
Partial dual eligible coverage
| Program | Eligibility | Benefits |
| Qualified Medicare Beneficiary (QMB) Pro ... | Monthly income limit: $1,084 for an indi ... | Helps pay for Part A and/or Part B premi ... |
| Specified Low-Income Medicare Beneficiar ... | Monthly income limit: $1,296 for an indi ... | Helps pay for Part B premiums |
| Qualifying Individual (QI) Program | Monthly income limit: $1,456 for an indi ... | Helps pay for Part B premiums |
| Qualified Disabled Working Individual (Q ... | Monthly income limit: $4,339 for an indi ... | Pays the Part A premium for certain peop ... |
How to qualify for Medicare and Medicaid as dual eligibility?
You may be eligible to qualify for a dual eligible plan if:
- You qualify for Medicaid in your state
- You qualify for Medicare Parts A and B (Original Medicare)
- You live in the dual-eligible plan’s coverage area
What does it mean to be duel eligible?
There are several levels of assistance an individual can receive as a dual eligible beneficiary. The term “full dual eligible” refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as “partial dual eligible.”
What is full benefit dual eligible?
dual-eligible beneficiaries: People who are jointly enrolled in Medicare and Medicaid and who are eligible to receive benefits from both programs. All dual-eligible beneficiaries qualify for full Medicare benefits, which cover their acute and postacute care.
What does full dual eligible mean?
full duals: Dual-eligible beneficiaries who qualify for full benefits from Medicaid as well as from Medicare. Thus, Medicaid pays for their premiums for Part B of Medicare (and for Part A, if applicable) and covers various health care services that Medicare does not cover, such as most types of long-term services and supports (as well as dental care and other services in some states).
Can I have dual coverage with Medicare?
If you qualify for both Medicare and Medicaid, you are considered "dual eligible." Sometimes the two programs can work together to cover most of your health care costs. Individuals who are dual eligible can often qualify for special kinds of Medicare plans.
What are dual benefits?
You can have both Medicare and Medicaid at the same time If so, they could be “dual eligible.” That's where dual special needs plans — or “dual” plans — come in. Dual plans work together with the individual's Medicaid plan. Dual health plans cover eligible doctor visits, hospital stays and prescription drugs.
What is a partial dual eligible?
“Partial dual eligible” is a term used to describe Medicare beneficiaries who receive financial assistance for certain Medicare costs from their state Medicaid program. These individuals don't qualify for full Medicaid benefits from their state, like long-term services and supports or behavioral health services.
What is a dual coverage?
If you are covered under two different dental insurance plans, then you have dual dental coverage. Dual dental coverage typically occurs when you have two jobs that each provide dental benefits, or you are covered by your spouse's dental plan in addition to your own.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Can you have Medicare and Medicaid at the same time?
Yes. A person can be eligible for both Medicaid and Medicare and receive benefits from both programs at the same time.
Which patient would be considered dual eligible for federal health care resources quizlet?
Who are the "dual eligible"? Individuals who are eligible for Medicare and Medicaid. Medicare is provided without cost to the Medicare beneficiary. You just studied 20 terms!
What is United Healthcare Dual Complete?
A UnitedHealthcare Dual Complete plan is a DSNP that provides health benefits for people who are “dually-eligible,” meaning they qualify for both Medicare and Medicaid. Who qualifies? Anyone who meets the eligibility criteria for both Medicare and Medicaid is qualified to enroll in a DSNP.
What is a dual SNP plan?
Dual Eligible Special Needs Plans (D-SNPs) are Medicare Advantage (MA) health plans which provide specialized care and wrap-around services for dual eligible beneficiaries (eligible for both Medicare and Medicaid).
What is a dual provider?
Dual eligibles are recipients who have Medicare and Medicaid coverage. Medicaid will reimburse the provider an amount up to the full amount of Medicare's statement of liability for co-insurance and deductible for the beneficiary.
Which insurance is primary when you have two?
If you have two plans, your primary insurance is your main insurance. Except for company retirees on Medicare, the health insurance you receive through your employer is typically considered your primary health insurance plan.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
How to get dual eligibility for Medicare?
