- Balance billing is when a provider bills you for the rest of the charge after your insurance company has paid their limit.
- Balance billing is also known as surprise billing since it often takes patients by surprise.
- Some states have taken steps to protect patients from balance billing.
What states have balance billing laws?
States with Comprehensive Protection
- California. In July 2017, a new law took effect in California that protects consumers who use in-network hospitals or other health facilities, from being charged with surprise bills after ...
- Connecticut. According to Connecticut’s law No. ...
- Florida. ...
- Illinois. ...
- Maryland. ...
- New Hampshire. ...
- New York. ...
- Oregon. ...
- Virginia. ...
- Other States. ...
What are balance billing charges?
The basics of the new protections follow: What is balance billing? Balance billing occurs when a health care provider bills a patient after the patient’s health insurance company has paid its portion. The balance bill is for
What is a surprise medical bill or balance billing?
“Surprise billing” is an unexpected balance bill. This can happen when you can’t control who is involved in your care—like when you have an emergency or when you schedule a visit at an in-network facility but are unexpectedly treated by an out-of-network provider.
Is balance billing illegal?
In some states, balance billing is actually illegal, meaning you do not have to pay the balance if you visit an in-network provider that takes your insurance and your policy covers the services rendered. Balance billing is legal in some states and not in others.
What does balance billing mean in healthcare?
When a provider bills you for the difference between the provider's charge and the allowed amount. For example, if the provider's charge is $100 and the allowed amount is $70, the provider may bill you for the remaining $30. A preferred provider may not balance bill you for covered services.
How do you fight balance billing?
Steps to Fight Against Balance BillingReview the Bill. Billing departments in hospitals and doctor offices handle countless insurance claims on a daily basis. ... Ask for an Itemized Billing Statement. ... Document Everything. ... Communicate with Care Providers. ... File an Appeal with Insurance Company.
How do you use balance billing?
A balance bill is issued when a provider charges a patient with the amount the insurance company doesn't pay. For example, the dermatologist charges the insurance company $300. The insurance company agreed to pay $150. If the doctor then charges the patient the remaining $150, the patient will receive a balance bill.
Why do doctors charge more than Medicare pays?
Why is this? A: It sounds as though your doctor has stopped participating with Medicare. This means that, while she still accepts patients with Medicare coverage, she no longer is accepting “assignment,” that is, the Medicare-approved amount.
Can doctors charge whatever they want?
They're not actually billing people different amounts because they have insurance or not. Doctors can pretty much bill a patient whatever they want for their service, similar to how a grocery store can charge whatever they want for their fresh deli cheese. Generally, they charge every single person the same amount.
How can I get my medical bills forgiven?
How does medical bill debt forgiveness work? If you owe money to a hospital or healthcare provider, you may qualify for medical bill debt forgiveness. Eligibility is typically based on income, family size, and other factors. Ask about debt forgiveness even if you think your income is too high to qualify.
Can a physician write off a patient balance?
There is no rule of thumb for writing off balances; it is per the practice's discretion. Many practices make the determination based on the patient's ability to pay. A more practical solution may be to set a policy for indigent charity write-offs.
Can a par provider can bill the patient for the difference between their fee and insurance companies allowed amount?
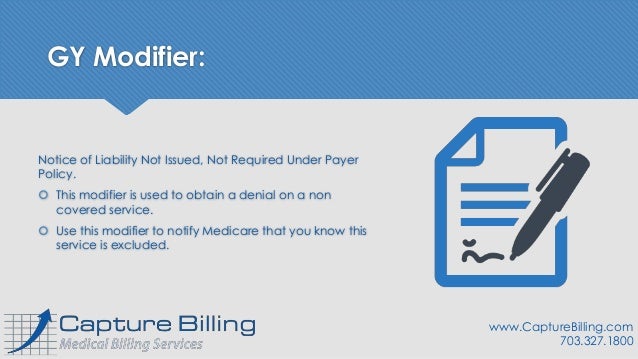
Importantly, as a PAR provider, you cannot bill patients for any amount over the set Medicare allowable fee.
