What is Humana timely filing? Medicare Advantage: Claims must be submitted within one year from the date of service or as stipulated in the provider agreement. Commercial: Claims must be submitted within 90 days from the date of service if no other state-mandated or contractual definition applies.
How to refund Humana overpayments?
Mar 06, 2020 · What is Humana timely filing? Medicare Advantage: Claims must be submitted within one year from the date of service or as stipulated in the provider agreement. Commercial: Claims must be submitted within 90 days from the date of service if no other state-mandated or contractual definition applies.
Does Humana do subrogation?
Apr 06, 2020 · What is the timely filing limit for Medicare Advantage plans? 12 months Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided.
Where to send Humana claims?
Apr 15, 2021 · What is the timely filing limit for Humana appeals? within 60 calendar days In order to request an appeal of a denied claim, you need to submit your request in writing within 60 calendar days from the date of the denial. How do I correct my Humana claim? Claims Payment Inquiries. Call Humana’s provider call center at 800-457-4708.
How do I file an appeal with Humana?
Commercial: Claims must be submitted within 90 days from the date of service if no other state-mandated or contractual definition applies. If a claim is submitted in error to a carrier or agency other than Humana, the timely filing period begins on the date the provider was notified of the error by the other carrier or agency.
What is Humana Medicare timely filing limit for corrected claims?
Claims must be submitted within 365 days of the date of service or discharge. We will not pay if there is incomplete, incorrect or unclear information on a claim. If this happens, providers have 365 days from the date of service or discharge to submit a corrected claim or file a claim appeal.
Does Humana follow CMS guidelines?
Humana is excited to announce that we recognize the new coding and guidelines for our Medicare Advantage, commercial and select Medicaid plans. When the AMA and CMS differ in their coding and guidelines, Humana plans follow the CMS guidance.
Is Humana a form of Medicare?
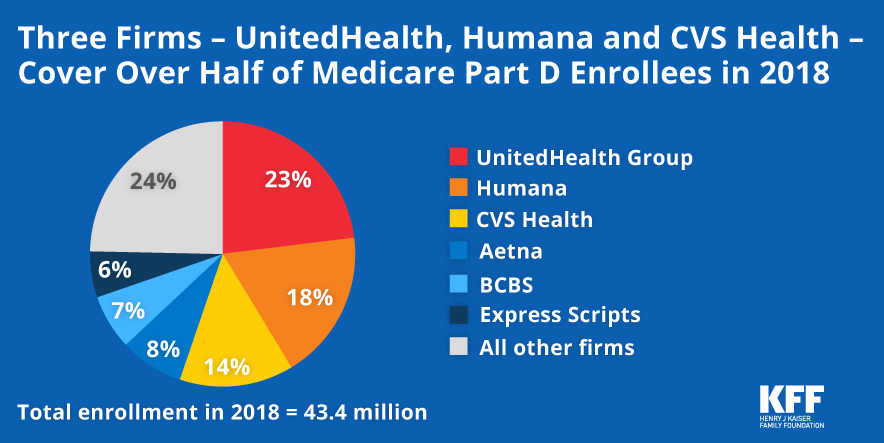
Unlike Original Medicare (Part A and Part B), which is a federal fee-for-service health insurance program, Humana is a private insurance company that contracts with Medicare to offer benefits to plan members.
How do I submit an appeal to Humana?
How can I submit a grievance request?Fax number: 1-855-251-7594.Mailing address: Humana Grievances and Appeals. P.O. Box 14165. ... Puerto Rico members: Use the following form and fax and/or mailing address: Appeal, Complaint or Grievance Form – English. ... Fax number: 1-800-595-0462.Mailing address: Humana Puerto Rico.Nov 6, 2013
Does Humana follow NCCI edits?
Updates are made to Humana's editing systems based on direction from the AMACPT, the National Correct Coding Initiative (NCCI) and other applicable codingstandards.
Does Humana accept modifier 59?
1, 2020. Humana's policy is consistent with the CMS changes. The Humana decision significantly reduces the instances in which a PT will need to append the 59, X, XE, XP, XS, or XU modifiers and will eliminate situations in which certain code pairs were prohibited.Feb 17, 2021
Do I need Humana if I have Medicare?
People eligible for Medicare can get coverage through the federal government or through a private health insurance company like Humana. Like Medicaid, every Medicare plan is required by law to give the same basic benefits. Private health insurance plans, like Humana's, often add extra benefits and services for members.
What is an AOR form Humana?
If you are filing an appeal or grievance on behalf of a member, you need an Appointment of Representative (AOR) form or other appropriate legal documentation on file with Humana so that you are authorized to work with Humana on his or her behalf.Feb 15, 2022
What is Humana out of pocket maximum?
Individual maximum out-of-pocket – $8,150* Preventive exams, screenings and immunizations – 100%
Does Humana accept corrected claims?
If an underpayment is identified during the review and the healthcare provider is owed payment by Humana, the healthcare provider may be asked to submit a corrected claim to receive additional reimbursement.
Who is the head of Humana?
Bruce D. Broussard (Jan 1, 2013–)Humana / CEOBruce Dale Broussard is chief executive officer and president of Humana, a health insurance company with headquarters in Louisville, Kentucky. Wikipedia
What is Humana payer ID?
HUMANA INC. Arcadian Management Services Inc Other ID's: L0200, 72127, 62072, 61120, 62073, 73288, 95885. Full Payer List.