How Do I Get Dual Eligibility? To become dual eligible for both Medicare and Medicaid, you will first need to be enrolled in Medicare. You are not required to be enrolled in every part of Original Medicare or a Medicare Advantage plan, but signing up for Medicare benefits beyond Part A hospital insurance is ok to do.
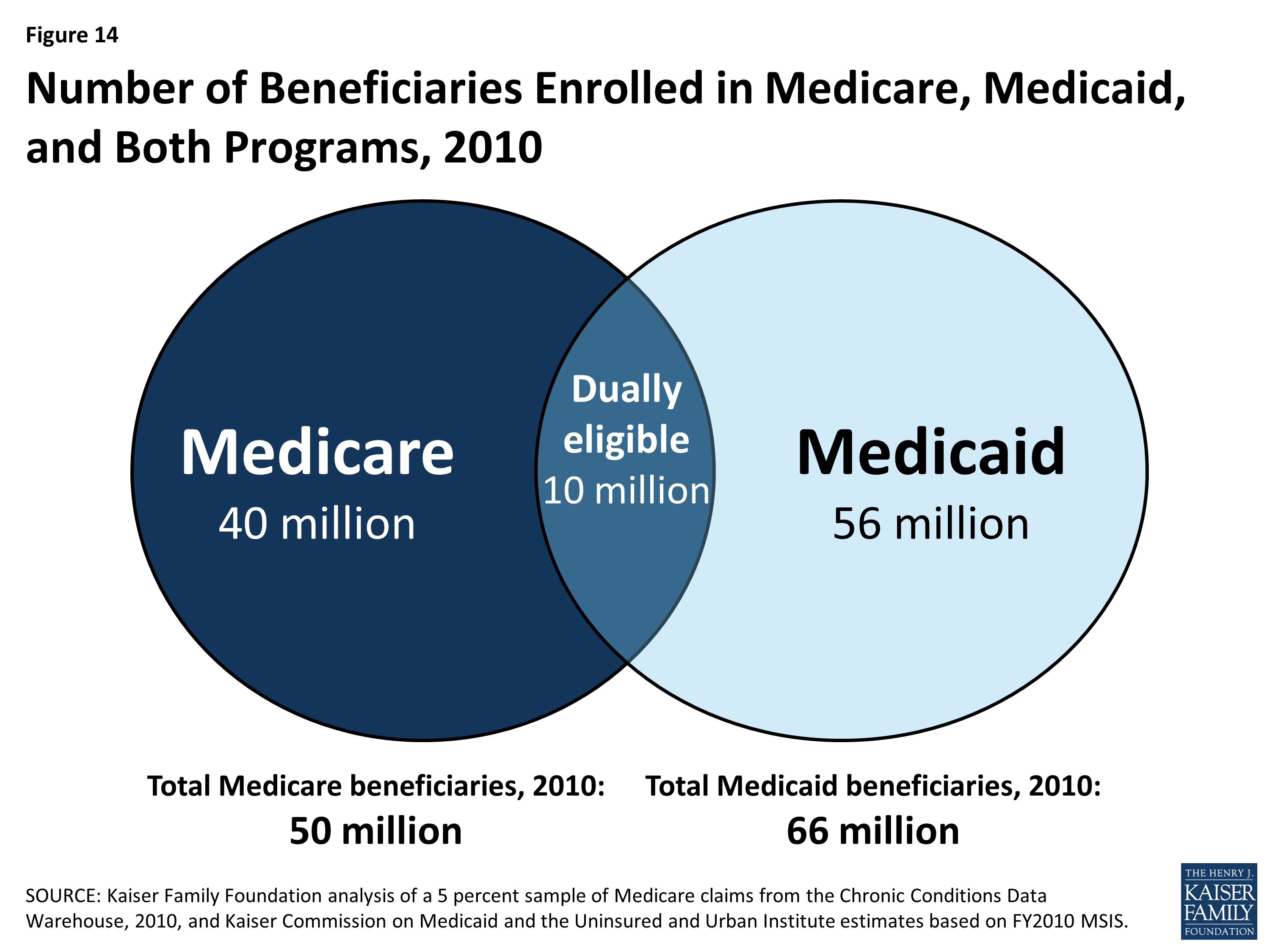
How many people are dual eligible for Medicare?