What is no balance billing policy?
The No Balance Billing (NBB) is a policy of the government—implemented through. PhilHealth—which ensures that qualified members shall not be charged or be forced to. spend out-of-pocket for services that had been rendered to them in government hospitals. and selected private hospitals that are PhilHealth-accredited.
Do doctors lose money on Medicare patients?
Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
Do doctors have to accept what Medicare pays?
Can Doctors Refuse Medicare? The short answer is "yes." Thanks to the federal program's low reimbursement rates, stringent rules, and grueling paperwork process, many doctors are refusing to accept Medicare's payment for services. Medicare typically pays doctors only 80% of what private health insurance pays.
Can a doctor charge more than the Medicare-approved amount?
A doctor who does not accept assignment can charge you up to a maximum of 15 percent more than Medicare pays for the service you receive. A doctor who has opted out of Medicare cannot bill Medicare for services you receive and is not bound by Medicare's limitations on charges.
Is Balance Billing Legal Or Not?
Sometimes it’s legal, and sometimes it isn’t; it depends on the circumstances and your state’s insurance laws.Balance billing is generally illegal:...
How Balance Billing Works
When you get care from a doctor, hospital, or other health care provider that isn’t part of your insurer’s provider network (or, if you have Medica...
When Does Balance Billing Happen?
In the United States, balance billing usually happens when you get care from a doctor or hospital that isn’t part of your health insurance company’...
Surprise Balance Billing: Out-Of-Network Providers Working at In-Network Facilities
Receiving care from an out-of-network provider can happen unexpectedly, even when you try to stay in-network. For example, you go to an in-network...
What to Do If You Receive An Unexpected Balance Bill
Receiving a balance bill is a stressful experience, especially if you weren't expecting it. You've already paid your deductible and coinsurance and...
If You Know in Advance You’Ll Be Legally Balance Billed
First, try to prevent balance billing by staying in-network and making sure your insurance company covers the services you’re getting. If you’re ha...
What is balance billing?
In the United States, balance billing usually happens when you get care from a doctor or hospital that isn’t part of your health insurance company’s provider network or doesn’t accept Medicare or Medicaid rates as payment in full.
What happens if a doctor doesn't accept assignment with Medicare?
But if your doctor hasn't opted out but just doesn't accept assignment with Medicare (ie, doesn't accept the amount Medicare pays as payment in full), you could be balance billed up to 15% more than Medicare's allowable charge, in addition to your regular deductible and/or coinsurance payment.
What happens if you pay your deductible?
If You Know in Advance. Prevention. Balance billing happens after you’ve paid your deductible, coinsurance or copayment and your insurance company has also paid everything it’s obligated to pay toward your medical bill. If there is still a balance owed on that bill and the doctor or hospital expects you to pay that balance, ...
What happens if you have a contract with a medicaid provider?
When your doctor or hospital has a contract with your health plan and is billing you more than that contract allows. In each of these cases, the agreement between the healthcare provider and Medicare, Medicaid, or your insurance company includes a clause ...
Is it stressful to receive a balance bill?
Receiving a balance bill is a stressful experience, especially if you weren't expecting it. You've already paid your deductible and coinsurance and then you receive a substantial additional bill—what do you do next?
Can a lab balance bill you?
It can also happen for services received from a provider chosen by someone else, such as when you have a pap smear or a biopsy done in your doctor’s office, or blood drawn by your home health nurse. If your doctor or nurse sends the specimen to an out-of-network lab, that lab can balance bill you.
Is a health insurance plan self funded?
If your health plan is self-funded, meaning your employer is the entity actually paying the medical bills even though an insurance company may administer the plan, then your health plan won't fall under the jurisdiction of your state’s department of insurance.
What is balance billing?
Balance billing occurs when providers bill a patient for the difference between the amount they charge and the amount that the patient’s insurance pays. The amount that insurers pay providers is almost always less than the providers’ “retail price.”. Some providers will bill the patient for the difference, or balance; this is called balance billing.
When will surprise balance billing protections be implemented?
