The index is obtained by computing the ratio of the Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
How do doctors get paid from Medicaid?
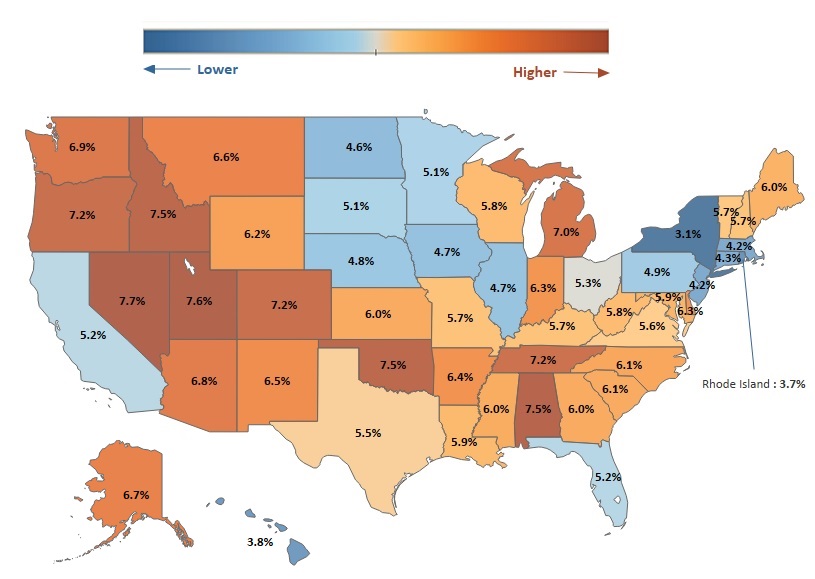
Medicaid pays about 61% of what Medicare pays, nationally, for outpatient physician services. The payment rate varies from state to state, of course. But if 61% is average, you can imagine how ...
What percent does Medicaid pay?
Medicare for most people will only cover 80 percent of the medical costs. Medicare will usually discount a physician or hospital charges and then paid 80 percent of the adjusted cost. The patient will be required to pay the remaining 20 percent either out-of-pocket or through the use of a supplemental policy.
How much does Medicaid reimburse?
the american hospital association (aha) estimated that medicaid payments to hospitals amounted to 90 percent of the costs of patient care in 2013, while medicare paid 88 percent of costs; by...
How does the federal government funds Medicaid?
The federal government guarantees matching funds to states for qualifying Medicaid expenditures; states are guaranteed at least $1 in federal funds for every $1 in state spending on the program.
What is a CMS fee?
CMS develops fee schedules for physicians, ambulance services, clinical laboratory services, and durable medical equipment, prosthetics, orthotics, and supplies.
How are Medicare fees calculated?
Calculating 95 percent of 115 percent of an amount is equivalent to multiplying the amount by a factor of 1.0925 (or 109.25 percent). Therefore, to calculate the Medicare limiting charge for a physician service for a locality, multiply the fee schedule amount by a factor of 1.0925.
What is Medicare's reimbursement rate?
roughly 80 percentAccording to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill. Not all types of health care providers are reimbursed at the same rate.
What will Irmaa be in 2021?
The maximum IRMAA in 2021 will be $356.40, bringing the total monthly cost for Part B to $504.90 for those in that bracket. The top IRMAA bracket applies to married couples with adjusted gross incomes of $750,000 or more and singles with $500,000 or more of income.
What is CMS conversion factor?
CMS has recalculated the MPFS payment rates and conversion factor to reflect these changes. The revised MPFS conversion factor for CY 2021 is 34.8931.
What is the Medicare conversion factor for 2021?
$34.8931This represents a 0.82% cut from the 2021 conversion factor of $34.8931. However, it also reflects an increase from the initial 2022 conversion factor of $33.5983 announced in the 2022 Medicare physician fee schedule final rule.
How much is an RVU worth in 2022?
The new 2022 conversion factor is $34.6062. (The conversion factor is multiplied by the RVUs to calculate the dollar reimbursement amount.) The estimated impact of these and other adjustments on the allergy/immunology specialty is 0.8% overall decrease in Medicare payments for 2022, compared to 2021.
Who determines RVU?
The Specialty Society Relative Value Scale Update Committee (also known as the RUC) determines the RVUs for each new code and revalues existing codes on a five-year schedule to reflect changes in costs and technology.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
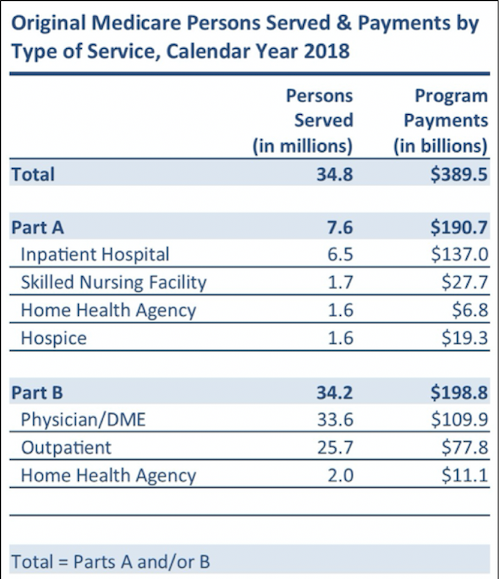
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
Can you spend down on medicaid?
Medicaid spenddown. Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid . The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
What is Medicare fee schedule?
The organization that manages the Medicare program, Centers for Medicare & Medicaid Services (CMS), describes the Medicare fee schedule as a comprehensive list of maximum fees used by Medicare to reimburse physicians, other healthcare providers and suppliers.
When is the Medicare Physician Fee Schedule Final Rule?
The Medicare Physician Fee Schedule Final Rule for the calendar year of 2020 has been displayed at the Federal Register since November 1, 2019. It includes payment policies, rates and other elements for services provided under the Medicare Physician Fee Schedule (MPFS).
What percentage of Medicare deductible do you pay when you visit a doctor?
After meeting the Part B deductible, patients will usually pay 20% of the Medicare-approved amount for most services delivered by a physician.
What is AFS in Medicare?
The Ambulance Fee Schedule (AFS) is a national fee schedule for ambulance services provided as part of the Medicare benefits under the provisions of Part B. These services include volunteer, municipal, private, independent and institutional providers as well as skilled nursing facilities.
What is Medicare insurance?
Medicare. Medicare is an insurance program. Medical bills are paid from trust funds which those covered have paid into. It serves people over 65 primarily, whatever their income; and serves younger disabled people and dialysis patients. Patients pay part of costs through deductibles for hospital and other costs.
Do you pay for medical expenses on medicaid?
Patients usually pay no part of costs for covered medical expenses. A small co-payment is sometimes required. Medicaid is a federal-state program. It varies from state to state. It is run by state and local governments within federal guidelines.
Is Medicare a federal program?
Small monthly premiums are required for non-hospital coverage. Medicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government.
Who pays for medicaid?
The Medicaid program is jointly funded by the federal government and states. The federal government pays states for a specified percentage of program expenditures, called the Federal Medical Assistance Percentage (FMAP) .
Can states fund Medicaid?
States must ensure they can fund their share of Medicaid expenditures for the care and services available under their state plan. States can establish their own Medicaid provider payment rates within federal requirements, and generally pay for services through fee-for-service or managed care arrangements.