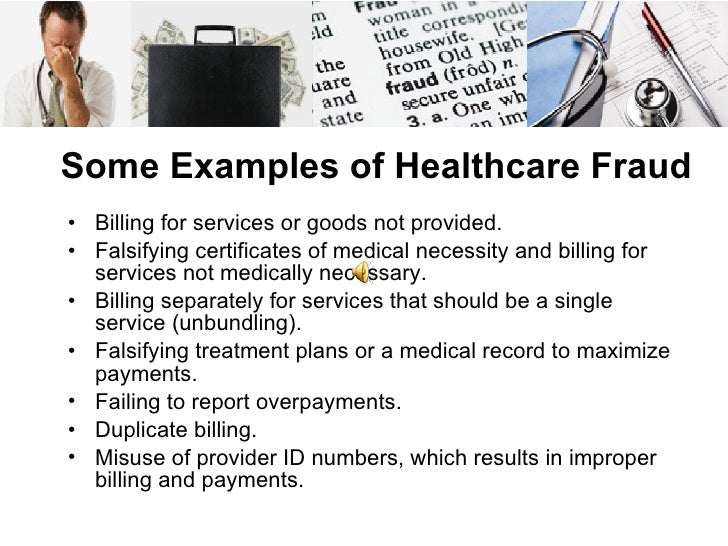
Common claims brought under Medicare abuse or fraud include:
- overbilling;
- unbundling services for higher reimbursement;
- assigning a code for a higher level of service than that which was actually performed;
- billing for patients who do not exist;
- submitting a code for a service that is covered under Medicare or Medicaid when the actual service was not covered; and
What are the most common types of Medicare fraud?
Dec 29, 2010 · Medicare and Medicaid fraud refer to illegal practices aimed at getting unfairly high payouts from government-funded healthcare programs. Key Takeaways Medicare and Medicaid fraud can be committed...
What are some examples of Medicare fraud?
Jul 02, 2019 · Medicare and Medicaid Fraud Overview Medicare and Medicaid fraud may take several forms, including phantom billing, patient billing, or upcoding and unbundling. In phantom billing fraud, the medical provider bills Medicare or Medicaid for procedures that either are never performed or are unnecessary.
What do you need to know about Medicare fraud?
Medicaid Fraud Medicaid fraud is the intentional providing of false information to get Medicaid to pay for medical care or services. Medical identity theft is one type of fraud. It involves using another person’s medical card or information to get health care goods, services, or funds. Below are other types of fraud, and provider and benef iciary examples.
Which is considered Medicare fraud?
Committing Medicare fraud exposes individuals or entities to potential criminal, civil, and administrative liability, and may lead to imprisonment, fines, and penalties. Criminal and civil penalties for Medicare fraud reflect the serious harms associated with health care fraud and the need for aggressive and appropriate intervention.

What are examples of Medicare fraud?
Additional examples of Medicare scams include: A person without Medicare coverage offering money or goods to a Medicare beneficiary in exchange for their Medicare number in order to use their Medicare benefits. A sales person offering a prescription drug plan that is not on Medicare's list of approved Part D plans.Dec 7, 2021
What happens if you do Medicare fraud?
Defrauding the Federal Government and its programs is illegal. Committing Medicare fraud exposes individuals or entities to potential criminal, civil, and administrative liability, and may lead to imprisonment, fines, and penalties.
What is a major part of Medicare fraud?
Beneficiaries commit fraud when they… Let someone use their Medicare card to get medical care, supplies or equipment. Sell their Medicare number to someone who bills Medicare for services not received. Provide their Medicare number in exchange for money or a free gift.
How long does a Medicaid fraud investigation take?
2 weeks to 3 monthsYou can make $825 a month per person to avoid a Medicaid Fraud investigation. How long does a Medicaid fraud investigation last? Medicaid fraud investigations usually last from 2 weeks to 3 months, but can go on indefinitely depending on the case.
What is the difference between healthcare fraud and abuse?
What is health care fraud and abuse? Fraud is an intentional deception or misrepresentation of fact that can result in unauthorized benefit or payment. Abuse means actions that are improper, inappropriate, outside acceptable standards of professional conduct or medically unnecessary.
Who are the victims of healthcare fraud?
Individual victims of health care fraud are sadly easy to find. These are people who are exploited and subjected to unnecessary or unsafe medical procedures. Or whose medical records are compromised or whose legitimate insurance information is used to submit falsified claims.
What is heat in Medicare?
The DOJ, OIG, and HHS established HEAT to build and strengthen existing programs combatting Medicare fraud while investing new resources and technology to prevent and detect fraud and abuse . HEAT expanded the DOJ-HHS Medicare Fraud Strike Force, which targets emerging or migrating fraud schemes, including fraud by criminals masquerading as health care providers or suppliers.
What is the role of third party payers in healthcare?
