejection, antiretrovirals, and antineoplastics.
How to decide if you need Medicare Part D?
How To Decide If You Need Part D. Medicare Part D is insurance. If you need prescription drug coverage, selecting a Part D plan when you’re eligible to enroll is probably a good idea—especially if you don’t currently have what Medicare considers “creditable prescription drug coverage.”. If you don’t elect Part D coverage during your initial ...
What is Medicare Part D 2021?
Luke Brown. Updated July 15, 2021. Medicare Part D is optional prescription drug coverage available to Medicare recipients for an extra cost. But deciding whether to enroll in Medicare Part D can have permanent consequences—good or bad. Learn how Medicare Part D works, when and under what circumstances you can enroll, ...
How long can you go without Medicare Part D?
You can terminate Part D coverage during the annual enrollment period, but if you go 63 or more days in a row without creditable prescription coverage, you’ll likely face a penalty if you later wish to re-enroll. To disenroll from Part D, you can: Call Medicare at 1-800-MEDICARE.
How long do you have to be in Medicare to get Part D?
You must have either Part A or Part B to get it. When you become eligible for Medicare (usually, when you turn 65), you can elect Part D during the seven-month period that you have to enroll in Parts A and B. 2. If you don’t elect Part D coverage during your initial enrollment period, you may pay a late enrollment penalty ...
How to disenroll from Medicare?
Call Medicare at 1-800-MEDICARE. Mail or fax a letter to Medicare telling them that you want to disenroll. If available, end your plan online. Call the Part D plan directly; the issuer will probably request that you sign and return certain forms.
What happens if you don't have Part D coverage?
The late enrollment penalty permanently increases your Part D premium. 3. Prescription drug coverage that pays at least ...
What is Part D insurance?
Part D coverage is generally provided through a network of pharmacies that are contracted with the Part D insurance provider . Network pharmacies generally include retail pharmacies and may include mail-order pharmacies as well. You will generally be required to fill your prescription at in-network pharmacies.
When does Medicare Part D start?
If you are turning 65, your Initial Enrollment Period for Part D coverage coincides with your general Medicare Initial Enrollment Period, which is the 7-month period that starts 3 months before the month you turn 65.
How long do you have to enroll in Part D if you have creditable coverage?
If you are eligible to defer enrollment penalty-free because you have creditable coverage, you must enroll in a Part D plan within 63 days of losing creditable drug coverage to avoid penalties. This a one-time Special Enrollment Period (SEP) where you can select a new Medicare prescription drug plan (PDP or MA-PD). If you miss this SEP you must enroll during the Annual Enrollment Period.
How long do you have to wait to enroll in Part D?
If at any point after you are first eligible for Part D, you have a continuous period of 63 days where you do not have ‘creditable drug coverage’ you will have to pay a Late Enrollment Penalty.
Does Medicare Part D have to be separately purchased?
Part D provides prescription drug coverage and needs to be separately purchased as Original Medicare does not provide drug coverage . Read this article to understand how Part D works with your Medicare.
Does Medicare cover prescription drugs?
Medicare Part D helps to cover prescription drug costs. Part D providers are required to have 2 drugs for each of the key most commonly prescribed drug classes for the Medicare population . However, drug lists (or ‘formularies’) can be different across different providers so it is always worthwhile checking your drug plan every year to make sure you are paying the least.
What is Medicare Part D?
Part D covers medications you get at your local pharmacy, mail order, or other pharmacies. You must be enrolled in either Medicare Part A or Part B to join a Part D plan, and individual Part D plans offer different levels of coverage. The plan you choose will determine how much you pay.
What are the requirements for Medicare Part D?
Part D eligibility requirements are the same as those for original Medicare and include those who: 1 are age 65 or older 2 have received Social Security disability payments for at least 24 months 3 have a diagnosis of amyotrophic lateral sclerosis (ALS) 4 have a diagnosis of end stage renal disease (ESRD) or kidney failure 5 have received Social Security disability for at least 24 months
What is coinsurance in Medicare?
Coinsurance. Coinsurance costs are determined by the specific plan you choose and in which tier your individual medication is placed. Coinsurance will be a percentage of the cost of a medication. After you have met your deductible, you’ll begin paying this fee if the Part D plan you choose requires it.
