Medicare ABN Specific Modifiers – GA, GX, GY, GZ
- GA Modifier: Waiver of Liability Statement Issued as Required by Payer Policy. ...
- GX Modifier: Notice of Liability Issued, Voluntary Under Payer Policy. ...
- GY Modifier: Notice of Liability Not Issued, Not Required Under Payer Policy. ...
- GZ Modifier: Item or Service Expected to Be Denied as Not Reasonable and Necessary. ...
What is G0 modifier used for?
Apr 03, 2020 · GY Modifier: How Is It Different? The GY modifier is similar to the GZ modifier in that it is used to specify that the supply or service is not supported by any definition of Medicare accepted policies. The difference between the GY and the GZ modifier is the issuing of an ABN. The GY modifier helps with auto-denial claims and is typically used when a patient has …
What is a GA modifier for Medicare?
May 06, 2018 · Modifier GY Item or service statutorily excluded or does not meet the definition of any Medicare benefit Statutorily Excluded Examples (not all-inclusive) Hearing aids Most dental items Personal comfort items Does Not Meet Definition of Medicare Benefit Examples (not all-inclusive) Prosthetic device for temporary conditions
When to use G codes for Medicare?
Jul 07, 2010 · The GY modifier is used to obtain a denial on a Medicare non-covered service. This modifier is used to notify Medicare that you know this service is excluded. The explanation of benefits the patient get will be clear that the service was …
What is gz modifier?
May 11, 2011 · Modifier GY Fact Sheet. Definition: • If the service provided is statutorily excluded from the Medicare Program, the claim will deny whether or not the modifier is present on the claim. Example: Patient transport is for a non-covered condition that does not meet the definition of any Medicare benefit. The provider is expecting a denial.

What does GY modifier mean for Medicare?
is statutorily excludedAdding the GY HCPCS modifier to the CPT code indicates that an “item or service is statutorily excluded or the service does not meet the definition of Medicare Benefit.” This will automatically create a denial and the beneficiary may be liable for all charges whether personally or through other insurance.Jun 6, 2021
Does Medicare cover GY modifier?
The GY modifier must be used when physicians, practitioners, or suppliers want to indicate that the item or service is statutorily non-covered or is not a Medicare benefit.Feb 4, 2011
When should a GY modifier be used?
Beginning in January 2002, Medicare allowed providers and suppliers to use the GY modifier to indicate that a service or item is not covered by Medicare, either because it is statutorily excluded (e.g., hearing aids) or does not meet the definition of any Medicare benefit (e.g., surgical dressings that are used to ...
Can we bill patient for GY modifier?
Modifier GY will cause the claim to deny with the patient liable for the charges....Region Service was Performed in:Part B Medical ClaimsPart A Facility ClaimsMIB MI (J8)INA IN (J8)MIA MI (J8)2 more rows•Feb 3, 2016
Is ABN needed for GY modifier?
Does a beneficiary need to sign an Advance Beneficiary of Noncoverage (ABN) for every visit? Answer: Notifiers are required to issue ABNs when an item or service is expected to be denied based on one of the provisions in the Medicare Claims Processing Manual Chapter 30 §50.5.
What is Medicare Code A9270 Gy?
GY - Item or service statutorily excluded or does not meet the definition of any Medicare benefit. GZ - Item or service expected to be denied as not reasonable and necessary. Clarification on Use of A9270. HCPCS code A9270, Non-covered item or service, will remain an active code and valid for Medicare.
What is statutorily excluded service?
The -GX modifier indicates you provided the notice to the beneficiary that the service was voluntary and likely not a covered service. -GY – Item or service statutorily excluded, does not meet the definition of any Medicare benefit or for non-Medicare insurers, and is not a contract benefit.
Which of the following is excluded under Medicare?
Non-medical services, including a private hospital room, hospital television and telephone, canceled or missed appointments, and copies of x-rays. Most non-emergency transportation, including ambulette services. Certain preventive services, including routine foot care.
What is the difference between GA and GX modifier?
Modifier Modifier Definition Modifier GA Waiver of Liability Statement Issued as Required by Payer Policy. Modifier GX Notice of Liability Issued, Voluntary Under Payer Policy. Modifier GY Notice of Liability Not Issued, Not Required Under Payer Policy.Jul 14, 2021
What is a modifier GY?
Under the Medicare program, modifier GY, Item or service statutorily excluded, does not meet the definition of any Medicare benefit or for non-Medicare insurers, is not a contract benefit is appended to procedures that are excluded from the Medicare payment system.
What is the purpose of a modifier GY?
Modifier GY identifies services and supplies that are statutorily excluded from Medicare coverage.
