What is the primary role of MDS?
What kind of primary care physician do you need?
- Family doctors. These physicians treat patients of all ages. ...
- Internists. Doctors who practice internal medicine specialize in treating adults. ...
- Pediatricians. Pediatricians complete special training that focuses on wellness, development, and treatment of the conditions that can affect babies, children, and teenagers up to the age of 21.
- Geriatricians. ...
What does MDS stand for?
- Important Facts About This Occupation
- Professional Training Requirements. To be an MDS coordinator, you must at least be a licensed practical nurse (LPN); many facilities require one be a registered nurse (RN) with some experience, ...
- Employment Outlook and Salary Expectations. ...
How can I become MDS certified?
MDS coordinators need a strong skill set that includes:
- People skills: The ability to converse comfortably with different types of people
- Compassion: Empathy for challenges others are facing
- Patience: The ability to handle lengthy interviews and slow responses
- Communication: Ability to convey information verbally and in writing
- Data entry: Handle large amounts of information in an organized manner
How to complete MDS assessment?
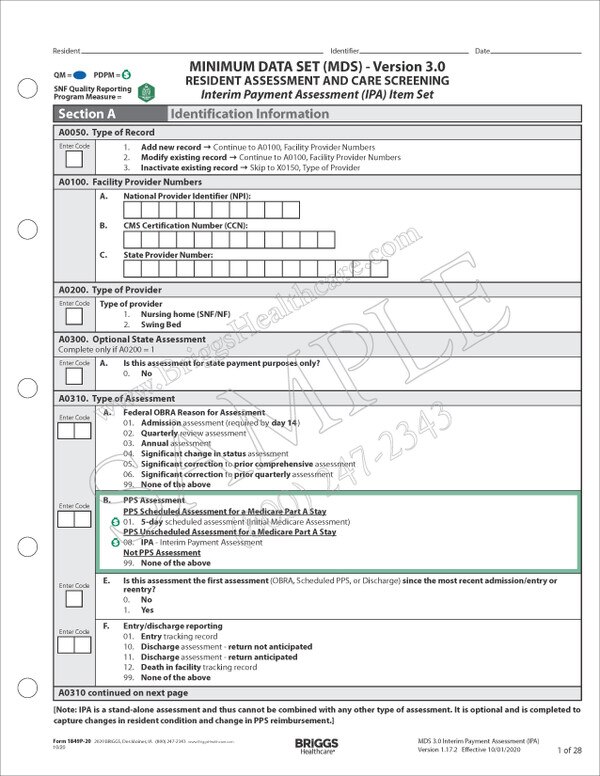
- Minimum Data Set (MDS) 3.0 background
- Assessments overview
- Factors affecting the assessment schedule
- Assessment results reporting
- Resources

What is the purpose of a MDS?
The Minimum Data Set (MDS) is part of a federally mandated process for clinical assessment of all residents in Medicare or Medicaid certified nursing homes. This process entails a comprehensive, standardized assessment of each resident's functional capabilities and health needs.
What is collected in MDS?
The MDS system collects data on the physical, psychological, and psychosocial functioning of all residents of long-term facilities certified by Medicare or Medicaid.
What is MDS section?
The Minimum Data Set (MDS) is part of the federally-mandated process for assessing individuals receiving care in certified skilled nursing facilities regardless of payer source. The process provides a comprehensive assessment of individuals' current health conditions, treatments, abilities, and plans for discharge.
Who uses MDS?
The Minimum Data Set (MDS) is a standardized assessment tool that measures health status in nursing home residents. MDS assessments are completed every 3 months (or more often, depending on circumstances) on nearly all residents of nursing homes in the United States.
How is MDS used to determine the payment a healthcare facility receives?
The MDS assessment data is used to calculate the RUG-III Classification necessary for payment. The MDS contains extensive information on the resident's nursing needs, ADL impairments, cognitive status, behavioral problems, and medical diagnoses.
Does the MDS link to reimbursement?
The MDS (Minimum Data Set) is a direct link to reimbursement, consumer ratings and interdisciplinary teamwork.
