What does FWA stand for in Medicare?
· Medicare fraud, waste, and abuse come from a series of laws designed to protect all parties involved in Medicare and Medicaid. The laws promote healthy relationships between agents, carriers, and clients and prevent the insurance industry from becoming profit-based, instead of care-based. Your coverage should be more important than profits.
Which is considered Medicare fraud?
· FWA is an acronym for “Fraud, Waste and Abuse,” a crime you — either as a patient or a provider — may knowingly or unwittingly commit. If the state or federal government charges you with either crime, you may wonder what, exactly the charges entail. The Centers for Medicare and Medicaid Services defines fraud, waste and abuse so that health care professionals can …
How to report Medicare fraud, abuse, and waste?
FWA training is required for all Part C and D first tier, downstream, related and delegated entities, including Medicare Advantage providers who administer the Part D drug benefit or provide health care services to Medicare Advantage
Who is required to undergo compliance and FWA training?
· FWAs. Through the FWA and the Terms of the FWA, an institution commits to HHS that it will comply with the requirements in the HHS Protection of Human Subjects regulations at 45 CFR part 46. The Federalwide Assurance (FWA) is the only type of assurance currently accepted and approved by OHRP. Please note: The fact that the Office for Human Research …
What is FWA in compliance?
• An effective compliance program is essential to prevent, detect, and. correct non‐compliance, as well as, Fraud, Waste and Abuse (FWA). It must, at a minimum, include the Seven Core Elements of an Effective Compliance Program.
How do you stop FWA?
Simple tips that may help you prevent fraud, waste and abuse includes:Review your Explanation of Benefits to ensure accurate dates of services, name of providers, and types of services reported.Protect your insurance card and personal information at all times.Count your pills each time that you pick up a prescription.More items...
Does CMS require FWA training?
Sponsors must provide general compliance and fraud, waste and abuse (FWA) training for all employees of their organization and entities they partner/contract with to provide benefits or services.
How do you report potential FWA?
There are several ways to contact the Hotline:Toll-free phone: 1-800-HHS-TIPS (1-800-447-8477), 8:00 am - 5:30 pm, Eastern Time, Monday-Friday.Fax: 1-800-223-8164 (10 pages or less, please)TTY: 1-800-377-4950.Mail: HHS TIPS Hotline. P.O. Box 23489. Washington, DC 20026. (Note: please do not send any original documents)
Which of the following requires intent to obtain payment and the knowledge that the actions are wrong?
Fraud requires the person to have an intent to obtain payment and the knowledge that their actions are wrong. Waste and abuse may involve obtaining an improper payment, but does not require the same intent and knowledge.
What is the difference between waste and abuse?
6.21 Waste is the act of using or expending resources carelessly, extravagantly, or to no purpose. Importantly, waste can include activities that do not include abuse and does not necessarily involve a violation of law. Rather, waste relates primarily to mismanagement, inappropriate actions, and inadequate oversight.
What happens after non-compliance is detected?
What Happens After Non-Compliance Is Detected? After non-compliance is detected, it must be investigated immediately and corrected promptly.
What must all Medicare Advantage sponsors have in place in order to meet CMS compliance guidelines?
Medicare Advantage Plans Must Follow CMS Guidelines In the United States, according to federal law, Part C providers must provide their beneficiaries with all services and supplies that Original Medicare Parts A and B cover. They must also provide any additional benefits proclaimed in their Part C policy.
What is the minimum core requirements for a compliance program?
The compliance program must, at a minimum, include the following core requirements: 1. Written Policies, Procedures and Standards of Conduct; 2. Compliance Officer, Compliance Committee and High Level Oversight; 3. Effective Training and Education; 4.
What are examples of FWA?
Examples of Fraud, Waste and AbuseBilling for services not rendered.Altering medical records.Use of unlicensed staff.Drug diversion (e.g. dispensing controlled substances with no legitimate medical purpose)Kickbacks and bribery.Providing unnecessary services to members.
What includes any misuse of resources?
Waste includes any misuse of resources such as the overuse of services, or other practices that, directly or indirectly, result in unnecessary costs to the Medicare Program.
