Private Medicare Advantage insurers didn’t have to follow the old Resource Utilization Group (RUG) model when deciding how to reimburse for skilled nursing services, and they don’t have to abide by the new Patient-Driven Payment Model (PDPM), either.
What is a Medicare rug level?
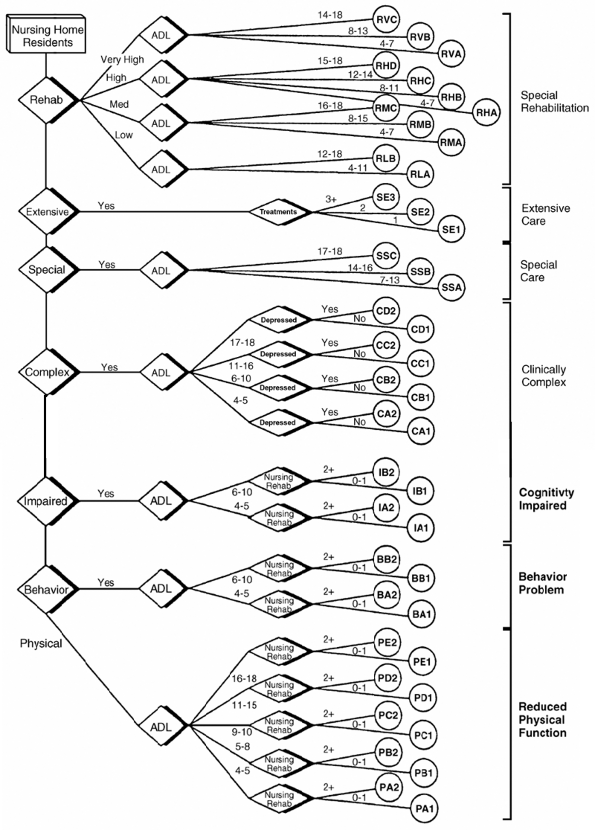
What Is a Medicare RUG Level? A RUG, or resource utilization group, is used to classify patients in long-term care facilities based on the care the patient requires, according to the Texas Department of Aging and Disability Services. As of 2014, there are 34 RUG groups.
What is a rug in long-term care?
A RUG, or resource utilization group, is used to classify patients in long-term care facilities based on the care the patient requires, according to the Texas Department of Aging and Disability Services.
What do Medicare Advantage plans cover?
, and usually Medicare drug coverage (Part D). Find Medicare Advantage Plans in your area. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like fitness programs (like gym memberships or discounts) and some vision, hearing, and dental services. Plans can also choose to cover even more benefits.
What is the rug refinement?
The aim of the "RUG Refinement" is to improve the ability of the existing RUG-III classification system to explain non-therapy ancillary (NTA) costs. The Urban Institute re-examined prior efforts by Abt Associates (2000) and Dr. Brant Fries (2003) using data from our 2001 analysis files and replicated and validated the research.

What does Medicare RUGs mean?
Medicare pays skilled nursing facilities based on a. prospective payment system that categorizes each resident into a. different group depending upon his or her care and resource needs. These groups are called RUGs, and each represents a different Medicare. payment rate.
What is a rug category?
Classifications from RUG-IV assigns patients to payment classification groups, called RUGs, within the payment components, based on various patient characteristics and the type and intensity of therapy services provided to the residents. Rehabilitation Plus Extensive Services. Rehabilitation.
What does rug mean in MDS?
Resource Utilization GroupsResource Utilization Groups, or RUGs, flow from the Minimum Data Set (MDS) and drive Medicare reimbursement to nursing homes under the Prospective Payment System (PPS). A resident is initially assigned to one of the seven major categories of RUGs based on their clinical characteristics and functional abilities.
Does Medicare still use RUGs?
New Medicare Payment Model, PDPM, Proposes to Replace RUGs System for SNFs. On April 27, 2018, the Centers for Medicare and Medicaid Services (CMS) announced a proposal to replace the Resource Utilization Groups (RUGs) payment system with a new model for Medicare payment of skilled nursing care.
What is Rug rate for Medicare?
The base rate for nontherapy RUGs is $16 and covers, for example, SNFs' costs for evaluating beneficiaries to determine whether they need therapy.
What does rug level stand for?
The RUG score shows the type and quantity of care required for each individual resident. RUG scores consist primarily of the levels of occupational, physical and speech therapy a patient receives along with the intensity of nursing services the patient requires.
Did PDPM replace rugs?
What is PDPM? Patient-Driven Payment Model. The Patient-Driven Payment Model (PDPM) is the proposed new Medicare payment rule for skilled nursing facilities. It is intended to replace the current RUG-IV system with a completely new way of calculating reimbursement.
What is Rbrvs healthcare?
The resource-based relative value scale (RBRVS) is the physician payment system used by the Centers for Medicare & Medicaid Services (CMS) and most other payers.
What is Medicare Advantage Plan?
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are an “all in one” alternative to Original Medicare. They are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, you still have. Medicare.
Does Medicare cover dental?
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
Final Report
This is the final report from the Urban Institute (March 2007) that describes data sources and methodological approaches used in the research of the RUG-III refinements.
Data
Updated RUG-53 Unadjusted Case Mix Indices --The updated nursing and therapy case mix index chart shows the distributional impact of adding 9 new groups to the RUG-III hierarchy. The addition of the new groups requires a recalibration of the case mix indices for all the RUG-III groups.
What is the SNF code?
All SNF claims must include Health Insurance Prospective Payment System (HIPPS) codes, which is a 5-digit code consisting of a 3-digit RUG-IV code and a 2-digit AI, for the assessments billed on the claim.
How long does it take for a Medicare Part A resident to return?
The Part A resident returns more than 30 days after a discharge assessment when return was anticipated. The resident leaves a Medicare Advantage (MA) Plan and becomes covered by Medicare Part A (the Medicare PPS schedule starts over as the resident now begins a Medicare Part A stay)
What is the PPS assessment schedule?
The Medicare-required PPS assessment schedule includes 5-day, 14-day, 30-day, 60-day, and 90-day scheduled assessments.
Where to send MDS 3.0 data?
You must transmit MDS 3.0 data to a Federal data repository, the QIES ASAP system. You must submit MDS 3.0 assessments and tracking records mandated under the OBRA and the SNF PPS. Do not submit assessments completed for purposes other than OBRA and SNF PPS requirements (for example, private insurance, including MA Plans). For more information on transmitting MDS 3.0 data to the QIES ASAP system, visit the MDS 3.0 Technical Information webpage and refer to Chapter 5 of the Long-Term Care Facility Resident Assessment Instrument 3.0 User’s Manual.
When do you have to complete the OBRA discharge assessment?
If the End Date of the Most Recent Medicare Stay (A2400C) occurs on the day of or one day before the Discharge Date ( A2000), you must complete the OBRA Discharge Assessment and the Part A PPS Discharge Assessment, and you may combine them.
What is default rate?
The default rate takes the place of the otherwise applicable Federal rate. It equals the rate paid for the RUG-IV group reflecting the lowest acuity level and is generally lower than the Medicare rate payable if the SNF submitted a timely assessment.
What is SNF in Medicare?
Medicare Part A covers skilled care in a Medicare-certified Skilled Nursing Facility (SNF). Skilled care is nursing or other rehabilitative services, furnished pursuant to physician orders, that: Require the skills of qualified technical or professional health personnel.
