When should a Medicare ABN be given?
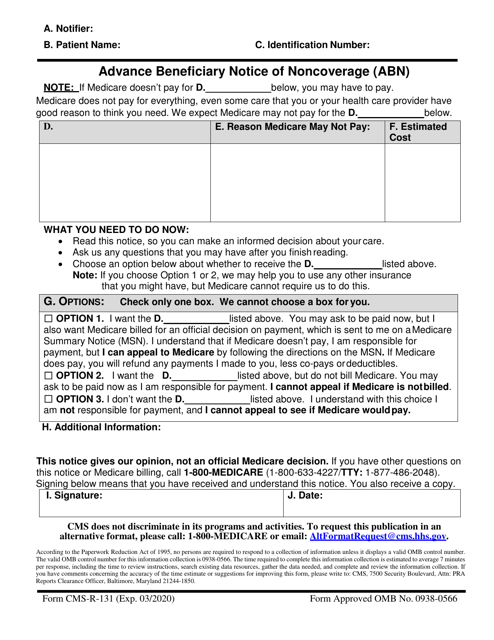
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying you: Medicare may deny payment for that specific procedure or treatment You will be personally responsible for full payment if Medicare denies payment
Do Medicare replacement plans require an ABN?
Jan 21, 2022 · An Advance Beneficiary Notice (ABN) is a formal notification that Medicare may not pay for a certain item or service. ABNs are important because they help you make informed Medicare coverage decisions and prepare for any costs you might incur.
How to use the Medicare ABN to your advantage?
Dec 01, 2021 · The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, is issued by providers (including independent laboratories, home health agencies, and hospices), physicians, practitioners, and suppliers to Original Medicare (fee for service - FFS) beneficiaries in situations where Medicare payment is expected to be denied. The ABN is issued in order to …
Does Medicaid have ABN?
Advance Beneficiary Notice of Non-coverage (ABN) OMB Approval Number: 0938-0566 Overview The ABN is a notice given to beneficiaries in Original Medicare to convey that Medicare is not likely to provide coverage in a specific case. “Notifiers” include: • Physicians, providers (including institutional providers like outpatient hospitals),
What does Medicare ABN stand for?
The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, is issued by providers (including independent laboratories, home health agencies, and hospices), physicians, practitioners, and suppliers to Original Medicare (fee for service - FFS) beneficiaries in situations where Medicare payment is expected to be ...Dec 1, 2021
What services require an ABN for Medicare?
You must issue an ABN: When a Medicare item or service isn't reasonable and necessary under Program standards, including care that's: Not indicated for the diagnosis, treatment of illness, injury, or to improve the functioning of a malformed body member. Experimental and investigational or considered research only.
What is a patient ABN?
An ABN is a Medicare waiver of liability that providers are required to give a Medicare patient for services provided that may not be covered or considered. medically necessary. An ABN is used when service(s) provided may not be reimbursed by Medicare.
When must a patient have an ABN?
An ABN is required when an item or service is expected to be denied. This may occur at any one of three points during a course of treatment which are initiation, reduction and termination, also known as "triggering events."Oct 11, 2021
What is an ABN and what is its purpose?
An ABN is a unique 11 digit number that identifies your business to the government and community. You can use an ABN to: identify your business to others when ordering and invoicing. avoid pay as you go (PAYG) tax on payments you get.Mar 10, 2021
Is an ABN only for Medicare patients?
Medicare has defined the use of the ABN into two categories: required and voluntary. The service or item is a benefit of Medicare (normally payable) but due to restricted coverage will not be paid.Sep 25, 2017
Is ABN for Medicare Part A or B?
Therefore, an ABN is used for services rendered to Original Medicare FFS (Part A and Part B) enrollees. That means an ABN is not required for Medicare Part C and Part D. When the services are not covered, then patient is responsible for UMDAP amount or cost of services, whichever is less.
Why is ABN important to the patient?
