Dual Eligibility for Medicare and Medicaid: Requirements & Benefits for Long Term Care
- Differentiating Medicare and Medicaid. Persons commonly confuse the terms Medicare and Medicaid. ...
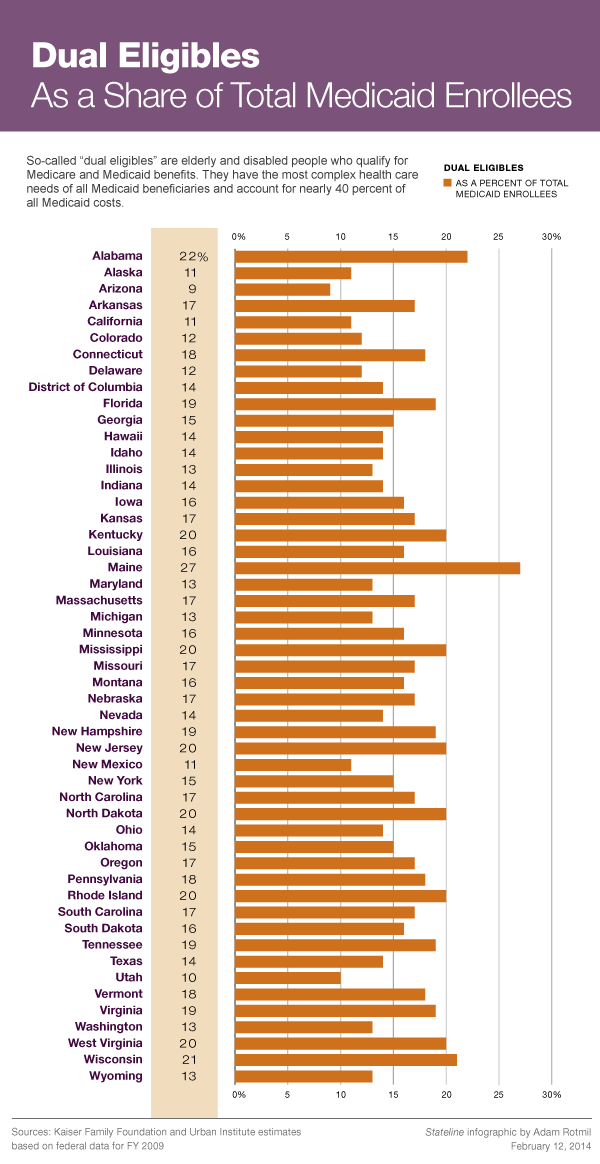
- Definition: Dual Eligible. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees.
- Benefits of Dual Eligibility. ...
- Eligibility Requirements. ...
- Becoming Medicaid Eligible. ...
Full Answer
How to qualify for Medicare and Medicaid as dual eligibility?
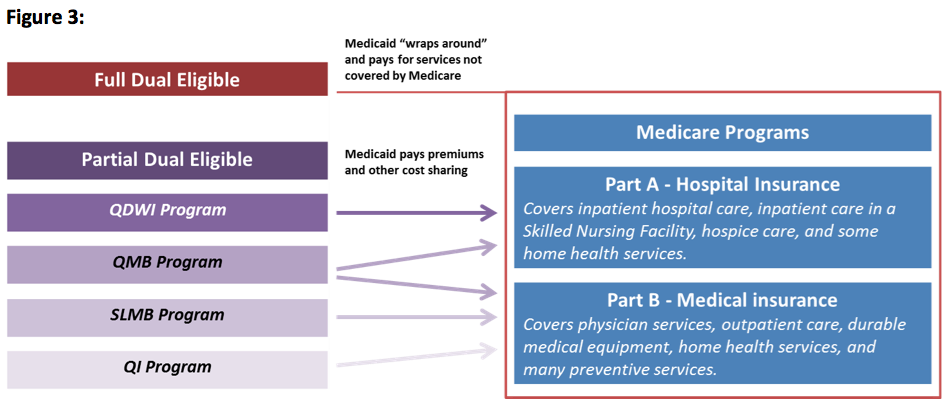
Jul 08, 2020 · The term “full dual eligible” refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as “partial dual eligible.” *Cost sharing is the amount of your health care that you pay out of your own pocket.
What does it mean to be duel eligible?
Dually eligible beneficiaries generally describe low-income beneficiaries enrolled in both Medicare and Medicaid. The term includes beneficiaries enrolled in Medicare Part A, Part B, or both, and getting full Medicaid benefits or only help with Medicare premiums or cost-sharing through 1 of these Medicare Savings Programs (MSP) eligibility groups:
What is full benefit dual eligible?