What involves payment for items or services?
AbuseAbuse involves payment for items or services when there is no legal entitlement to that payment and the provider has not knowingly and/or intentionally misrepresented facts to obtain payment.
What is Medicare waste?
Waste entails overusing Medicare services and, therefore, causing the Medicare Program to accrue unnecessary costs. Though not necessarily caused by criminal negligence, the government does frown upon it and may intervene if it feels you misuse resources.
How much is Medicare fraud?
Because of this, the government considers it a very serious crime, and one that comes with a penalty of up to $250,000 in fines and 10 years in prison.
Who needs FWA training?
FWA training is required for all Part C and D first tier, downstream, related and delegated entities, including Medicare Advantage providers who administer the Part D drug benefit or provide health care services to Medicare Advantage enrollees.
What is Medicare fraud and abuse training?
The Centers for Medicare and Medicaid Services (CMS) requires annual fraud, waste, and abuse training for organizations providing health, prescription drug, or administrative services to Medicare Advantage (MA) or Prescription Drug Plan (PDP) enrollees on behalf of a health plan.
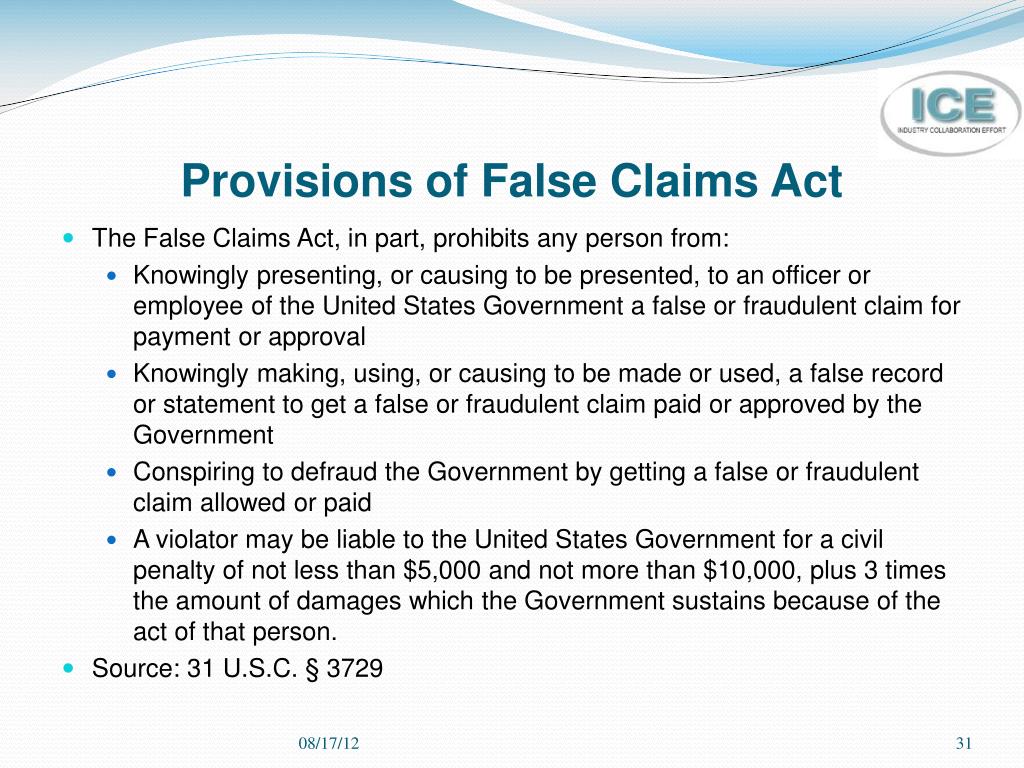
When was the False Claims Act enacted?
The False Claims Act, or FCAwas enacted in 1863 to fight procurement fraud in the Civil War. The FCA has historically prohibited knowingly presenting or causing to be presentedto the federal government a false or fraudulent claim for payment or approval.
What is the GSA exclusion list for Medicare Advantage?
