Do premiums count towards out of pocket maximum?
Your premium, which you must continue paying to maintain your insurance coverage, doesn’t count toward your out-of-pocket limit. Here is an overview of healthcare expenses which DO count toward your out-of-pocket maximum: Deductibles, Coinsurance fees, Copayments, and
Is there a cap on out of pocket for Medicare?
You can think of an out-of-pocket limit as a “cap.” There is no cap on your share of medical expenses under Original Medicare. For example, you usually pay 20% of your allowable Medicare Part B charges regardless of the total amount. If the allowable charges for your surgeon’s bill total $10,000, your share is typically $2,000.
Does Medicare have a standard "out-of-pocket maximum"?
There isn't a maximum out of pocket on Medicare. Because of this, there is no limit to the amount you can pay in medical bills. You can contribute 20% of any number of costs after meeting the deductible. Don't worry, though; we have a few solutions to help you. Below we discuss Medicare plans that have a maximum limit and some that don't.
Should you buy a Medigap or Medicare Advantage plan?
About 14.5 million beneficiaries are enrolled in a Medigap plan, which helps cover certain cost-sharing aspects of original Medicare ... "I've seen it a lot." If you work with an agent, you should ask how many insurance companies they work with (or ...

Do you pay more out-of-pocket with Medicare Advantage?
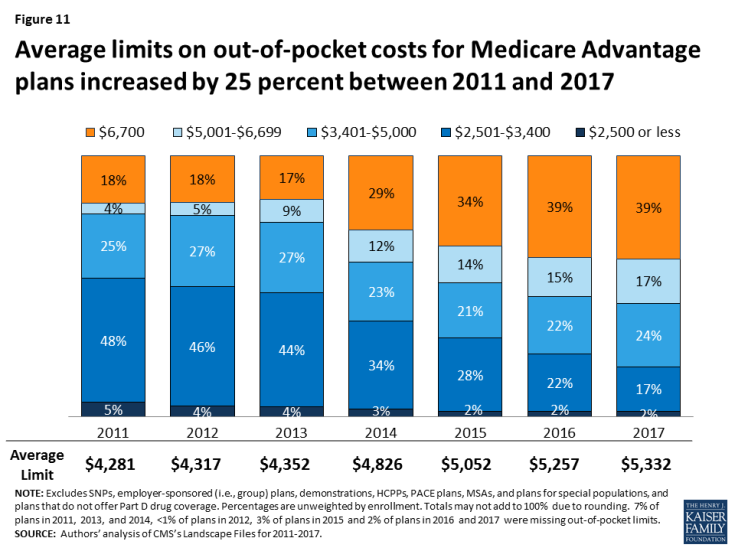
Medicare Advantage plans out-of-pocket maximum Unlike Original Medicare, all Medicare Advantage plans have out-of-pocket maximums. An out-of-pocket maximum can be a reassuring thing because this means you only have to pay up to known amount before all your covered medical costs are paid for.
What is the maximum out-of-pocket for Medicare Advantage plans for 2022?
The maximum out-of-pocket limit for Advantage Plans can reach up to $7,550 in 2022 for in-network services. For out-of-network, that cap would be $11,300.
What does out-of-pocket mean with Medicare Advantage plans?
out-of-pocket costs. Health or prescription drug costs that you must pay on your own because they aren't covered by Medicare or other insurance. in a. Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare.
Do Medicare Advantage plans have limits?
Medicare Advantage Plans have a yearly limit on your out-of-pocket costs for medical services. Once you reach this limit, you'll pay nothing for covered services. Each plan can have a different limit, and the limit can change each year. You should consider this when choosing a plan.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
What are the negatives to a Medicare Advantage plan?
The takeaway There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling. Whether you choose original Medicare or Medicare Advantage, it's important to review healthcare needs and Medicare options before choosing your coverage.
What is the out-of-pocket maximum for Medicare Advantage plans for 2021?
Since 2011, federal regulation has required Medicare Advantage plans to provide an out-of-pocket limit for services covered under Parts A and B. In 2021, the out-of-pocket limit may not exceed $7,550 for in-network services and $11,300 for in-network and out-of-network services combined.