An ABN is important because it allows a provider to administer a service to a Medicare patient that may not be covered by Medicare.Mar 8, 2018
Is an ABN required if Medicare is secondary?
The ABN needs to be on file for the year that the patient is responsible for paying. If the patient fits Medicare's guidelines for “high risk” they are allowed to have the pap every 12 months and no ABN is required.Nov 19, 2009
What Is A Medicare Waiver/Advance Beneficiary Notice (ABN)?
An ABN is a written notice from Medicare (standard government form CMS-R-131), given to you before receiving certain items or services, notifying y...
If I Receive An ABN Form, What Are My Options?
You have the option to receive the items or services or to refuse them. In either case, you should choose one option on the form by checking the bo...
What If I Refuse to Sign An ABN, but I Want The Items Or Services Anyway?
If you refuse to sign, one of two actions will take place: 1. Mayo Clinic may decide not to provide the items or services. 2. A second person will...
When I Am Liable For Payment Because I Signed An ABN, How Much Can I Be charged?
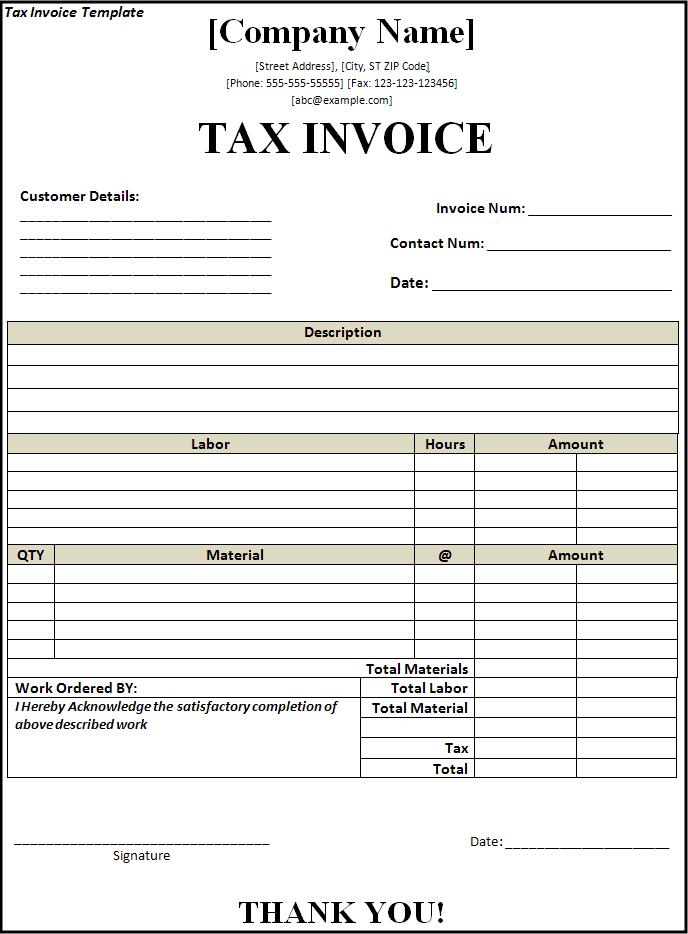
When you sign an ABN and become liable for payment, you will have to pay for the item or service yourself, either out of pocket or by some other in...
Why Do I Routinely Receive An ABN For Certain Items Or Services?
Certain items or services that are covered by Medicare are only covered up to a certain number of times within a specified amount of time. Examples...
Do Abns Mean That Medicare Is Reducing Coverage?
No. ABNs do not operate to reduce coverage at all. Only if and when Medicare does deny the claim, do you become liable for paying personally for th...
Who Do I Contact If I Have More Questions About My Medicare Coverage?
For more information about your Medicare coverage, please contact Medicare directly: 1. Phone: 800-633-4227 (toll-free) 2. Website: www.medicare.go...
When Does Medicare Issue An Advance Beneficiary Notice?
