
What is Fiss and how does it work?
What is FISS? The Fiscal Intermediary Standard System (FISS) is the standard Medicare Part A claims processing system. It allows you to perform the following functions:
What is the Fiscal Intermediary standard system (Fiss)?
The Fiscal Intermediary Standard System (FISS) is the standard Medicare Part A claims processing system. Through its Direct Data Entry (DDE) system you may perform the following functions:
What is the status of a claim in Fiss?
Claim is approved for payment and is on the payment floor. This is also considered to be a finalized status. Claim is denied by medical review or claim was submitted as a demand denial. Billing transaction is temporarily paused in FISS for processing and/or Medicare staff intervention may be required.
Which Fiss options are available for claims processing?
All of the FISS functionality that you will need for claims processing is available through FISS options 01, 02, and 03.
What is the Fiss system for Medicare?
The Fiscal Intermediary Standard System (FISS) is the standard Medicare Part A claims processing system. Through its Direct Data Entry (DDE) system you may perform the following functions: Enter, correct, adjust, or cancel your Medicare billing transactions. Inquire about beneficiary eligibility.
How do I get access to Fiss?
If not already enrolled, complete an EDI enrollment form prior to completing the FISS application. Once the EDI enrollment form is processed, you will receive a letter confirming your enrollment. At that time, you can complete the FISS application for access.
How do I correct a Fiss claim?
You can verify whether a claim posted to CWF by reviewing the TPE-TO-TPE (tape-to-tape) field, wMIDh is found on FISS screen Map 171D. 1. To adjust paid or rejected claims, enter the Claims Adjustments option (21,23, or 25) that matches your provider type and press Enter.
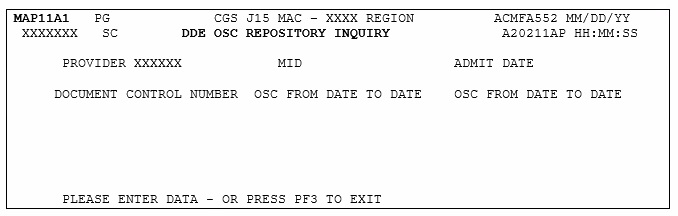
What is the DDE system?
DDE is a real-time Fiscal Intermediary Shared System (FISS) application giving providers interactive access for inquiries, claims entry and correction purposes. Functions include: Eligibility. Claims: Submission, Status, Corrections, Cancellations, Related Attachments and Roster Billing.
What does Fiss stand for?
The Fiscal Intermediary Standard System (FISS) is the standard Medicare Part A. claims processing system.
How do I access DDE?
To access DDE, a request must be submitted electronically by the Authorized Signer using the DDE Electronic Access Request Form. Each facility will have an Authorized Signer. The DDE Authorized Signer is determined by the facility.
How do I cancel my Fiss claim?
MSP Claims can be cancelled electronically or through DDE / FISS. You may only cancel a finalized claim, status location P B9997, that as appeared on your remittance advice. The cancel claim must be made on original paid claim.
What is the difference between a redetermination and an reopening?
2:545:03Reopening vs. Redetermination - YouTubeYouTubeStart of suggested clipEnd of suggested clipAnd assert smirk and/or rack denials no please keep in mind that a redetermination is the firstMoreAnd assert smirk and/or rack denials no please keep in mind that a redetermination is the first level of appeals providers must adhere to the following stipulations.
How long do I have to submit a corrected claim to Medicare?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
What is DDE claim?
The Fiscal Intermediary Shared System (FISS) is the processing system designated by the Centers for Medicare & Medicaid (CMS) to be used for Medicare Part A claims and Part B facility claims. DDE is a real-time FISS application giving providers interactive access for inquiries, claims entry and correction purposes.
How do you suppress a claim in DDE?
Type a 'Y' in the SV (short cut) field located in the upper right hand corner of page 1 and then press [F9].
What is direct data entry?
Direct Data Entry (DDE) is a method of claim submission with full editing, claim correction, and claim status inquiry directly into/from the Fiscal Intermediary Shared System (FISS).
How to exit a session in ELGA?
When you are finished in FISS, press F4 to terminate your session. When you are finished in ELGA or ELGH press F3 to exit.
How to check ELGH eligibility?
To check beneficiary eligibility information via CWF records, instead of typing FSS0, type ELGA to access ELGA, or type ELGH to access ELGH. Press ENTER.
What time does FISS work?
FISS is available Monday through Friday typically between the hours of 5:00 a.m. and 8:00 p.m. CT (Central Time) and Saturday between the hours of 5:00 a.m. and 5:00 p.m. CT. Note: Depending on the time it takes the nightly system cycle to run, FISS may not always be available at 5:00 a.m. CT. In addition, FISS system releases may affect availability over weekends. FISS is not available on Sunday or on national holidays.
How to access FISS?