Does Medicare Advantage pay 100 percent?
Medicare Advantage plans must limit how much their members pay out-of-pocket for covered Medicare expenses. Medicare set the maximum but some plans voluntarily establish lower limits. After reaching the limit, Medicare Advantage plans pay 100% of eligible expenses.
What is the maximum out-of-pocket?
What is an out-of-pocket maximum? An out-of-pocket maximum is a predetermined, limited amount of money that an individual must pay before an insurance company or (self-insured health plan) will pay 100% of an individual's covered health care expenses for the remainder of the year.
What is the maximum out-of-pocket for Medicare in 2020?
The maximum limits will increase to $7,550 for in-network and $11,300 for in- and out-of-network combined. Once the limit is reached, the plan covers any costs for the remainder of the year.
What is the highest rated Medicare Advantage plan?
Best Medicare Advantage Plans: Aetna Aetna Medicare Advantage plans are number one on our list. Aetna is one of the largest health insurance carriers in the world. They have an AM Best A-rating. There are multiple plan types, like Health Maintenance Organizations (HMOs) or Preferred Provider Organizations (PPOs).
What is the Maximum Medicare Out-of-Pocket Limit for in 2022?
Many people are surprised to learn that Original Medicare doesn’t have out-of-pocket maximums. Original Medicare consists of two parts — Part A and...
What is the Medicare out-of-pocket maximum ?
Let’s face it, higher-than-expected medical bills can happen to anyone, even those in perfect health. That’s a scary reality we hope won’t happen t...
How Much do Medicare Patients Pay Out-of-Pocket?
To summarize, Medicare beneficiaries pay varying out-of-pocket amounts, based upon the type of coverage they have.
What’s included in the out-of-pocket maximum for Medicare Part C plans?
The costs you pay for covered healthcare services all go towards your Part C out-of-pocket maximum. These include:
How much can you save if you don't accept Medicare?
If you are enrolled in Original Medicare, avoiding health care providers who do not accept Medicare assignment can help you save up to 15 percent on excess charges. Read additional medicare costs guides to learn more about Medicare costs and how they will affect you.
How much is Medicare Part B?
Part B. The standard Medicare Part B premium is $148.50 per month. However, the Part B premium is based on your reported taxable income from two years prior. The table below shows what Part B beneficiaries will pay for their premiums in 2021, based off their 2019 reported income. Medicare Part B IRMAA.
What is a Medigap plan?
These plans, also known as “ Medigap ,” provide coverage for some of Medicare’s out-of-pocket costs, such as deductibles, coinsurance and copayments. Some Medigap plans even include annual out-of-pocket spending limits. Sign up for a Medicare Advantage plan.
How much is the deductible for Part D in 2021?
Part D. Deductibles vary according to plan. However, Part D deductibles are not allowed to exceed $455 in 2021, and many Part D plans do not have a deductible at all. The average Part D deductible in 2021 is $342.97. 1.
How much coinsurance is required for hospice?
A 5 percent coinsurance payment is also required for inpatient respite care. For durable medical equipment used for home health care, a 20 percent coinsurance payment is required.
How much is a copayment for a mental health facility?
For an extended stay in a hospital or mental health facility, a copayment of $371 per day is required for days 61-90 of your stay, and $742 per “lifetime reserve day” thereafter.
Do you have to pay coinsurance on Medicare?
Medicare coinsurance and copayments. Once you meet your deductible, you may have to pay coinsurance or copayments when you receive care. A coinsurance is a percentage of the total bill, while a copayment is a flat fee.
Does Medicare Advantage cover dental?
Medicare plans cover a wide range of medical services. Medicare Advantage often pays for even more, including services not covered by traditional Medicare, such as dental and vision coverage. But that doesn't mean your medical care will be completely free, which is where co-pays and other out-of-pocket expenses come in.
Do Medicare beneficiaries have to pay for Part B?