What is MDS diagnosis?
Myelodysplastic syndromes (MDS) are an often unrecognized, under-diagnosed rare group of bone marrow failure disorders, where the body no longer makes enough healthy, normal blood cells in the bone marrow. The disease is also known as a form of blood cancer.
What does MDS stand for in a nursing home?
Minimum Data SetThe Minimum Data Set (MDS) is part of the federally mandated process for clinical assessment of all residents in Medicare and Medicaid certified nursing homes. This process provides a comprehensive assessment of each resident's functional capabilities and helps nursing home staff identify health problems.
What is the current version of MDS?
MDS 3.0 RAI Manual v1. 17.1, effective October 1, 2019 (posted September 2019) This is the final version and went into effect October 2019, and due to the COVID-19 public health emergency continues to be in effect without changes for fiscal year 2021 (starting Oct. 1, 2020).
Who has the primary responsibility for the accuracy of the MDS?
Legally, it is an attestation of accuracy with the primary responsibility for its accuracy with the person selecting the MDS item response. Each person completing a section or portion of a section of the MDS is required to sign the Attestation Statement.
What are different types of MDS assessments?
Type of Assessment.A. Federal OBRA Reason for Assessment. Admission assessment (required by day 14).Quarterly review assessment. Annual assessment.Significant change in status assessment. Significant correction to prior comprehensive assessment.Significant correction to prior quarterly assessment. None of the above.
How soon after a resident is admitted does an MDS need to be completed by a nurse?
The timing requirements for a comprehensive assessment apply to both completion of the MDS (R2b) and the completion of the RAPs (VB2). For example, an Admission assessment must be completed within 14 days of admission. This means that both the MDS and the RAPs (R2b and VB2 dates) must be completed by day 14.
Massachusetts MDS Section S
Massachusetts implemented state specific MDS Section S items effective April 1, 2012. Please see the documents below for more information.
Contact us
For more information on MDS issues, please contact one of the following staff at the Division of Health Care Facility Licensure and Certification:
MDS Automation Coordinator
Contact the MDS Automation Coordinator for questions on the transmission of the MDS to the federal database.
What is an MDS assessment?
An MDS, or minimum data set, assessment is used by nursing homes to assess and plan care for patients. Nursing homes that are certified by Medicare must perform assessments as required by Medicare, Medicaid and the Omnibus Budget Reconciliation Act -- OBRA -- of 1987. An MDS assessment provides a standardized set of information ...
What is the evaluation of a patient?
Patients are evaluated on their communication ability, including clarity of speech and use of a hearing aid. Other data include the patient's relationships with other residents and the amount of assistance the patient needs for daily tasks such as eating and bathing.
Do nursing homes have to have MDS?
If a nursing home is not certified by Medicare, residents are not required to undergo MDS assessments. If MDS assessments are required, the facility is responsible for backing up data so that data can be recovered in case of fire, floods or damage to software and hardware.
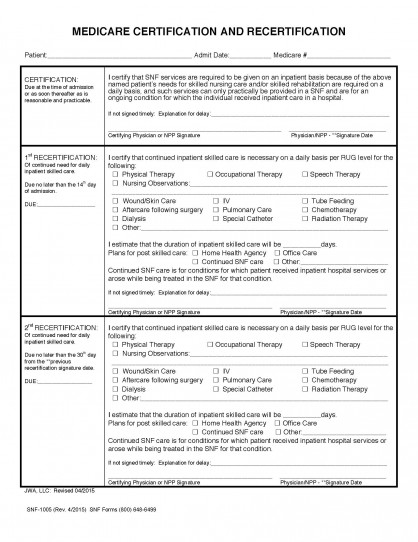
What is a PPS discharge assessment?
Effective October 1st, Medicare requires a Medicare Part A PPS Discharge Assessment. This MDS contains the required data elements used to calculate current and future Skilled Nursing Facility Quality Reporting Program (SNF QRP) quality measures under the IMPACT Act. The IMPACT Act directs the Secretary to specify quality measures on which post-acute care (PAC) providers (which includes SNFs) are required to submit standardized patient assessment data. Section 1899B (2) (b) (1) (A) (B) of the Act delineates that patient assessment data must be submitted with respect to a resident’s admission to and discharge from a Medicare Part A Assessment.