These people are known as “dual eligible” because they are eligible for both Medicaid and Medicare health care coverage at the same time. Once you are enrolled as a dual eligible, Medicaid funds the cost of maintaining Part A and Part B coverage. Medicare and Medicaid enrollment has been steadily increasing over the past two decades.
What does full dual eligible mean?
Americans who are enrolled in both Medicaid and Medicare are referred to as dual-eligible beneficiaries, or Medicare dual eligibles, or sometimes simply duals. Dual-eligibles are enrolled in both programs when a Medicare enrollee’s income and assets are low enough to qualify them for Medicaid help in paying for some of the costs of Medicare – or to qualify them for full …
What does Medicare Dual Complete mean?
A UnitedHealthcare Dual Complete plan is a DSNP that provides health benefits for people who are “dually-eligible,” meaning they qualify for both Medicare and Medicaid. Who qualifies? Anyone who meets the eligibility criteria for both Medicare and Medicaid is qualified to enroll in a DSNP.Oct 14, 2019
Can I have dual coverage with Medicare?
If you qualify for both Medicare and Medicaid, you are considered "dual eligible." Sometimes the two programs can work together to cover most of your health care costs. Individuals who are dual eligible can often qualify for special kinds of Medicare plans.
Is QMB the same as dual eligible?
Medicaid Only Dual Eligibles (Non QMB, SLMB, QDWI, QI-1, or QI-2) - These individuals are entitled to Medicare Part A and/or Part B and are eligible for full Medicaid benefits. They are not eligible for Medicaid as a QMB, SLMB, QDWI, QI-1, or QI-2.
What does Medicare eligible mean?
You are eligible for Medicare if you are a citizen of the United States or have been a legal resident for at least 5 years and: You are age 65 or older and you or your spouse has worked for at least 10 years (or 40 quarters) in Medicare-covered employment.
Does Medicare cover copay as secondary?
Medicare will normally act as a primary payer and cover most of your costs once you're enrolled in benefits. Your other health insurance plan will then act as a secondary payer and cover any remaining costs, such as coinsurance or copayments.
How do you determine which insurance is primary and which is secondary?
The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer. The secondary payer only pays if there are costs the primary insurer didn't cover.Dec 1, 2021
Does Social Security count as income for QMB?
An individual making $1,800 from Social Security cannot qualify for QMB because they are over the $1,133 income limit.
Who qualifies for QMB?
In order to qualify for QMB benefits you must meet the following income requirements, which can also be found on the Medicare Savings Programs page: Individual monthly income limit $1,060. Married couple monthly income limit $1,430. Individual resource limit $7,730.
Can you bill a Medicaid QMB patient?
Federal law prohibits Medicare providers from billing people enrolled in the Qualified Medicare Beneficiary (QMB) program for any Medicare cost-sharing. This means that if you have QMB, Medicare providers should not bill you for any Medicare-covered services you receive.
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).Feb 11, 2022
Are you automatically enrolled in Medicare if you are on Social Security?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.Jan 3, 2022
What is dual eligible?
What is a dual eligible? Americans who are enrolled in both Medicaid and Medicare are referred to as dual-eligible beneficiaries, or Medicare dual eligibles, or sometimes simply duals. Dual-eligibles are enrolled in both programs when a Medicare enrollee’s income and assets are low enough to qualify them for Medicaid help in paying for some ...
What is a full benefit dual eligible?
full-benefit dual-eligibles – who have Medicare but also receive benefits under Medicaid. partial duals – who have Medicare but qualify to have Medicaid help pay for expenses such as Medicare premiums and/or cost-sharing.
What is Medicaid coverage?
Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. Medicaid is a state-based program that is funded jointly by states and the federal government. Within broad national guidelines established by federal statutes, regulations, and policies, each state has the flexibility to:
Can you be dually enrolled in Medicare and Medicaid?
These individuals may either be enrolled first in Medicare and then qualify for Medicaid, or vice versa.
What is Medicare dual eligible?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program for seniors and disabled persons, Medicaid is a state and federal medical assistance program for financially needy persons of all ages. Both programs offer a variety of benefits, including physician visits and hospitalization, but only Medicaid provides long-term nursing home care. Particularly relevant for the purposes of this article, Medicaid also pays for long-term care and supports in home and community based settings, which may include one’s home, an adult foster care home, or an assisted living residence. That said, in 2019, Medicare Advantage plans (Medicare Part C) began offering some long-term home and community based benefits.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
How old do you have to be to apply for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
Does Medicare provide long term care?
Long-Term Care Benefits. Medicaid provides a wide variety of long-term care benefits and supports to allow persons to age at home or in their community. Medicare does not provide these benefits, but some Medicare Advantage began offering various long term home and community based services in 2019. Benefits for long term care may include ...
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Is there an age limit for Medicare?
Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