Medicare beneficiaries have to pay a premium for Part B medical insurance. Those who choose Medicare Advantage also have to pay premiums. The monthly cost of premiums depends on the specific plan you choose, as well as the type of plan.
What happens if a doctor doesn't accept my insurance?
And, if the doctor doesn’t accept the policy, you don’t have coverage. Any expense you incur that doesn’t have coverage won’t apply to your maximum out of pocket. Further, that service will be 100% your bill. Some choose PPO plans to have some coverage outside the plan.
Does Medigap have a maximum out of pocket?
Medigap plans don’t have a maximum out of pocket because they don’t need one. The coverage is so good you’ll never spend $5,000 a year on medical bills. Sure, the premium is a little higher, but the benefits are more significant. If high medical bills are your concern, consider choosing Medigap.
Is there a limit on Medicare 2021?
Updated on July 13, 2021. There isn’t a maximum out of pocket on Medicare. Because of this, there is no limit to the amount you can pay in medical bills. You can contribute 20% of any number of costs after meeting the deductible. Don’t worry, though; we have a few solutions to help you.
Can you pay Medicare out of pocket?
No, with Medicare you can pay any amount out of pocket on medical bills. So, those with chronic health conditions can expect to pay endlessly on coinsurances with Medicare. There is no Part A or Part B maximum out of pocket.
Does Medicare cover surgery?
Medicare doesn’t have a limit on the amount you can spend on healthcare. But, they do cover a portion of most medical bills. Yes, there is some help, but 20% of $100,000+ surgery or accident could be bank-breaking. But, there are options to supplement your Medicare. Some options have a maximum limit. Yet, some options don’t.
Does Medicare Part A have an out-of-pocket maximum?
As previously mentioned, Medicare Part A and Medicare Part B do not have an out-of-pocket maximum. Technically speaking, beneficiaries who have Original Medicare coverage are responsible for a potentially very high amount of out-of-pocket costs (such as deductibles and copays) in a year.
Does Medicare Advantage have out-of-pocket limits?
All Medicare Advantage plans and Part D drug plans include out-of-pocket maximums (spending limits). Original Medicare (Parts A and B), which is provided by the government, doesn’t. Learn how the out-of-pocket maximums for each part of Medicare.
What is the Medicare Advantage spending limit?
Medicare Advantage (Medicare Part C) plans, however, do feature an annual out-of-pocket spending limit for covered Medicare expenses. While each Medicare Advantage plan carrier is free to set their own out-of-pocket spending limit, by law it must be no greater than $7,550 in 2021. Some plans may set lower maximum out-of-pocket (MOOP) limits.
What is Medicare Advantage Plan?
When you enroll in a Medicare Advantage plan, it replaces your Original Medicare coverage and offers the same benefits that you get from Medicare Part A and Part B.
What is the Medicare donut hole?
Medicare Part D prescription drug plans feature a temporary coverage gap, or “ donut hole .”. During the Part D donut hole, your drug plan limits how much it will pay for your prescription drug costs. Once you and your plan combine to spend $4,130 on covered drugs in 2021, you will enter the donut hole. Once you enter the donut hole in 2021, you ...
How much is Medicare Part A deductible in 2021?
You are responsible for paying your Part A deductible, however. In 2021, the Medicare Part A deductible is $1,484 per benefit period. During days 61-90, you must pay a $371 per day coinsurance cost (in 2021) after you meet your Part A deductible.
What happens if you spend $6,550 out of pocket in 2021?
After you spend $6,550 out-of-pocket on covered drugs in 2021, you leave the donut hole coverage gap and enter the catastrophic coverage stage. Once you reach this stage, you only pay a small coinsurance or copayment for your covered drugs for the rest of the year.
What is Medicare Part B and Part D?
Medicare Part B (medical insurance) and Part D have income limits that can affect how much you pay for your monthly Part B and/or Part D premium. Higher income earners pay an additional amount, called an IRMAA, or the Income-Related Monthly Adjusted Amount.
How long does Medicare cover hospital care?
Depending on how long your inpatient stay lasts, there is a limit to how long Medicare Part A will cover your hospital costs. For the first 60 days of ...