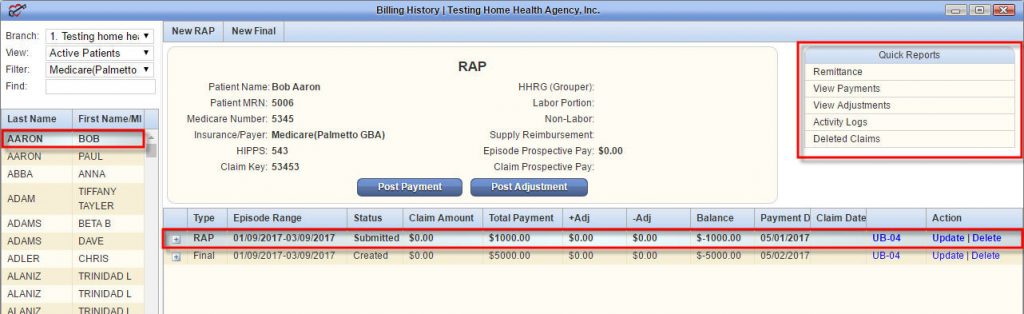
When should I submit my raps to the HHA?
Requirements and resources for home health outpatient therapy billing are available on the Home Health Outpatient Therapy Billing page. In addition, HHAs are required to issue an Advance Beneficiary Notice (ABN) to beneficiaries before providing them therapy that is not medically reasonable and necessary, regardless of the therapy cap.
When are HHAs paid for home health visits?
A hospice revocation occurs when a beneficiary chooses to end their hospice care. The beneficiary must sign a revocation form indicating the date they wish the revocation to become effective. When reporting a revocation, the hospice must bill an occurrence code (OC) 42 along with the date the revocation is effective.
Are you eligible for Medicare home health services?
Consolidated billing. For individuals under a home health plan of care, payment for all services (nursing, therapy, home health aides and medical social services) and routine and non-routine medical supplies, with the exception of certain injectable osteoporosis drugs, DME, and furnishing negative pressure wound therapy (NPWT) using a disposable device is included in the HH PPS …
What is the CBSA code for home health insurance?
Jan 12, 2022 · Home Health and Hospice Areas (HH+H) There are four A/B MACs that process home health and hospice claims in addition to their typical Medicare Part A and Part B claims. Please note that the four HH+H areas do not coincide with the jurisdictional areas covered by these four A/B MACs.
What is Medicare HHH?
Are H codes billable to Medicare?
What are the codes for medical billing?
- International Classification of Diseases (ICD) codes.
- Current Procedure Terminology (CPT) codes.
- Healthcare Common Procedure Coding system (HCPCS) codes.
What is HH PPS?
What are H CPT codes?
What are the three categories of CPT codes?
What are the different types of medical coding?
- ICD Codes.
- CPT Codes.
- HCPCS Codes.
- DRG Codes.
- Modifiers.
What is the difference between CPT code and procedure code?
What is modifier in medical billing?
What is a Medicare outlier payment?
What is covered under the ambulance fee schedule?
It applies to all ambulance services, including volunteer, municipal, private, independent, and institutional providers, i.e., hospitals, critical access hospitals (except when it is the only ambulance service within 35 miles), and skilled nursing facilities.Jan 6, 2022
What is episodic billing?