Medicare Advantage Organizations, Part D Sponsors and contracted entities are required to check the OIG and General Services Administration (GSA) exclusion lists for all new employees and at least once a year thereafter to validate that employees and other entities that assist in the administration or delivery of services to Medicare beneficiaries are not included on such lists.
What is Medicare abuse?
Abuse includes any practice that does not provide patients with medically necessary services or meet professionally recognized standards of care.
Why do doctors work for Medicare?
Most physicians try to work ethically, provide high-quality patient medical care, and submit proper claims. Trust is core to the physician-patient relationship. Medicare also places enormous trust in physicians. Medicare and other Federal health care programs rely on physicians’ medical judgment to treat patients with appropriate, medically necessary services, and to submit accurate claims for Medicare-covered health care items and services.
What is CMPL 1320A-7A?
The CMPL, 42 U.S.C. Section 1320a-7a, authorizes OIG to seek CMPs and sometimes exclusion for a variety of health care fraud violations. Different amounts of penalties and assessments apply based on the type of violation. CMPs also may include an assessment of up to three times the amount claimed for each item or service, or up to three times the amount of remuneration offered, paid, solicited, or received. Violations that may justify CMPs include:
What is heat in Medicare?
The DOJ, OIG, and HHS established HEAT to build and strengthen existing programs combatting Medicare fraud while investing new resources and technology to prevent and detect fraud and abuse . HEAT expanded the DOJ-HHS Medicare Fraud Strike Force, which targets emerging or migrating fraud schemes, including fraud by criminals masquerading as health care providers or suppliers.
Is there a measure of fraud in health care?
Although no precise measure of health care fraud exists, those who exploit Federal health care programs can cost taxpayers billions of dollars while putting beneficiaries’ health and welfare at risk. The impact of these losses and risks magnifies as Medicare continues to serve a growing number of beneficiaries.
What is the FWA?
federally-conducted or –supported research covered by the FWA, the U.S. federal department or agency that conducts or supports the research retains final authority for determining whether the Institution complies with the Terms of Assurance. If HHS receives an allegation or indication of noncompliance related to research to which ...
How often does a FWA need to be renewed?
The Institution must renew its FWA every 5 years, even if no changes have occurred, in order to maintain an active FWA.
How often do you need to renew your FWA?
The Institution must renew its FWA every 5 years, even if no changes have occurred, in order to maintain an active FWA. The Institution must update its FWA within 90 days after changes occur regarding the legal name of the Institution, the Human Protections Administrator, or the Signatory Official.
When the Institution becomes engaged in research to which the FWA applies, the Institution and institutional review boards (IRBs
When the Institution becomes engaged in research to which the FWA applies, the Institution and institutional review boards (IRBs) upon which it relies for review of such research will comply with the Common Rule.
How long does it take to complete the FWA lesson?
It should take about 10 minutes to complete. Upon completing the lesson, you should correctly:
What is Medicare Advantage?
Medicare Part C, or Medicare Advantage (MA), is a health insurance option available to Medicare beneficiaries. Private, Medicare-approved insurance companies run MA programs. These companies arrange for, or directly provide, health care services to the beneficiaries who enroll in an MA plan.
What is Medicare Part C and D?
As a person providing health or administrative services to a Medicare Part C or D enrollee, you play a vital role in preventing fraud, waste, and abuse (FWA). Conduct yourself ethically, stay informed of your organization’s policies and procedures, and keep an eye out for key indicators of potential FWA.
What is the difference between fraud, waste, and abuse?
One of the primary differences is intent and knowledge. Fraud requires intent to obtain payment and the knowledge the actions are wrong. Waste and abuse may involve obtaining an improper payment or creating an unnecessary cost to the Medicare Program but do not require the same intent and knowledge.
What is Medicare Learning Network?
The Medicare Learning Network® (MLN) offers free educational materials for health care professionals on the Centers for Medicare & Medicaid Services (CMS) programs, policies, and initiatives. Get quick access to the information you need.
What is fraud in health care?
Fraud is knowingly and willfully executing, or attempting to execute, a scheme or artifice to defraud any health care benefit program or to obtain, by means of false or fraudulent pretenses, representations, or promises, any of the money or property owned by, or under the custody or control of, any health care benefit program.