When is a Medicare Part A discharge MDS required?
In other words, the Medicare Part A Discharge MDS is required any time a Medicare Part A stays ends with the only exception being when a patient expires during a Part A stay. Note that section GG is not required and will not appear on the MDS for any unplanned discharges (e.g. unexpected acute care hospital discharges).
When is Medicare Part A PPS discharge completed?
The Medicare Part A PPS Discharge MDS is completed when a patient’s Medicare Part A stay ends: When the Medicare Part A stay ends and the patient remains in the facility. When the Medicare Part A stay ends and the patient is physically discharged from the facility (the Part A PPS and OBRA Discharge assessments may be combined in this situation) ...
How to contact Harmony Healthcare International?
You can contact harmony by clicking here or calling 800.530.4413.
What is the impact act?
The IMPACT Act directs the Secretary to specify quality measures on which post-acute care (PAC) providers (which includes SNFs) are required to submit standardized patient assessment data. Section 1899B (2) (b) (1) (A) (B) of the Act delineates that patient assessment data must be submitted with respect to a resident’s admission to ...
Is A2400C equal to ARD?
The ARD must be equal to the date recorded in section A2400C. The only exception is when the End Date of the Most Recent Medicare Stay (A2400C) occurs on the day of or day before the Discharge Date (A2000). In this situation the OBRA Discharge assessment and Part A PPS Discharge assessment are both required and may be combined with an ARD equal ...
What is the OBRA code for MDS?
OBRA assessments are coded in A0310A of the MDS assessment form.
Can Medicare SNF PPS assessments be transmitted late?
In the event that the assessments become necessary for Medicare SNF PPS reimbursement, they can be transmitted late as long as they were performed in the correct timeframes.
Can you submit assessments to MA insurance?
If the beneficiary has an MA plan, CMS suggests that you may want to submit the assessments to the MA insurance carrier. The insurance carrier usually pays under contract to the facility. Therefore, it would not be appropriate to routinely submit any and all assessments. We all need to follow the specific guidelines.
What happens if SNF fails to set ARD?
If the SNF fails to set the ARD within the defined ARD window for a Medicare-required assessment, including the grace days, and the resident is still on Part A, the SNF must complete a late assessment. The ARD can be no earlier than the day the error was identified.
What is missed assessment in Medicare?
An assessment is considered to be missed when the SNF does not set the ARD within the prescribed window and the patient is no longer on Medicare Part A services. If the patient has already been discharged from Medicare Part A services prior to the discovery of the omission of the assessment the facility may not perform the assessment.
What is the MDS in PPS?
The MDS is the cornerstone of PPS reimbursement methodology and is used to classify residents into resource utiliza tion groups (RUG’s) that in turn sets the rate of reimbursement. The MDS contains extensive information on the resident’s nursing needs, ADL impairments, cognitive status, behavioral problems, and medical diagnoses.
What is Medicare group therapy?
For Medicare Part A group therapy is defined as a group of four participants working on the same activity. The group may be led by a professional therapist or a PTA or COTA who is under the professional therapist’s supervision. The total number of minutes spent is captured individually on each group member’s MDS.
What is a short stay policy?
The short stay policy allows the assignment into a Rehabilitation Plus Extensive Services or Rehabilitation category when a resident received rehabilitation therapy and was not able to have received five days of therapy due to discharge from Medicare Part A.
What changes affect Medicare schedule?
The Medicare schedule is also affected by clinical changes in the patients care, including changes in the intensity of therapy rendered. The Medicare schedule is altered if one of the following occurs: Discharge and/or readmission to the SNF. Death of a resident. Late or Missed assessment.
How many days does Medicare require assessments?
In accordance with the Final Rule, Medicare requires scheduled assessments on days 5, 14, 30, 60 and 90. Each assessment pre-determines a specific number of billable days. Not all residents will complete the regular assessment schedule.