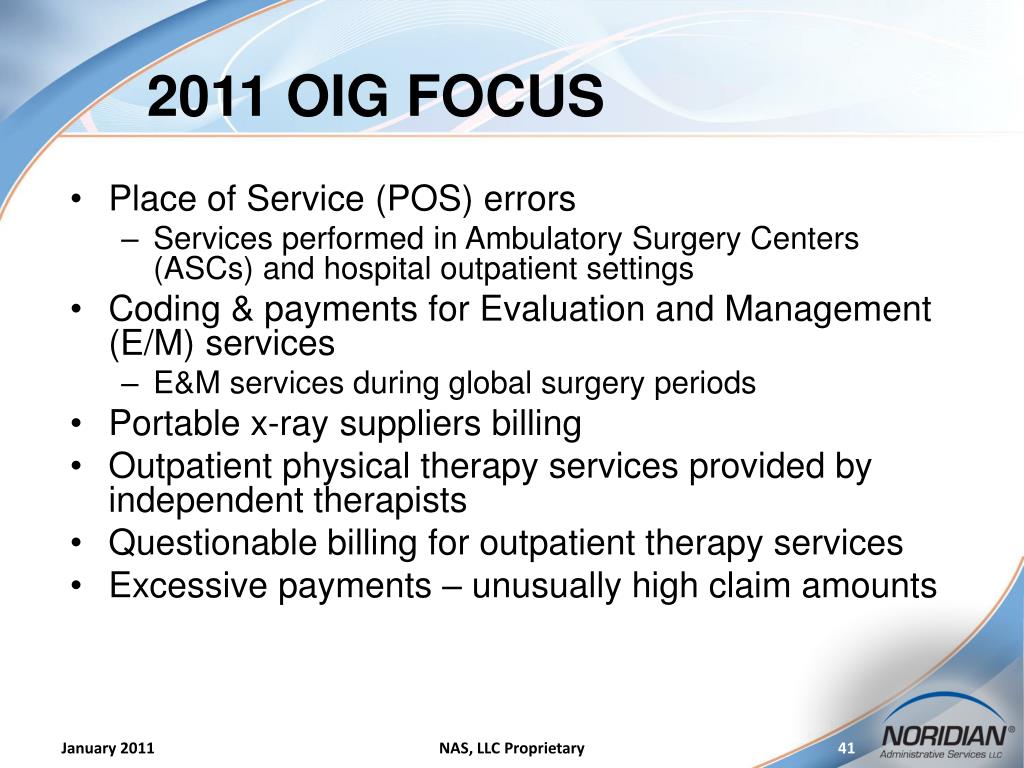
What is the purpose of the OIG investigation?
The object of the investigation is to determine the appropriate use of the modifier and to determine if Medicare patients are unknowingly becoming liable for health care expenses.
What is the GA modifier?
This GA modifier is to notify Medicare from provider that ABN is on file, and provider anticipates Medicare probably or certainly will not to cover those item or service. So by this provider indicates that patient has signed ABN form by appending GA modifier to CPT and patient will be responsible for the charges billed, if those items or service not covered by Medicare.
Why do you need to add GA modifier to CPT?
GA modifier should be append to a CPT, for which the provider had a patient sign an ABN form because there is a possibility the service may be denied because the patient’s diagnosis might not medically necessary. By this provider ensure upon Medicare denial, member will be liable to pay those services.
What is an ABN for Medicare?
ABN is also known as Waiver of Liability, signed by Medicare patients. In other way we can say a notice the hospital or doctor gives the patient before the treatment, telling the patient that Medicare may not pay for some treatment or services. This ABN document is signed by the patient, stating that, in case of Medicare is not going to pay, or not covering the payment, the patient himself is liable for the payment.
Can you use ABN modifiers on Medicare Advantage?
ABN modifiers are prohibited for Medicare advantage enrollees. As per CMS, dated on May 05, 2014 released that Advance Beneficiary notice modifiers i.e. GA, GX, GY or GZ to be used only for Medicare beneficiaries and not to be used for members of Medicare advantage plans.
Does Medicare cover CPT 15775?
CPT 15775 and 15776 performed for cosmetic reason will be denied as non-covered. Medicare does not cover cosmetic surgery codes that are performed to reshape or improve the beneficiary appearance.
What is a GY modifier?
The definition is for GY is it is to be used for items or services that are statutorily excluded items or that do not meet the definition of any Medicare benefit.
What is the 1862 (a) (1) exclusion?
All decisions that items, services, etc. are not covered are based on §1862 (a) (1) of the Act (the “not reasonable and necessary” exclusion) unless otherwise specifically noted. Where another statutory authority for denial is indicated, that is the sole authority for denial.
Can a lab test be modified with a GY modifier?
The Medicare NCD Manual for Laboratory Tests lists the diagnosis that are considered screening and as such can be modified with the GY modifier in order to transfer the liability to the patient. Here is a link to the Manual.