In July 2021, HHS published an interim final rule with details regarding how the surprise balance billing protections will be implemented as of 2022 (more details are available here and here ).
When will surprise balance billing start?
Relief is on the horizon, however, with new federal legislation that will protect consumers from most surprise balance billing starting in 2022.
Can a provider accept a balance bill?
Providers that are in-network have agreed to accept the insurance payment as payment in full (less any applicable copays, deductible, or coinsurance), and are not allowed to balance bill the patient. However, balance billing is allowed if the provider is not in your insurance network (as described below, there are varying state rules ...
Does an out of network provider pay for out of network care?
If the insurer covers out-of-network care, they will pay the provider based on the insurer’s reasonable and customary rates (keeping in mind that the patient will be responsible for the out-of-network deductible and coinsurance, which is typically quite a bit higher than in-network cost-sharing). But at that point, the provider can bill ...
Surprise Billing Explained in Less Than 5 Minutes
Lorraine Roberte is an insurance writer for The Balance. As a personal finance writer, her expertise includes money management and insurance-related topics. She has written hundreds of reviews of insurance products.
Definition and Examples of Balance Billing
What your medical provider charges for a service and the amount your health insurance company will pay for that service can be, and often are, two different numbers. Balance billing is when your provider bills you for the difference. In-network providers are not allowed to do this for covered services.
How Does Balance Billing Work?
Balance billing is when you’re responsible for the remainder of a bill after your insurance company has paid the allowed or approved amount. If you visit a preferred provider, that provider isn’t allowed to balance bill—in-network providers have an agreement with the insurance company to provide services for the agreed-upon amount.
When Is Balance Billing Not Allowed?
To help protect its clients from unexpected medical bills, some insurance companies have banned balance billing. For example, Medicare providers are prohibited from balance billing qualified Medicare patients. 3
What to do if you receive a balance bill from a health care provider?
One of the first things to do if you receive a balance bill from a health care provider is to confirm that the bill is legitimate. Billing departments do make mistakes from time to time, and they could have sent you a statement by mistake.
What is a balance bill?
A balance bill is issued when a provider charges a patient with the amount the insurance company doesn't pay. For example, the dermatologist charges the insurance company $300. The insurance company agreed to pay $150. If the doctor then charges the patient the remaining $150, the patient will receive a balance bill.
Why is a balance bill alarming?
A balance bill can be a cause for alarm, especially when it is for a large amount of money and a patient isn't expecting it. Understanding how balance-billing works and when it is allowed and not allowed will help you know what to do if you ever receive an unexpected bill for medical services.
How to protect employees from balance billing?
One way to protect your employees from the challenges of balance-billing is to make sure you have protections in place should the issue ever come up. With Patient Defender, plan members have legal counsel at their fingertips should they get a surprise or balance bill from a provider.
What is surprise billing?
In some cases, it's called "surprise billing” if the patient had a specific reason to expect that there would be no balance-billing (such as visiting an in-network hospital but unwittingly being treated by an out-of-network anesthesiologist). A balance bill can be a cause for alarm, especially when it is for a large amount ...
Is balance billing the same as deductible?
Balance-billing is not the same thing as charging a patient a deductible, co-insurance or co-pay. The deductible is the amount a patient needs to pay out-of-pocket before a health insurance plan starts to pay for covered services and providers. For example:
Can a hospital send a patient a balance bill?
There are two instances when a hospital or provider is not allowed to send a patient a balance bill. First, some states have passed laws that limit balance-billing or surprise bills. Twenty-five states have laws that partially or fully protect patients from surprise bills.
What is balance billing?
Balance billing occurs when you receive care at an in network facility, but the provider treating you is out of network on your health plan. Your insurance will cover the in network facility charges. The out of network provider will send you a bill outside of your insurance plan for what they want to get paid.
How to fight a balance bill?
You can fight a balance bill by submitting 1 or 2 internal appeals with your insurance company. During the appeals process, insurance companies will review the situation to determine if they can pay the doctor more money to offset or negate the balance bill. Ultimately, the doctor decides whether or not to play ball and rescind the balance bill.