If you are dually eligible for both programs, most of your health care expenses will likely be covered, leaving you with a smaller (or no) bill to foot for the care you need. About 9 million people in the United States have dual eligibility for Medicare and Medicaid.
What is dual eligibility?
Dual eligibility is the term used to explain that you qualify for both Medicare and Medicaid benefits. This usually occurs in situations where you already qualify for Medicare but because of low income, cannot afford the remaining costs such as deductibles or your portion of the medical bills. If you are dually eligible for both programs, most ...
What is the difference between Medicare and Medicaid?
This avenue allows beneficiaries to customize their health insurance needs. Medicaid is a state program that helps low-income individuals and families with the costs of healthcare.
How does medicaid work?
How Medicaid and Medicare Work Together. Medicaid works to help alleviate costs after Medicare has paid its portion. This means that Medicaid never pays first for your healthcare costs, especially if your Medicare benefits would cover some or all of a particular need or service.
What is Medicare for 65?
Medicare offers health insurance benefits to people who are at least 65-years-old or for people who have disabilities or kidney failure. This kind of insurance is provided by the U.S. federal government and consists of multiple parts that cover different medical needs, such as hospital insurance, medical insurance (for use at doctors’ offices) ...
What is Medicare Advantage?
In terms of Medicare, your health coverage will be through Original Medicare or a Medicare Advantage plan of your choice. If you are enrolled in Part D prescription drug benefits through Medicare, you will be automatically enrolled in the Extra Help program to help with medication costs.
What is dual eligibility?
You’re also considered a dual eligible beneficiary if you’re enrolled in Medicare Part A or Part B and receiving cost-sharing through a Medicare savings program (MSP). Below is table summarizing the benefits and eligibility criteria for each of the different MSPs in 2021: MSP. Benefits.
What is the difference between Medicare and Medicaid?
Takeaway. Medicare is the federal health insurance program in the United States for people age 65 and older. Medicaid is a joint federal and state program to help people with limited resources or income pay for medical costs.
How many people are on Medicare and Medicaid?
According to Health Affairs, about 9.2 million people, representing about 16 percent of Medicare enrollees and about 15 percent of Medicaid enrollees, are enrolled in both Medicare and Medicaid. Keep reading to learn more about dual eligibility, benefits, and state-by-state differences.
What is fee for service Medicaid?
fee-for-service Medicaid coverage. plans that include all Medicare and Medicaid benefits. Income and resource standards are defined by federal law for full Medicaid and the Medicare Savings Programs. At their discretion, states can effectively raise the federally mandated limits.
Is Medicare a dual beneficiary?
If you’re eligible for both Medicare and Medicaid, you’re considered a dual eligible beneficiary. Dual eligibility is typically determined by your age, any disabilities, and income.
Is Medicare free for older people?
It also covers people with certain disabilities and health conditions. Medicare is not free coverage — you’ll still pay deductibles, premiums, and copays for medical services.
Is dual eligibility covered by insurance?
If you’re a dual eligibility beneficiary, it’s likely that most of your healthcare costs are covered. The information on this website may assist you in making personal decisions about insurance, but it is not intended to provide advice regarding the purchase or use of any insurance or insurance products.
What Is Medicare?
Medicare is a federal health insurance program for older people (65 and over), younger people with disabilities, and individuals who have ESRD (End-Stage Renal Disease).
What Is Medicaid?
Medicaid is a federal government and state health care program for low-income individuals of any age in the U.S. This health insurance offers affordable health care options to people who can't afford to pay for medical items, services, and treatments.
What Is Dual Eligibility?
There are a variety of reasons why people may struggle to cover the costs of Medicare insurance.
Who Can Apply for Dual Eligibility?
To qualify for dual eligibility, you need to meet the enrollment criteria for both the Medicare and Medicaid program.
Part A and B Financial Help
Once you're dual eligible, you’ll be able to use your Medicaid to pay some or all of your Original Medicare premiums and health care costs.
Dual-Eligible Benefit Types
There are six types of dual-eligible beneficiaries. Each one has its own financial requirements to enroll and offers other relief from Medicare health care costs.