The U.S. health care system relies heavily on third-party payers to pay the majority of medical bills on behalf of patients . When the Federal Government covers items or services rendered to Medicare and Medicaid beneficiaries, the Federal fraud and abuse laws apply. Many similar State fraud and abuse laws apply to your provision of care under state-financed programs and to private-pay patients.
What does "knowingly submitting" mean?
Knowingly submitting, or causing to be submitted, false claims or making misrepresentations of fact to obtain a To learn about real-life cases of Federal health care payment for which no entitlement Medicare fraud and abuse and would otherwise existthe consequences for culprits,
What is the OIG?
The OIG protects the integrity of HHS’ programs and the health and welfare of program beneficiaries. The OIG operates through a nationwide network of audits, investigations, inspections, evaluations, and other related functions. The Inspector General is authorized to, among other things, exclude individuals and entities who engage in fraud or abuse from participation in all Federal health care programs, and to impose CMPs for certain violations.
What is the Stark Law?
Section 1395nn, often called the Stark Law, prohibits a physician from referring patients to receive “designated health services” payable by Medicare or Medicaid to an entity with which the physician or a member of the physician’s immediate family has a financial relationship , unless an exception applies.
What is the OIG exclusion statute?
Section 1320a-7, requires the OIG to exclude individuals and entities convicted of any of the following offenses from participation in all Federal health care programs:
Is there a measure of fraud in health care?
Although no precise measure of health care fraud exists, those who exploit Federal health care programs can cost taxpayers billions of dollars while putting beneficiaries’ health and welfare at risk. The impact of these losses and risks magnifies as Medicare continues to serve a growing number of beneficiaries.
What is the number to call for Medicare fraud?
1-800-557-6059 | TTY 711, 24/7. The above scenario is just one example of a recent type of Medicare scam. Let’s take a deeper look at Medicare fraud, including the types of scams to be aware of and how you and your loved ones can stay safe.
What is Medicare scam?
Medicare scams, like the one described above involving Medicare cards, are when individuals pose as health care providers to gather and use a Medicare beneficiary’s personal information to receive health care or money they are not entitled to.
How long is the man in jail for Medicare fraud?
The man faces up to 10 years in prison for each of the six counts of fraud. A former health care executive in Texas admitted to her role in a $60 million Medicare fraud scheme that included overdosing hospice patients in order to maximize profits. She faces up to 10 years in prison.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
Can Medicare call you out of the blue?
In other words, Medicare will never call you out of the blue. This is very important to remember as you look to keep yourself safe from Medicare fraud, scams and abuse.
What are some examples of Medicare abuse?
One example of Medicare abuse is when a doctor makes a mistake on a billing invoice and inadvertently asks for a non-deserved reimbursement. Medicare waste involves the overutilization of services that results in unnecessary costs to Medicare.
What is the False Claims Act?
The False Claims Act protects the government from being sold substandard goods or services or from being overcharged. It holds people accountable who knowingly submit or cause to be submitted a false or fraudulent Medicare claim.
What are some examples of Medicare fraud?
Some of the More Common Examples of Medicare or Medicaid Fraud include the following: Paying “kickbacks” in exchange for referring business. “Kickbacks” are customary in healthcare fraud cases. State and federal laws by and large ban payments to individuals who refer patients to a particular hospital or medical provider.
What is healthcare fraud?
Healthcare fraud is committed when a dishonest provider intentionally submits, or causes someone else to submit, false or misleading information for use in determining the amount of healthcare benefits payable by an insurer. Many leading, medical groups calculate fraud to amount up to 10% of all healthcare costs.
Why did a doctor fabricated his patient's medical records?
He fabricated his patient’s medical records to indicate office visits and treatments that never took place.
How much does Medicare pay out?
Medicare pays out over $800 billion a year for claims. Medicaid also has enormous budget, providing $615 billion a year. Their sheer size makes these goliaths a target for those groups committing fraud. Plus with such volume, the U.S. Government is unable to police fraudulent claims. They rely on whistleblower.
What is itemized medical bill?
Itemized medical bills are long and contain dozens of items the patient may not recognize. It’s tempting to throw an extra procedure onto the bill, while charging Medicare or Medicaid for services not rendered. The longer the bill, the simpler it is to slip in a fraudulent charge.
How much does an appendectomy cost?
Here’s a prime example. A patient has an appendectomy that costs $2400 total.
What is the False Claims Act?
As a prime example, the False Claims Act bars medical practitioners from submitting insurance claims for substandard and overpriced goods and services, identifying individuals who do not report their knowledge of such claims as perpetrating fraud.
How does Medicaid fraud affect the health care system?
Not only do fraudulent and abusive practices increase the cost of Medicaid without adding value – they increase risk and potential harm to patients who are exposed to unnecessary procedures.
What is program integrity?
Program Integrity Initiatives. The federal government and states have adopted a variety of steps to combat Medicaid fraud, waste and abuse and to ensure that public funds are used to promote Medicaid enrollees’ health. According to the Medicaid and CHIP Payment Access Commission ( MACPAC ), these include data mining, audits, investigations, ...