How many tiers are there in Medicare?
The medications at the bottom of the pyramid are less expensive and the ones at the very top are the most expensive. Most plans have four to six tiers. Medicare part d tier system. Here’s how a formulary tier system works:
How long do you have to be on Social Security to get Medicare Part D?
have a diagnosis of end stage renal disease (ESRD) or kidney failure. have received Social Security disability for at least 24 months. You can buy either a standalone Part D drug plan based on your medication needs or you can get Part D coverage through Medicare Advantage (Part C) plans.
How much is the deductible for Part D 2021?
Deductible. In 2021, guidelines say the deductible can’t be more than $445 for any Part D plan. You can choose plans that have $0 deductible based on the medications you take. For example, some Part D plans offer tier 1 and 2 medications with no deductible.
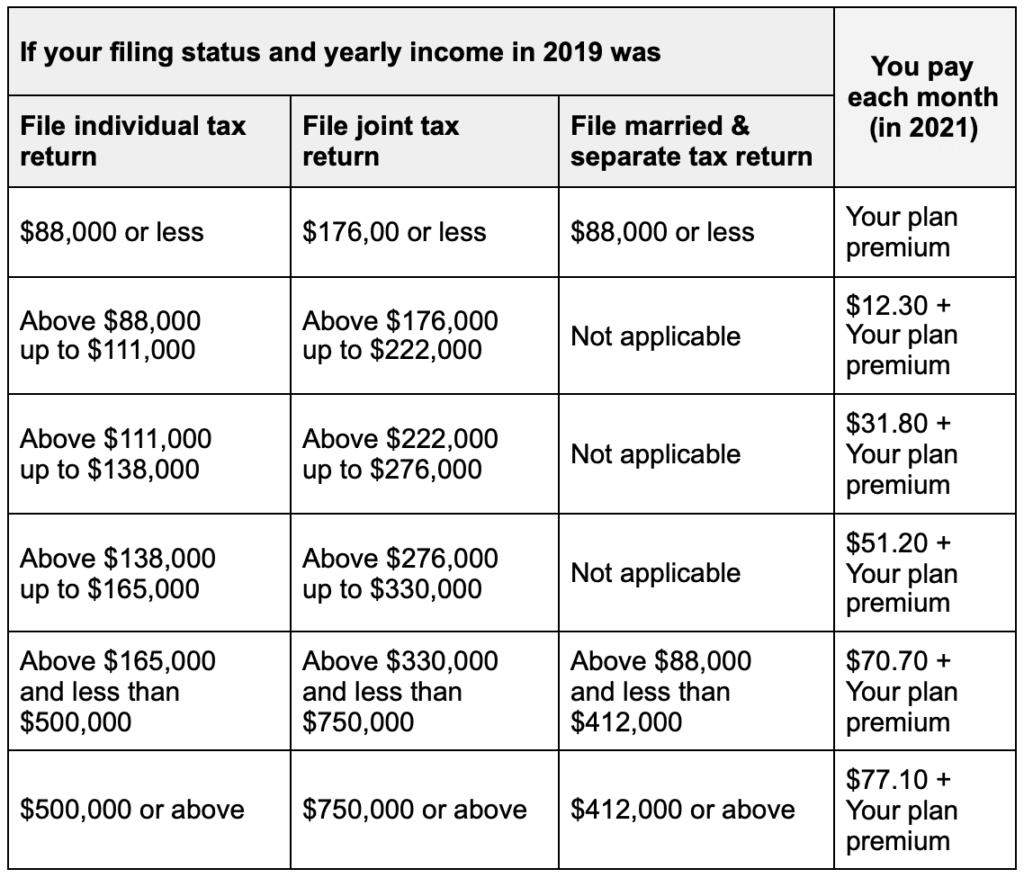
What are the factors that determine the cost of Medicare Part D?
There are several factors that determine how Part D costs are calculated, including out-of-pocket costs such as deductibles, premiums, coinsurance, and copayments. In addition to these costs, Part D has a premium in addition to the premiums you pay for your original Medicare parts.
