Dual Eligible Special Needs Program (D-SNP)
- Dually Eligible Recipients. Dual-Eligible recipients are individuals who receive both Medicare and Medicaid benefits. ...
- Overview of Dual Eligible Special Needs Plans. ...
- Eligibility for D-SNP. ...
- Benefits of D-SNP. ...
- Services Offered. ...
- Nevada Plans. ...
Does dsnp have drug coverage?
May 13, 2020 · People who have dual eligibility status can sign up for a type of Special Needs Plans known as a Dual-eligible Special Needs Plan, or DSNP. DSNPs are specialized Medicare Advantage plans that provide healthcare benefits for beneficiaries that have both Medicare and Medicaid coverage. Most DSNPs are categorized as either HMOs (Health Maintenance …
When can I enroll in a dsnp?
Dual Eligible Special Needs Plans (D-SNPs) Dual Eligible Special Needs Plans (D-SNPs) enroll individuals who are entitled to both Medicare (title XVIII) and medical assistance from a state plan under Medicaid (title XIX). States cover some Medicare costs, depending on the state and the individual’s eligibility.
What does dsnp stand for?
Oct 05, 2021 · What is a Dual-eligible Special Needs Plan (DSNP)? DSNPs are special types of Medicare Advantage plans that limit membership dual-eligible beneficiaries. Most DSNPs are categorized as HMOs (Health Maintenance Organizations), but some are PPOs (Preferred Provider Organizations).
What are dual special needs plans dsnp?
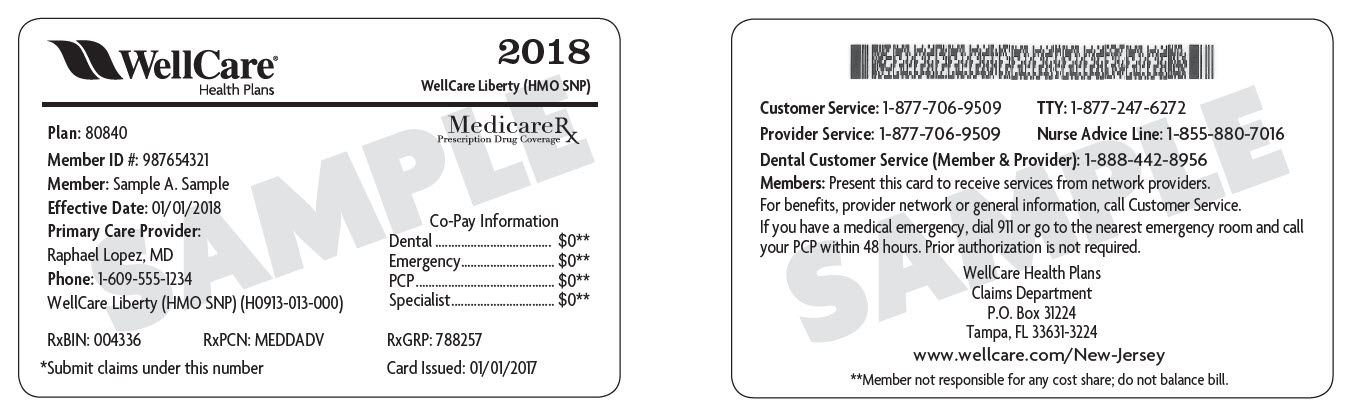
A dual-eligible special needs plan (DSNP) is for those who carry both a Medicare and a Medicaid card. If you’re receiving benefits from both programs, you may be eligible to receive benefits from a DSNP as well. Each state determines which DSNPs are available and what benefits are provided. DSNPs may include:
What are the features of a Dsnp?
A DSNP plan will include coverage for hospital services (Medicare Part A), medical health care needs (Medicare Part B), and prescription drugs (Medicare Part D) through a single plan. With a DSNP there may also be social services available to help coordinate a beneficiaries Medicare and Medicaid benefits.
What is the difference between SNP and D-SNP?
Institutional SNP (I-SNP): For those who live in an institution such as a nursing home or require nursing care at home. Dual-Eligible SNP (D-SNP): For those with both Medicare and Medicaid.
What are D-SNP benefits?
Dual Eligible Special Needs Plans (D-SNPs) are Medicare Advantage (MA) health plans which provide specialized care and wrap-around services for dual eligible beneficiaries (eligible for both Medicare and Medicaid).Jan 5, 2022
What are dual special needs plans Dsnp )?
A dual special needs plan is a type of health insurance plan. It's for people who have both Medicaid and Medicare. If that's you, you're “dual-eligible.” (That's just another way of saying you can have Medicaid and Medicare at the same time).
What is the difference between Dsnp and MMP?
An MMP is an alignment initiative in which Medicare and Medicaid benefits are offered as a single plan in a three-way contract between CMS, the state Medicaid agency (SMA), and the health plan; a D-SNP model is when a health plan holds a contract with Medicare and then a separate contract with the SMA to provide ...
Which statement best describes a Dsnp?
Which statement best describes a DSNP? The consumer states they currently pay a percentage of charges when they receive medical care. This means: The consumer is not likely to be a Full Dual-Eligible and may be better suited for enrollment in another type of plan.
What is the difference between an IEP and Icep?