The Centers of Medicare & Medicaid Services (CMS) issues advance beneficiary notices to make you aware when you may be personally responsible for paying for a medical service.
How Long Is an Advance Beneficiary Notice (ABN) in Effect?
An ABN remains in effect after valid delivery if there haven’t been any changes to the care described in the original notice and no changes to your health status that would require a change in the subsequent treatment for your non-covered condition.
What Should I Do If I Receive an Advance Beneficiary Notice?
If you receive an ABN, you have three options in terms of how you can respond.
Compare Medigap plans in your area
Lisa Eramo is an independent health care writer whose work appears in the Journal of the American Health Information Management Association, Healthcare Financial Management Association, For The Record Magazine, Medical Economics, Medscape and more.
What is an ABN?
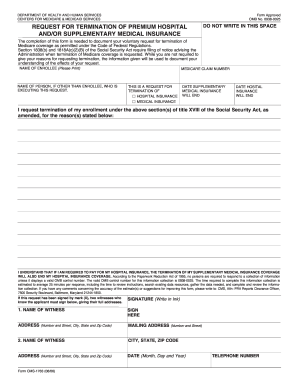
The ABN is a formal information collection subject to approval by the Executive Office of Management and Budget (OMB) under the Paperwork Reduction Act of 1995 (PRA). As part of this process, the notice is subject to public comment and re-approval every 3 years. With the latest PRA submission, a change has been made to the ABN. In accordance with Title 18 of the Social Security Act, guidelines for Dual Eligible beneficiaries have been added to the ABN form instructions.
Who completes the signature box on an ABN?
Once the beneficiary reviews and understands the information contained in the ABN, the Signature Box is to be completed by the beneficiary (or representative). This box cannot be completed in advance of the rest of the notice.
What is an advance benefit notice for skilled nursing?
A skilled nursing facility may send you a Skilled Nursing Facility ABN if there is a chance that your care or a long-term stay in a facility will not be covered by Medicare Part A. This type of ABN may also be issued if your stay is considered custodial care.
What is an ABN in Medicare?
An advance beneficiary notice of noncoverage (ABN) lets you know when Medicare may not cover an item or service. You must respond to an ABN in one of three ways. If a claim has been denied for Medicare coverage, you have the right to appeal the decision.
What is an ABN?
What is an Advance Beneficiary Notice of Noncoverage (ABN)? An Advance Beneficiary Notice of Noncoverage (ABN) is a liability waiver form that is given when a healthcare provider or medical supply company thinks or knows Medicare will not cover something. An ABN will explain:
How long does it take to appeal a Medicare claim?
If your claim is denied by Medicare, you can file an appeal. Here are a few things you need to know: You must file the appeal within 120 days of receiving your Medicare summary notice, which will have your appeal information on it.
What does it mean to sign an ABN?
By signing an ABN, you are agreeing to the fees that may come with the items and services you are receiving. You are also accepting responsibility to pay for the item or service, even if Medicare denies the claim and will not reimburse you.
How long does it take to get a decision from Medicare?
Once you have filed an appeal, you should get a decision within 60 days of your request being received.
What to do if you receive an ABN?
If you have received an ABN, you must respond to confirm how you’d like to proceed. There are three different options to choose from: You want to continue receiving the items or services that may not be covered by your Medicare plan.
What is an ABN in Medicare?
The ABN allows you to decide whether to get the care in question and to accept financial responsibility for the service (pay for the service out-of-pocket) if Medicare denies payment. The notice must list the reason why the provider believes Medicare will deny payment.
What is an ABN waiver?
An Advance Beneficiary Notice (ABN), also known as a waiver of liability, is a notice a provider should give you before you receive a service if, based on Medicare coverage rules, your provider has reason to believe Medicare will not pay for the service.
How to get an official decision from Medicare?
