For patients on Medicare Part D, the cost can range from $660.00 – 2,847.00 per month, based on your coverage phase. Patients with Low-Income Subsidy for Medicare will pay $8.95 per month. Compared to other approved oral HCV treatments, Mavyret is priced very competitively and may be your lowest-cost option.
Full Answer
Is Mavyret covered by Medicare?
Sep 10, 2021 · For patients on Medicare Part D, the cost can range from $660.00 – 2,847.00 per month, based on your coverage phase. Patients with Low-Income Subsidy for Medicare will pay $8.95 per month. Compared to other approved oral HCV treatments, Mavyret tablets are priced very competitively and may be your lowest-cost option.
How much does Medicare Part D prescription drug coverage cost in 2021?
May 16, 2019 · The Centers for Medicare & Medicaid Services (CMS) issued a final rule on May 16, 2019 that modernizes and improves the Medicare Advantage and Part D programs. These changes will ensure that patients have greater transparency into the cost of prescription drugs in Part D and will also enable Medicare Advantage plans to negotiate better prices for physician …
What is Medicare Part D (Medicare drug coverage)?
Dec 01, 2021 · Creditable Coverage Disclosure to CMS. Entities that provide prescription drug coverage to Medicare Part D eligible individuals must disclose to CMS whether the coverage is "creditable prescription drug coverage". This disclosure is required whether the entity's coverage is primary or secondary to Medicare.
How can I lower the cost of my Mavyret prescription?
What Medicare Part D drug plans cover. Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site. Costs for Medicare drug coverage. Learn about the types of costs you’ll pay in a Medicare drug plan. How Part D works with other insurance

What tier drug is MAVYRET?
Medicare prescription drug plans typically list Mavyret on Tier 5 of their formulary. Generally, the higher the tier, the more you have to pay for the medication. Most plans have 5 tiers.
Which medication would not be covered under Medicare Part D?
For example, vaccines, cancer drugs, and other medications you can't give yourself (such as infusion or injectable prescription drugs) aren't covered under Medicare Part D, so a stand-alone Medicare Prescription Drug Plan will not pay for the costs for these medications.
Does Medicaid pay for MAVYRET?
MAVYRET has preferred formulary status on the majority of2: Patients on Medicaid can have out-of-pocket costs of $20 or less depending on state plan. Most patients with commercial insurance will pay as little as $5 per month with their MAVYRET copay card.
What is a CMS excluded Part D drug?
products that contain at least one Part D drug component. are part D drugs when used for a "medically accepted" indication, unless CMS makes a determination that such. product, as a whole, belongs in one of the categories of. drugs excluded from coverage under Part D.Apr 19, 2006
What is the most popular Medicare Part D plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
Do any Part D plans cover chemotherapy drugs?
Part D covers most prescription medications and some chemotherapy treatments and drugs. If you have Original Medicare with a Medicare drug plan, and Part B doesn't cover a cancer drug, your drug plan may cover it.
What is the success rate of Mavyret?
Yes, Mavyret is a treatment that can clinically cure hepatitis C viral infection (HCV). The success rate for curing hepatitis C with Mavyret ranges from 95 to 99%.Jul 22, 2020
Can you take Mavyret at night?
I feel GREAT, I have found out that to keep the nausea away, it is best taken at night with food a few hours before bed.
What is the difference between Mavyret and Epclusa?
They're also both combination medications: Mavyret contains the active drugs glecaprevir and pibrentasvir. Epclusa contains the active drugs velpatasvir and sofosbuvir.Feb 19, 2021
Does Medicare Part D cover biologics?
Nationally, nearly all Part D plans cover at least one biologic DMARD, but the vast majority require sufficiently high cost sharing to risk significant financial burden to patients.
Is Medicare Part D required by law?
Is Medicare Part D Mandatory? It is not mandatory to enroll into a Medicare Part D Prescription Drug Plan.
Is vitamin D covered by Part D?
Most prescription vitamins, including vitamin D2 and D3, and minerals. Medicare Part D does cover prenatal vitamins, fluoride and vitamin D analogs, such as calcitriol, doxercalciferol and paricalcitol.
How much does Medicare cover in the donut hole?
Therefore, you may pay more for your drug. Copay Range. $7 – $15180. In the Post-Donut Hole (also called Catastrophic Coverage) stage, Medicare should cover most of the cost of your drug.
What is prior authorization for Medicare?
Most Medicare prescription drug plans have prior authorization rules that will require your prescriber to contact your plan before you can get your medication. This is to show that the drug is medically necessary.
What is the post deductible stage?
After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug.
What drugs are included in Part D?
Current Part D policy requires sponsors to include on their formularies all drugs in six categories or classes: 1) antidepressants; 2) antipsychotics; 3) anticonvulsants; 4) immunosuppressants for treatment of transplant rejection; 5) antiretrovirals; and 6) antineoplastics; except in limited circumstances. Under current policy, Part D sponsors are ...
When did Medicare and Medicaid change?
The Centers for Medicare & Medicaid Services (CMS) issued a final rule on May 16, 2019 that modernizes and improves the Medicare Advantage and Part D programs. These changes will ensure that patients have greater transparency into the cost of prescription drugs in Part D and will also enable Medicare Advantage plans to negotiate better prices ...
Does step therapy apply to new starts?
Under the policy being finalized, step therapy may only apply to new starts of medication, must be reviewed and approved by the plan’s pharmacy and therapeutics committee, and when patients request coverage of or appeal a denial of a Part B drug, a plan’s decision-making timeframe will be shorter and mirror current Part D rules.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.
What drugs does Medicare cover?
Medicare also requires Part D prescription drug plans to cover almost all drugs in these six classes: antidepressants, anti-convulsants, anti-psychotics, immunosuppressants, cancer drugs, and HIV/AIDS drugs. What is a prescription drug plan formulary?
What to do if Medicare doesn't cover a prescription?
If your Medicare prescription drug plan doesn’t cover a medication you think you need, covers the medication on a higher tier, or requires a coverage rule that you think should be waived, your doctor can submit a “Model Coverage Determination Request” form to your plan.
Does Medicare cover Part D?
Approved by the FDA. Sold and used in the United States. Not covered under Original Medicare, Part A or Part B. Also, Medicare Part D prescription drug plans are required to cover at least two drugs in each therapeutic class of drugs, along with certain vaccines and diabetes supplies. Medicare also requires Part D prescription drug plans ...
What are the tiers of a drug plan?
Here’s an example of how a plan might divide its drug tiers: Tier 1 — Most generic drugs. Tier 1 drugs will cost you the least amount. Tier 2 — Preferred brand-name drugs. Tier 2 drugs may cost you more than Tier 1 drugs. Tier 3 — Non-preferred brand-name drugs.
What is Tier 4 drug?
Tier 4 drugs are typically unique, very high-cost drugs and are likely to have the highest copayment or coinsurance. What are some of the prescription drug plan coverage rules? Most Medicare prescription drug plans use coverage rules, or limits on coverage, for certain prescription drugs.
What happens if you don't have a prescription drug plan?
If you are a member of a stand-alone prescription drug plan or a Medicare Advantage plan with prescription drug coverage, you have rights and options if your medication is not listed on your plan’s formulary: You can ask your doctor if you can switch to another drug that is on the formulary.
What are the two types of exceptions?
There are two types of exceptions: Formulary exception: You can request a formulary exception if your doctor believes it’s medically necessary for you to take a drug that is not on the formulary, or your doctor believes that a coverage rule should be waived (such as a quantity limit or step therapy requirement).
What is formulary in insurance?
Your prescriptions and whether they’re on your plan’s list of covered drugs (. formulary. A list of prescription drugs covered by a prescription drug plan or another insurance plan offering prescription drug benefits. Also called a drug list.
What is extra help?
Extra Help. A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. paying your drug coverage costs. Look for specific Medicare drug plan costs, and then call the plans you're interested in to get more details. Note.
How much is Medicare Part D 2021?
How much does Medicare Part D cost? As mentioned above, the average premium for Medicare Part D plans in 2021 is $41.64 per month. The table below shows the average premiums and deductibles for Medicare Part D plans in 2021 for each state. Learn more about Medicare Part D plans in your state.
What is Part D premium?
Your Part D deductible is the amount that you must spend out of your own pocket for covered drugs in a calendar year before the plan kicks in and begins providing coverage.
What is the difference between generic and brand name drugs?
Generic drugs are typically on lower tiers and cost less, while brand name drugs and specialty drugs are typically on higher tiers and cost more. Medicare Part D plans are sold by private insurance companies. These insurance companies are generally free to set their own premiums for the plans they sell.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
What is the Medicare donut hole?
After 2020, Medicare Part D plans have a shrunken coverage gap, or “donut hole,” which represents a temporary limit on what the plan will cover for prescription drugs. You enter the Part D donut hole once you and your plan have spent a combined $4,130 on covered drugs in 2021.
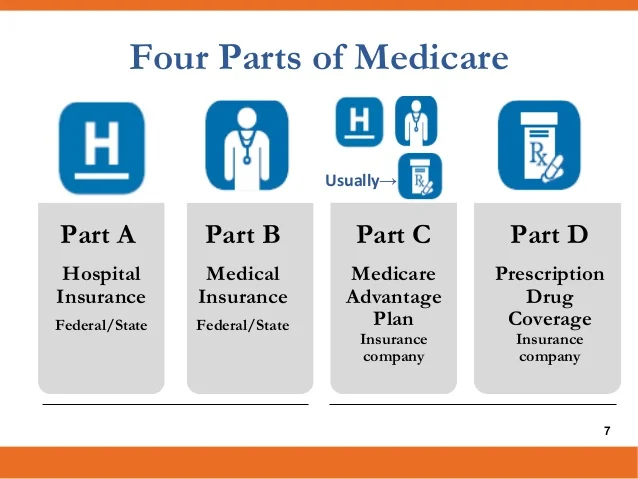
Does Medicare Advantage cover Part A?
Medicare Advantage plans (also called Medicare Part C) provide all of the same coverage as Medicare Part A and Part B, and many plans include some additional benefits that Original Medicare doesn’t cover. Read additional medicare costs guides to learn more about Medicare costs and how they will affect you.
What is coinsurance and copayment?
Copayments and coinsurance are the amounts that you must pay once your plan’s coverage does begin. A copayment is usually a fixed dollar amount (such as $5) while coinsurance is most often a percentage of the cost (such as 20 percent). Plans might have different copayment or coinsurance amounts for each tier of drugs.