Submitting a claim electronically
Healthcare professionals and facilities can use the Availity Portal and electronic data interchange (EDI) services as no-cost solutions for submitting claims electronically. To register for the Availity Portal or to learn more about Availity claims solutions, visit Availity.com.#N#, opens new window
Advanced claims editing
All EDI submissions to Humana pass through Availity. A process known as advanced claims editing (ACE) applies coding rules to a medical claim submitted through the Availity gateway via EDI before the claim enters Humana’s claim payment system.
Time frames to submit a claim
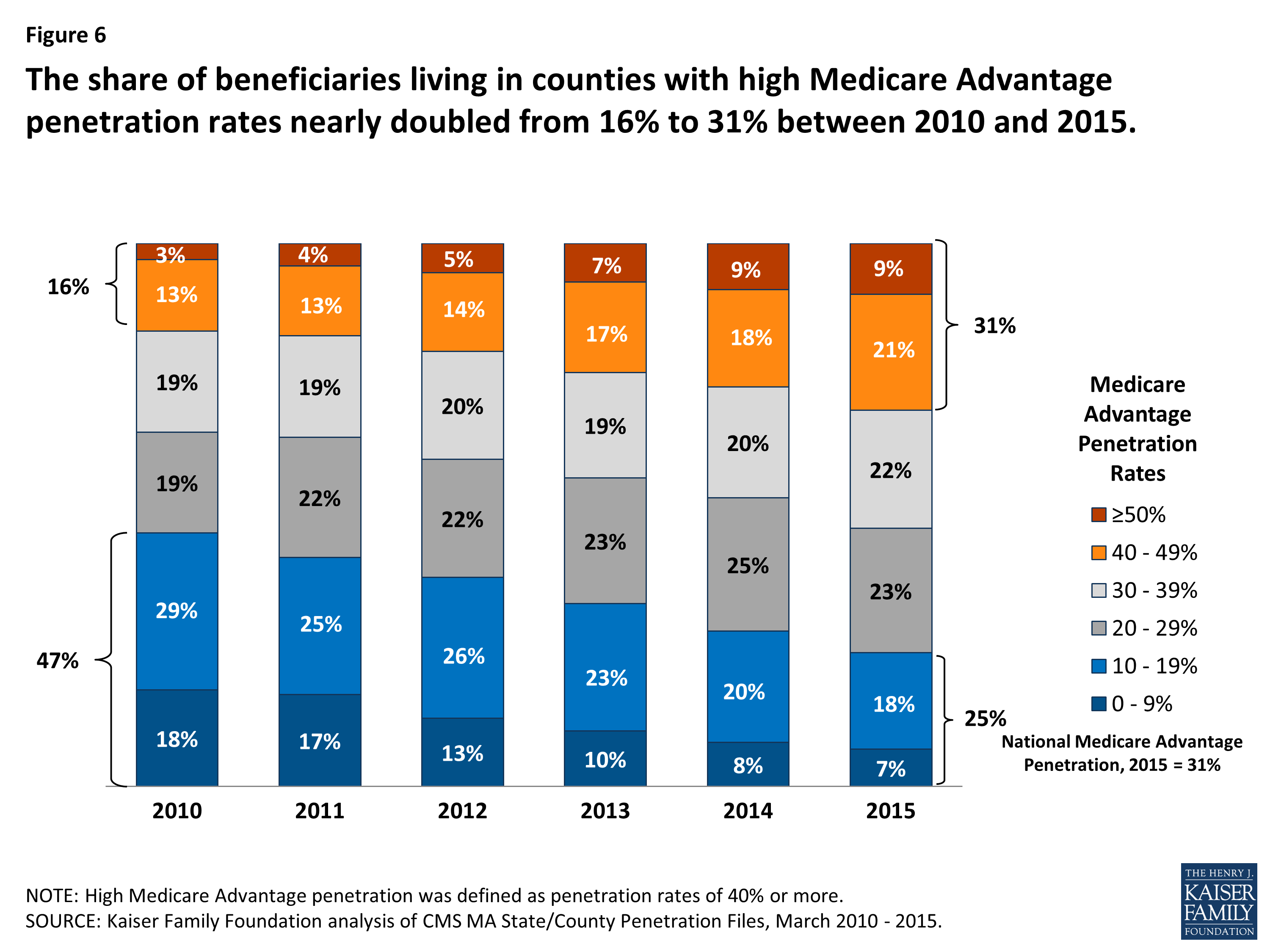
Please note the following time frames for submitting Medicare Advantage or commercial claims:
Checking claim status online
Healthcare professionals can check the status of a claim on the Availity Portal. Registration is required for access to the portal. Go to Availity.com#N#, opens new window
Assistance with claim submission
If your claim is rejected at the vendor level, please contact the vendor for assistance.
Texas deficient claims
If you are a Texas-based healthcare provider, read this flyer to learn how to check a deficient claim online.
What is timely filing limit in medical billing?
Timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. For example, if any patient getting services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement.
How to handle timely filing denial claims?
When received timely filing denials in that case we have to first review the claim and patient account to check when we billed the claim that it was billed within time or after timely filing. In some case claim was billed within time but stuck in our system or rejected by the system.
What is Medicare Administrative Contractor?
The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC Statement of Work. The contractor is not obligated to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer. If the contractor considers anything provided, as described above, to be outside the current scope of work, the contractor shall withhold performance on the part(s) in question and immediately notify the Contracting Officer, in writing or by e-mail, and request formal directions regarding continued performance requirements.
Does the revision date apply to red italicized material?
Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents.