If you want direct electronic access to FISS in order to perform the above functions, contact the CGS EDI (Electronic Data Interchange) department between 7:00 a.m. – 4:00 p.m. CT (8:00 a.m. 5:00 p.m. ET). For Home Health and Hospice providers, dial 1.877.299.4500 (select Option 2), or for Part A providers, dial 1.866.590.6703 (select Option 2) for assistance. You must also contract with a connectivity vendor to establish direct connection to the Enterprise Data Center (EDC) for FISS access through a connectivity product (e.g., IVANS or VisionShare). The CGS EDI department does not provide support for your connectivity product; therefore, you will need to contact your connectivity vendor for any issues related to your direct connection.
What is inquiry menu?
The Inquiry Menu allows you to check the status of claims, including how to check for Additional Development Requests (ADRs), claims summary, Medicare check history, payment totals, view inquiry screens to check the validity of diagnosis codes, revenue codes, HCPCS codes, and review reason code narratives.
Why does the line continue through the internal local medical necessity edits?
1– the line continues through the internal local medical necessity edits because: the HCPCS code was not applicable to the NCD edit table process, the date of services was not within the range of the effective dates for the codes, the override indicator is set to Y or D, or the HCPCS code field is blank.
What are the options for FISS?
All the FISS functionality that you will need for claims processing is available through FISS options 01, 02, and 03.
What is a FISS connection?
FISS requires a secure telecommunication connection from your facility. This connection is received by contracting with one of the secure DDE Vendors. Contact a vendor prior to completing the FISS application.
How often can you reset your password on DDE?
Please note that you can only use the automated password reset option once in a 24 hour period.
Does CMS require recertification?
The Centers for Medicare & Medicaid Services (CMS) requires annual recertification of every user that has access to the FISS system. Click here for more information.
Do I need to enroll in FISS?
All customers who are requesting a FISS RacfID must be enrolled for electronic billing. If not already enrolled, complete an EDI enrollment form prior to completing the FISS application. Once the EDI enrollment form is processed, you will receive a letter confirming your enrollment. At that time, you can complete the FISS application for access.
Can Novitas Solutions add email address?
That the user agrees that Novitas Solutions can add my email address indicated above to the general email list to receive electronic notifications.
Does Novitasphere have a claim status?
Novitasphere offers Part A users a fast and easy way to access a number of time-saving features including eligibility information and the ability to look up the new MBI numbers for their patients via the MBI Lookup Tool! Now, Part A portal users also have the ability to check Claim Status in the portal! The feature provides details such as billed and paid amounts, check number, status and finalized date, as well as patient claim information and line item details. Also, users have the capability to save or print claim status information via a “PDF” icon.
The Medicare FFS Approach
The purpose of this message is to clearly communicate the approach that Medicare Fee-For-Service (FFS) is taking to ensure compliance with the Health Insurance Portability and Accountability Act's (HIPAA's) new versions of the Accredited Standards Committee (ASC) X12 and the National Council for Prescription Drug Programs (NCPDP) Electronic Data Interchange (EDI) transactions..
CMS HETSHelp site
The CMS HETSHelp site provides information specific to the HIPAA Eligibility Transaction System (HETS) for 270/271 Medicare eligibility transactions. Please visit the HETSHelp site at: http://www.cms.hhs.gov/HETSHelp/ for details about the changes being made to HETS to support the X12 5010 standard.
What is the status loc code for Medicare?
The Status/Location (S/LOC) code for Medicare DDE screens indicates whether a particular claim is paid, suspended, rejected, returned for correction, etc. The six-character alphanumeric code is made up of a combination of four sub-codes: the claim status, processing type, location, and additional location information. Each S/LOC code is made up of two alpha characters followed by four numeric characters. For example, P B9997 is a status location code. • The first position (position a) is the claim’s current status. In this example, “P” indicates the claim has been
What is a DRG PPS?
The Diagnostic related grouper/prospective payment system ( DRG/PPS) inquiry screen displays detailed payment information calculated by the Pricer and Grouper software programs. Its purpose is to provide specific DRG assignment and PPS payment calculations. It should be used to research PPS information as it pertains to an inpatient stay. To start the inquiry process, enter the following information:
How many episodes of care for PBRO?
Displays information from CWF for Radiation Oncology Model (PBRO) Auxiliary File for up to 10 episodes of care for a beneficiary.
How to access provider practice address query screen?
Access the Provider Practice Address Query screen by selecting 1D from the Inquiry Menu Screen.
What is DDE in Medicare?
The Direct Data Entry ( DDE) system was designed as an integral part of the Fiscal Intermediary Standard System (FISS) to be used by all Medicare A providers. DDE will offer various tools to help providers obtain answers to many questions without contacting Medicare Part A via telephone or written inquiry. It will also provide another avenue for electronically submitting claims to the fiscal intermediary, which are listed below.
What is the 60 percent reimbursement rate?
60% Reimbursement Rate - This field identifies the rate the system uses for calculating reimbursement for the HCPC codes. The system displays 60 percent of the total charge in a dollar figure. This is an eight digit field in 999999.99 format.
What is fee indicator?
Fee Indicator - This field identifies the fee indicator that is received from CMS in the physician fee schedule abstract test file. This is a one position field, with six occurrences. The valid values are:
Is the National Drug Code used by FISS?
National Drug Code - This field is not used by FISS.