To get an official decision from Medicare, you must first sign the ABN, agreeing to pay if Medicare does not, and receive the care. Make sure you request that your provider bills Medicare for the service before billing you (the ABN may have a place on the form where you can elect this option).
Did not receive ABN before service?
You did not receive an ABN from your provider before you were given the service or item; Your provider had reason to believe your service or item would not be covered by Medicare; Your item or service is not specifically excluded from Medicare coverage; and. Medicare has denied coverage for your item or service.
Can you be responsible for denied charges?
You may not be responsible for denied charges if the ABN: Is difficult to read or hard to understand. Is given by the provider (except a lab) to every patient with no specific reason as to why a claim may be denied. Does not list the actual service provided, or is signed after the date the service was provided.
What is a Medicare ABN form?
An ABN form is a written notice that Medicare may not, or will not, pay for services or items recommended by your doctor, healthcare provider or supplier. The form includes the items or services that Medicare isn't expected to pay for, the reasons why and an estimate of the costs.
When will I be given a Medicare ABN form?
Your doctor, healthcare provider or supplier must deliver the ABN form before providing the recommended items or services. In fact, it must be given far in advance so you have time to consider your options without feeling rushed. 1
What options do Medicare ABN forms provide?
ABN forms generally provide you with 3 options. Here are the actual options, plus some additional insight:
Other important facts
Medicare ABNs are for Original Medicare only—not Medicare Advantage plans.
The power of choice
Medicare ABN forms provide you with an opportunity to make informed decisions about your healthcare. For more information on how to fill out the form, check out these ABN form instructions provided by the Centers for Medicare & Medicaid Service (CMS).
What is an ABN in Medicare?
An ABN is a Medicare waiver of liability that providers are required to give a Medicare patient for services provided that may not be covered or considered. medically necessary. An ABN is used when service (s) provided may not be reimbursed by Medicare. If the healthcare provider believes that Medicare will not pay for some or all ...
What happens if you don't sign an ABN?
If there is no signed ABN then you cannot bill the patient and it must be written off if denied by Medicare.
What is an ABN for a primary care provider?
Examples of services that require an ABN include a visual field exam for an ophthalmologist, a pelvic exam for a primary care provider, or an echocardiogram. These exams should be covered as long as they ...
Who is Manny Oliverez?
+Manny Oliverez is a 25 year healthcare veteran having managed medical practices. He advises medical practices, physicians and practice administrators on how to run their practice and manage their medical billing and revenue cycle management. Manny speaks, blogs and makes videos at CaptureBilling.com, a blog that is tops in the medical billing and coding field. READ MORE
When should the provider issue an ABN to a Medicare patient?
Healthcare providers need to get signed the CMS-R-131 Advance Benefit Notice (ABN) from your Medicare patients in the following situation.
Why is ABN important to the Patient?
An ABN protects patient rights and informs Medicare that the patient knows about the provision of treatment and procedures performed by the healthcare provider.
Modifiers required to Medicare for Billing Signed ABN
Below is the list of relevant Medicare Modifiers as per CMS which can be used on the claim with CPT codes when ABN is signed.
What is a Medicare ABN?
Medicare’s Advance Beneficiary Notice (ABN) of Noncoverage is a form that you must issue to your office patients when you believe that Medicare may not pay or cover a proposed treatment, service, or item.
What is a Mandatory Medicare ABN?
Medicare requires you to issue an ABN to a patient when you have reason to believe that a proposed treatment, service, or item that Medicare typically covers, won’t be covered in the patient’s situation. This is considered a mandatory ABN, and you would use this type in the following situations:
What is a Voluntary Medicare ABN?
When you choose to issue an ABN even though it isn’t required by Medicare, you file a voluntary ABN. For example, you are not required to use an ABN for services that are not part of the Medicare program (statutorily excluded services) or with private payer patients, but you may choose to do so as a courtesy.
What are Medicare ABN Modifier Requirements?
There are so many different situations that can affect which ABN you should use. For example, do you know: