What is the problem with Medicare Advantage?
Health Maintenance Organization (HMO) | Medicare Health Maintenance Organization (HMO) In HMO Plans, you generally must get your care and services from providers in the plan's network, except: Emergency care Out-of-area urgent care Out-of-area dialysis In some plans, you may be able to go out-of-network for certain services.
What are the advantages of Medicare Advantage?
What’s a Medicare Advantage Plan? You can get your Medicare benefits through Original Medicare, or a Medicare Advantage Plan (like an HMO or PPO). If you have Original Medicare, the government pays for Medicare benefits when you get them. Medicare Advantage Plans, sometimes called “Part C” or “MA Plans,” are offered by private companies
What are the advantages and disadvantages of HMO care?
Mar 31, 2022 · A Medicare HHMO plan is a type of Medicare Advantage Plan, an alternative to Original Medicare. An HMO provides you with access to your Medicare-covered services plus additional benefits through a specific network of physicians and facilities.
Why would a person choose a PPO over a HMO?
Jan 05, 2022 · How do Medicare Advantage HMO plans work? A health maintenance organization (HMO) gives you access to a network of doctors and hospitals that you must use in most cases. Some HMO plans require you to get a referral from a primary care physician for hospital care and specialist visits.

What is the difference between a HMO and a PPO Medicare Advantage plan?
There are differences between Medicare Advantage plans. The specific structure of the plan you choose dictates how much you pay for care and where you can seek treatment. HMO plans limit you to a specific network of providers, while PPO plans offer lower rates to beneficiaries who seek care from a preferred provider.
Is Medicare HMO the same as Medicare?
A Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan's network (except emergency care, out-of-area urgent care, or out-of-area dialysis).
What are the disadvantages of a Medicare Advantage plan?
Cons of Medicare AdvantageRestrictive plans can limit covered services and medical providers.May have higher copays, deductibles and other out-of-pocket costs.Beneficiaries required to pay the Part B deductible.Costs of health care are not always apparent up front.Type of plan availability varies by region.More items...•Dec 9, 2021
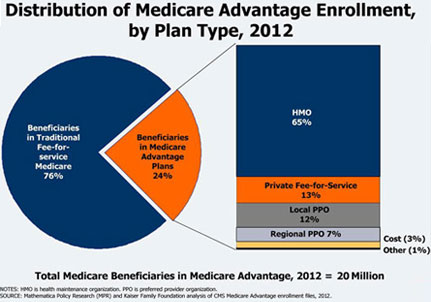
What are 4 types of Medicare Advantage plans?
Medicare Advantage PlansHealth Maintenance Organization (HMO) Plans.Preferred Provider Organization (PPO) Plans.Private Fee-for-Service (PFFS) Plans.Special Needs Plans (SNPs)
Is Medicare Advantage more expensive than Medicare?
Clearly, the average total premium for Medicare Advantage (including prescription coverage and Part B) is less than the average total premium for Original Medicare plus Medigap plus Part D, although this has to be considered in conjunction with the fact that an enrollee with Original Medicare + Medigap will generally ...Nov 13, 2021
What is the highest rated Medicare Advantage plan?
List of Medicare Advantage plansCategoryCompanyRatingBest overallKaiser Permanente5.0Most popularAARP/UnitedHealthcare4.2Largest networkBlue Cross Blue Shield4.1Hassle-free prescriptionsHumana4.01 more row•Feb 16, 2022
Why is Medicare Advantage being pushed so hard?
Advantage plans are heavily advertised because of how they are funded. These plans' premiums are low or nonexistent because Medicare pays the carrier whenever someone enrolls. It benefits insurance companies to encourage enrollment in Advantage plans because of the money they receive from Medicare.Feb 24, 2021
Can I change from Medicare Advantage to regular Medicare?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
Can I switch from Medicare to Medicare Advantage?
If you currently have Medicare, you can switch to Medicare Advantage (Part C) from Original Medicare (Parts A & B), or vice versa, during the Medicare Annual Enrollment Period. If you want to make a switch though, it may also require some additional decisions.
How can Medicare Advantage plans charge no premium?
Medicare Advantage plans are provided by private insurance companies. These companies are in business to make a profit. To offer $0 premium plans, they must make up their costs in other ways. They do this through the deductibles, copays and coinsurance.
Which is better a Medigap policy or Medicare Advantage plan?
Generally, if you are in good health with few medical expenses, Medicare Advantage is a money-saving choice. But if you have serious medical conditions with expensive treatment and care costs, Medigap is generally better.
Who is eligible for Medicare Advantage plans?
Who Qualifies for Medicare Advantage? You're eligible for a Medicare Advantage plan if you have Part A and Part B. Even those under 65 on disability may enroll! Further, you must live in the plan's service area and continue to pay your Part B premiums.Jan 18, 2022
What are the requirements for HMO?
In HMO Plans, you generally must get your care and services from providers in the plan's network, except: 1 Emergency care 2 Out-of-area urgent care 3 Out-of-area dialysis
What is network in health insurance?
network. The facilities, providers, and suppliers your health insurer or plan has contracted with to provide health care services. , you may have to pay the full cost. It's important that you follow the plan's rules, like getting prior approval for a certain service when needed.
What is Medicare HMO?
A Medicare HMO is one of several types of Medicare Advantage Plans available to Medicare beneficiaries. In order to sign up for a Medicare HMO plan an individual must first have signed up for Medicare Part A and Part B coverage.
Why do people choose HMO plans?
Health Maintenance Organization plans were created to offer cost savings to their beneficiaries, and the reduced expense is one of the primary advantages of selecting a Medicare HMO plan. Choosing an HMO reduces the need to fill out time-consuming paperwork or claim forms, as once the beneficiary provides their proof of insurance card at the point of service, there is no need to complete or submit any further claims. The beneficiary also has the security of knowing that their healthcare expenses will be limited to a fixed monthly premium; copayments and coinsurance charges vary depending upon the services received.
How long is the initial enrollment period?
The Initial Enrollment Period refers to a 7-month period that begins three months before the month you turn 65, the month in which you turn 65, and the three months after the month in which you turn 65. Initial Coverage Enrollment Period (ICEP). This enrollment period is for those enrolling in a Medicare Advantage plan.
Which is the least expensive Medicare plan?
Medicare HMO plans are generally among the least costly of the Medicare Advantage Plans. Continue reading to learn more about what these plans offer and whether one is right for you.
Who is Caren Lampitoc?
Caren Lampitoc is an educator and Medicare consultant for Medicare Risk Adjustments and has over 25 years of experience working in the field of Medicine as a surgical coder, educator and consultant.
Who is Ron Elledge?
Ron Elledge. Medicare Consultant and Author. Ron Elledge is a seasoned Medicare consultant and author of “Medicare Made Easy.”. As a Medicare expert, he regularly consults beneficiaries on Medicare rules, regulations, and strategies.
How does Medicare Advantage HMO work?
How do Medicare Advantage HMO plans work? A health maintenance organization (HMO) gives you access to a network of doctors and hospitals that you must use in most cases. Some HMO plans require you to get a referral from a primary care physician for hospital care and specialist visits.
What is a D-SNP?
Our dual-eligible Special Needs Plan (D-SNP) is a type of Medicare Advantage plan, available to people living in our service area who have both Medicare and Medicaid. We can help you find out if you qualify.
Does Aetna offer Medicare Advantage?
Medicare Advantage plans for every need. In addition to HMO plans, Aetna offers you other Medicare Advantage plan options — some with a $0 monthly plan premium. We can help you find a plan that’s right for you.
Does Aetna offer HMO?
In addition to HMO plans, Aetna offers you other Medicare Advantage plan options — some with a $0 monthly plan premium. We can help you find a plan that’s right for you.
Does Aetna require a primary care physician?
Our HMO plans. Requires you to use a provider network. Yes, unless it’s an emergency. Requires you to have a primary care physician (PCP) Yes, in many plans. Requires referral to see a specialist. Some plans. Monthly premiums.
What is MSA plan?
Medicare Medical Savings Account (Msa) Plan. MSA Plans combine a high deductible Medicare Advantage Plan and a bank account. The plan deposits money from Medicare into the account. You can use the money in this account to pay for your health care costs, but only Medicare-covered expenses count toward your deductible.
What is a special needs plan?
Special Needs Plans (SNPs) Other less common types of Medicare Advantage Plans that may be available include. Hmo Point Of Service (Hmopos) Plans. An HMO Plan that may allow you to get some services out-of-network for a higher cost. and a. Medicare Medical Savings Account (Msa) Plan.
Does Medicare Advantage include drug coverage?
Most Medicare Advantage Plans include drug coverage (Part D). In many cases , you’ll need to use health care providers who participate in the plan’s network and service area for the lowest costs.
What is an HMO POS plan?
A Medicare Advantage HMO plan with a POS option is known as an HMO-POS. This is a type of plan beneficiaries may choose for Medicare coverage. HMO-POS plans allow members to receive care outside of the plan’s network, but the cost of care will be more expensive. An HMO-POS policy has the flexibility of a PPO with restrictions like an HMO.
What is a point of service plan?
A health management organization with a point of service option is a type of Medicare Advantage plan, an alternative way to receive Medicare benefits. HMO-POS plans offer coverage for members that travel a lot within the country, different from the location restrictions of HMO plans.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare. You can also find her over on our Medicare Channel on YouTube as well as contributing to our Medicare Community on Facebook.
Do PPOs require referrals?
Unlike HMOs, PPOs don’t require referrals to visit with a specialist. Both HMO-POS and PPO plans allow members to visit with providers inside or outside of the plan’s network. However, the cost will be less when staying inside a plan’s network.
Where does John live?
Let’s use Johns’ situation for an example of how it works. John lives in New Mexico where he has Advantage HMO-POS coverage. He’s planning a trip to stay with his mother in Arizona for 2 months. John has several health concerns and wants to make sure he can visit with a doctor while he’s away from home.
What is Medicare Advantage HMO?
What is a Medicare Advantage HMO-POS plan? | 65 Incorporated. What does HMO-POS mean? HMO-POS stands for Health Maintenance Organization with a point-of-service option. This is one type of Medicare Advantage plan. An HMO-POS plan has features of an HMO plan. One is a defined list of providers, often referred to as a network, ...
What is the difference between HMO and POS?
However, there is one big difference. An HMO-POS plan allows members to use healthcare providers that are outside the plan’s network for some or all services.
What is an HMO plan?
Summary. Medicare health maintenance organization (HMO) plans are a type of Medicare Advantage plan. The plans are offered by private insurance companies, with varied coverage and costs. In this article, we discuss Medicare Advantage, look at the HMO plans, and examine how they compare with original Medicare.
What is Medicare Advantage?
Medicare Advantage plans combine the benefits of parts A and B and may offer prescription drug coverage. The Balanced Budget Act of 1997 added a new Part C to Medicare called the Medicare+choice program. It included various coordinated healthcare plans, including health maintenance organizations (HMOs). The Medicare+choice program is now known as ...
When is the open enrollment period for Medicare?
During the Medicare Advantage open enrollment period (OEP) from October 15 to December 7, a person can join, switch, or drop an Advantage plan.
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
What is Advantage Healthcare?
Advantage healthcare plans are offered by private companies that must follow Medicare rules and offer the same benefits as original Medicare (Part A and Part B). Many also offer prescription drug coverage.
Does HMO have a deductible?
An HMO-POS does not usually have a deductible for in-network providers and the copays may be low. When a person takes the HMO-POS option, they may have higher out-of-pocket costs. They may also have to pay most of the cost unless they have a referral from a doctor to the out-of-network provider.
Does HMO cover out of network care?
HMO plans have certain limitations and conditions: Most HMOs do not cover out-of-network care except in an emergency. If a person uses the services of a provider who is not in the network, they are responsible for the out-of-pocket costs.
How much does Medicare pay for each service?
You’ll generally pay 20% of the Medicare-approved amount for each item or service. A deductible may apply. Most people pay a monthly Part B premium. For both Medicare Part A and Part B to cover your services and items, providers must accept Medicare assignment.
What is Medicare Part A?
Original Medicare includes Part A and Part B. Medicare Part A ( hospital insurance ) typically covers: A deductible and coinsurance and/or copayments apply to most services.
Does Medicare cover prescriptions?
Original Medicare includes only limited prescription drug coverage. Part A may cover medications given to you as a hospital inpatient, and Part B may cover prescription drugs administered to you as an outpatient – generally those you wouldn’t take on your own (for example, intravenously administered medications).
Does Medicare cover home care?
Original Medicare doesn’t cover most medications you’d take at home, while a Medicare Advantage HMO plan might. You must continue paying your Medicare Part B premium, along with any premium the plan may charge.
Is hospice covered by Medicare Advantage?
A Medicare Advantage HMO plan delivers all your Medicare Part A and Part B benefits, except hospice care – but that’s still covered for you directly under Part A, instead of through the plan. Medicare Advantage plans are offered by private, Medicare-approved insurance companies.