Dual Eligible and Medicare Advantage
Certain dual eligibles are still allowed to enroll for Medicare Advantage plans. These are called Special Needs Plans (SNPs) and are designed to cater to dual eligibles and other specific groups.
Medicaid Eligibility Categories
The Medicaid eligibility categories encompass all categories of Medicaid eligibility including:
D-SNPs With or Without Medicare Zero-Dollar Cost Sharing
At the time of plan creation, each D-SNP must identify whether or not if offers Medicare zero-dollar cost sharing. In HPMS, D-SNPs will have the option of one of the following two indicators:
What is Medicaid coverage?
Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. Medicaid is a state-based program that is funded jointly by states and the federal government. Within broad national guidelines established by federal statutes, regulations, and policies, each state has the flexibility to:
Can you be dually enrolled in Medicare and Medicaid?
These individuals may either be enrolled first in Medicare and then qualify for Medicaid, or vice versa.
Can QDWIs get Medicare Part A?
QDWIs have income that does not exceed 200% of the FPL, resources that do not exceed two times the SSI resource standard, and are not otherwise eligible for Medicaid. Medicaid pays the Medicare Part A premiums only.

Effects
- Sometimes, the cost of medical care can keep people from seeking out the services they need, especially in situations where it is difficult enough to keep the lights on or buy groceries.
Purpose
- In these situations, government health insurance programs can help with or even cover the cost of necessary exams, procedures or health screenings to ensure that income does not keep people from being healthy. This is where Medicare and Medicaid come in to provide benefits. Generally, Medicare is reserved for people close to retirement age or with life-altering disabilities to offer in…
Definition
- Dual eligibility is the term used to explain that you qualify for both Medicare and Medicaid benefits.
Causes
- This usually occurs in situations where you already qualify for Medicare but because of low income, cannot afford the remaining costs such as deductibles or your portion of the medical bills. If you are dually eligible for both programs, most of your health care expenses will likely be covered, leaving you with a smaller (or no) bill to foot for the care you need.
Benefits
- Medicare offers health insurance benefits to people who are at least 65-years-old or for people who have disabilities or kidney failure. This kind of insurance is provided by the U.S. federal government and consists of multiple parts that cover different medical needs, such as hospital insurance, medical insurance (for use at doctors offices) and prescription medications. If you ar…
Advantages
- Medicare also offers another option Medicare Advantage Plan that allows people to receive their Medicare benefits through a private insurance company. This avenue allows beneficiaries to customize their health insurance needs.
Overview
- Medicaid is a state program that helps low-income individuals and families with the costs of healthcare. This is different from Medicare because you do not have to have a disability or be over the age of 65 to receive health insurance benefits.
Goals
- Medicaids goal is to help people who truly cannot afford the cost of health services because of their income level regardless of age. People who qualify for Medicaid may get assistance paying for premiums, deductibles, coinsurance, copayments, and prescription drugs. And in some cases, Medicaid covers things that Medicare will not, such as the cost of nursing home stays or person…
Programs
- While Medicare is a federal program with one set of requirements, Medicaid is a state-led program that varies from state to state. This means that each state has its own rules for eligibility. While it is hard to give a general guideline to determine your eligibility, most people qualify for Medicaid benefits if they live at or below their states poverty level. The best way to determine if …
Cost
- While Medicaid eligibility is generally determined by your income, there are some cases where you can surpass the qualifying limit but still receive help. This is called the Medicaid spend down and allows you to use Medicaid benefits if you become medically needy. This means that the cost of your healthcare largely impacts your income, or spends down the amount of income that you ha…
Results
- Unlike Medicare enrollment, which can happen automatically when you reach age 65, there is no automatic sign-up for Medicaid. This means you will have to contact your state government to be enrolled. And, because Medicaid eligibility is determined by your income, any changes such as an increase could impact your benefits in the future.
Treatment
- Medicaid works to help alleviate costs after Medicare has paid its portion. This means that Medicaid never pays first for your healthcare costs, especially if your Medicare benefits would cover some or all of a particular need or service. After Medicare pays for your doctors visits, surgeries or procedures, any other kinds of health insurance will then kick in. This means if you …