The ICEP is a Medicare Advantage enrollment period as defined in Chapter 2 of the Medicare Managed Care Manual. The IEP is a drug benefit enrollment period as defined in Chapter 3 of the Medicare Prescription Drug Benefit Manual.
Do Dsnp members have subsidized premiums and cost sharing?
If a member loses their Medicaid eligibility, they move into a “deemed” eligibility status for DSNP for six months. During this grace period, the member is responsible for the Medicare cost-sharing portion, which includes copayments, coinsurance, deductibles and premiums.Jan 1, 2021
What is feh in Medicare?
The decision to enroll in Medicare Part B, while maintaining your Federal Employee Health Benefits (FEHB) in retirement, is one of the most difficult choices a new retiree faces.Oct 12, 2017
Can you have both Medi-Cal and Medicare?
People who qualify for both Medicare and full Medi-Cal are known as “dual eligibles” or “Medi-Medis.”
How does CMS ensure plans are compliant with Medicare regulations?
CMS will also conduct targeted market conduct examinations, as necessary, and respond to consumer inquiries and complaints to ensure compliance with the health insurance market reform standards. CMS will work cooperatively with the state to address any concerns.
Which of the individuals below would not likely have the authority to enroll a consumer in a Medicare Advantage plan?
Which of the individuals below would not likely have the authority to enroll a consumer in a Medicare Advantage Plan? The consumer's spouse, who is neither a Power of Attorney or legal guardian.
Medicaid Eligibility Categories
The Medicaid eligibility categories encompass all categories of Medicaid eligibility including:
D-SNPs With or Without Medicare Zero-Dollar Cost Sharing
At the time of plan creation, each D-SNP must identify whether or not if offers Medicare zero-dollar cost sharing. In HPMS, D-SNPs will have the option of one of the following two indicators:
Added DSNP benefits at no extra cost!
A dual-eligible special needs plan (DSNP) is for those who carry both a Medicare and a Medicaid card. If you’re receiving benefits from both programs, you may be eligible to receive benefits from a DSNP as well. Each state determines which DSNPs are available and what benefits are provided. DSNPs may include:
Part D coverage
A DSNP may also work as a prescription drug plan, covering many prescriptions where Medicare Part D is accepted.
Gym memberships
Medicare wants you to stay healthy. Some DNSPs give you access to gym memberships for keeping active.
What are D-SNPs?
D-SNPs are a type of Medicare Advantage (MA) Special Needs Plan. Most D-SNPs are health maintenance organization (HMO) plans, though some are preferred provider organization (PPO) plans. There are five types of D-SNPs: All-Dual, Full-Benefit, Medicare Zero Cost Sharing, Dual Eligible Subset, and Dual Eligible Subset Medicare Zero Cost Sharing.
Who Qualifies for D-SNPs?
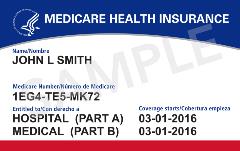
Dual-eligibles, individuals of any age who are eligible for both Medicare and Medicaid, qualify for D-SNPs.
When Can You Sell D-SNPs?
Even though D-SNPs are MA plans, they have no set enrollment period. Why? Because when someone becomes eligible for a D-SNP, they qualify for a Special Enrollment Period (SEP) to join one.
Where Can You Find D-SNP Prospects?
D-SNP prospects are all around you, especially if you work near an urban or generally low-income area. If you sell near a large rural area, it will be more difficult to find prospects because CMS won’t allow D-SNPs in counties that don’t have a certain number of doctors.
How Can You Build Your D-SNP Business?
To build your D-SNP book of business, you’ll want to focus your efforts on two main objectives: utilizing grassroots marketing and providing superior customer service.
How Can You Retain D-SNP Clients?
The fact that dual-eligibles can join or switch D-SNPs every calendar quarter can be a double-edged sword. On one hand, it gives you the opportunity to find new MA clients anytime throughout the year. On the other, it gives other agents the opportunity to simultaneously swoop in and steal your clients.
Why Sell D-SNPs?
You’ve learned that selling D-SNPs can earn commissions during Medicare’s off-season, but there’s one point we need to make clear: If you’re only interested in selling these products for your own profit, you may quickly find that you’re not working in the right market.
How long is the grace period for Medicare?
The grace period is at least one month long, but plans can choose to have a longer grace period. If you lose eligibility for the plan, you'll have a Special Enrollment Period to make another choice. This Special Enrollment Period starts when your Medicare SNP notifies you that you're no longer eligible for the plan.
What happens if you don't have Medicare?
If you don't have both Medicare and Medicaid (or get other help from your state paying your Medicare premiums), your exact costs will vary depending on the plan you choose. In general, you'll pay the basic costs of having a Medicare Advantage plan . expand.
What is Medicare SNP?
Medicare SNPs are a type of Medicare Advantage Plan (like an HMO or PPO). Medicare SNPs limit membership to people with specific diseases or characteristics. Medicare SNPs tailor their benefits, provider choices, and drug formularies to best meet the specific needs of the groups they serve. Find out who can join a Medicare SNP.
What is Medicare and Medicaid?
If you have Medicare and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid.
What is end stage renal disease?
End-Stage Renal Disease (Esrd) Permanent kidney failure that requires a regular course of dialysis or a kidney transplant. and need out-of-area dialysis. Medicare SNPs typically have specialists in the diseases or conditions that affect their members.