
Who is eligible for chronic care management?
recognizes Chronic Care Management (CCM) as a critical component of primary care that contributes to better health and care for individuals. In 2015, Medicare began paying separately under the Medicare Physician Fee Schedule (PFS) for CCM services furnished to Medicare patients with multiple chronic conditions.
What do you need to know about chronic care management?
Jan 19, 2022 · Chronic Care Management is defined as the non-face-to-face services provided to Medicare beneficiaries who have multiple , significant chronic conditions that place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline.
What are the requirements for chronic care management?
Medicare Chronic Care Management is for Medicare-eligible people with two or more serious chronic conditions. Chronic Care Management plans are paid for by Medicare Part B. Medicare Advantage (Part C) plans also cover the cost of CCMs. All the medical services you need for your conditions, including prescriptions and appointments, are overseen by one healthcare provider.
How to Bill CCM services?
Oct 26, 2021 · Chronic Care Management is an effective program developed to improve care coordination for the millions of Medicare beneficiaries with chronic medical conditions. It improves access to care, increases patient satisfaction, and decreases long-term medical complications. A Word From Verywell
What does chronic care management include?
Chronic care management includes any care provided by medical professionals to patients who have chronic diseases and conditions. A disease or condition is chronic when it lasts a year or more, requires ongoing medical attention or limits the activities of daily life.
How Much Does Medicare pay for CCM?
CCM is covered under Medicare Part B. This means that Medicare will pay 80 percent of the cost of service. You'll be responsible for a coinsurance payment of 20 percent.Apr 7, 2020
How do you explain CCM to patients?
CCM is the care coordination that is outside of the regular office visit for patients with multiple (two or more) chronic conditions expected to last at least 12 months or until the death of the patient, and that place the patient at significant risk of death, acute exacerbation or decompensation, or functional decline ...
Is CCM only for Medicare?
Chronic care management (CCM) services are generally non-face-to-face services provided to Medicare beneficiaries who have multiple (two or more) chronic conditions expected to last at least 12 months, or until the death of the patient.
Does chronic care management save money?
The effectiveness of the CCM program saves Medicare approximately $74 per patient, per month. Removing the patient cost burden would positively affect 72%4 of the Medicare population living with chronic conditions, and could save medicare nearly $3,700,000,000 per year in costs.Jul 15, 2019
How often can chronic care management be billed?
once per monthA claim for CCM, using code 99490, may be submitted to Medicare once per month when the requirements of the service are met.
What is the purpose of CCM?
The purpose of Medicare's Chronic Care Management program is to help patients with chronic conditions better manage their self-care and optimize their health. The primary goals of CCM are to assist patients with: accessing needed health services. coordinating care.
Why is CCM important?
Chronic care management is one of the best ways to ensure that patients who are battling chronic conditions have a better quality of life. Studies show that CCM services decrease depression, increase social activity, and promote patient engagement for these individuals.Aug 22, 2018
What are the benefits of CCM?
In adults, it effectively promotes the consolidation and maintenance of bone mass. In conjunction with vitamin D, CCM also decreases bone fracture risk in the elderly, slows the rate of bone loss in old age, and is of benefit to the health and well-being of postmenopausal women.
How do you introduce chronic care management to patients?
Offering Chronic Care Management to Patients Explain the Benefits. ... Get Your Staff on Board. ... Progress Reports. ... Prescription Refills and Discounts. ... Engage Community Resources.May 18, 2020
What is considered a chronic condition?
A disease or condition that usually lasts for 3 months or longer and may get worse over time. Chronic diseases tend to occur in older adults and can usually be controlled but not cured. The most common types of chronic disease are cancer, heart disease, stroke, diabetes, and arthritis.
What is a serious chronic medical condition?
Chronic diseases are defined broadly as conditions that last 1 year or more and require ongoing medical attention or limit activities of daily living or both. Chronic diseases such as heart disease, cancer, and diabetes are the leading causes of death and disability in the United States.
What Is Medicare Chronic Care Management?
Medicare Chronic Care Management (CCM) is a comprehensive care plan you sign up for through a Medicare-approved healthcare provider. These provider...
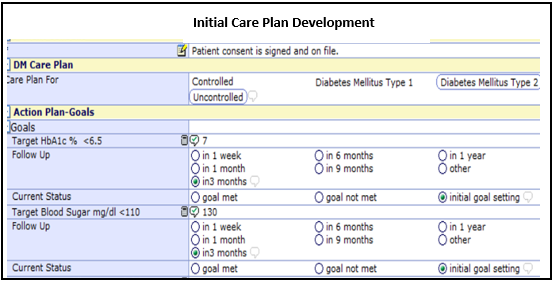
What is a CCM care plan?
CCM care plans provide chronic care management services that are personally overseen by a doctor or other qualified healthcare professional. CCM ca...
Does Medicare Cover Chronic Care Management?
Medicare Part B covers 80% of the cost of Chronic Care Management, provided it is administered by a Medicare-approved healthcare professional.
What conditions qualify for chronic care management?
Many severe conditions make you eligible for chronic care management. You must have two or more conditions that will last for one year or longer.
What Does Medicare Pay for Chronic Care Management?
If your healthcare provider takes Medicare assignment, Medicare will pay 80% of the Medicare-approved cost for all the services and supplies you ge...
How Do You Apply for Chronic Care Management?
Talk to your current medical provider about getting a CCM. If they don’t offer this service, they may recommend you to a physician who does.
What Does A Chronic Care Manager Do?
Your chronic care manager’s goal is to make sure you receive optimum medical support for every chronic condition you are diagnosed with.
What is CCM in healthcare?
The Centers for Medicare & Medicaid Services (CMS) recognizes Chronic Care Management (CCM) as a critical component of primary care that contributes to better health and care for individuals. CCM allows healthcare professionals to be reimbursed for the time and resources used to manage Medicare patients’ health between face-to-face appointments.
What is a CCM?
CCM requires that patients have 24/7 access to physicians or other qualified healthcare professionals or clinical staff to address urgent needs. In addition to physician offices, CCM services can be provided by Federally Qualified Health Centers (FQHCs), Rural Health Clinics (RHCs), and Critical Access Hospitals (CAHs).
How long does chronic care management last?
These conditions must be expected to last at least 12 months or until the death of the patient. Also, if you’re eligible, you should take advantage ...
Why is chronic care important?
Chronic care management is critical to those with severe health conditions. It can help patients continuously manage these conditions, potentially reducing pain, and increasing relaxation, mobility, and even lifespan.
What are management services?
Management services can include: 1 Creating a plan of care with your doctor 2 At least 20 minutes of care management health services per month 3 Frequent check-ins with your doctor 4 Emergency access to health care providers
Who is Lindsay Malzone?
https://www.medicarefaq.com/. Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
Does Medicare cover medical expenses?
Thankfully, Medigap plans can help with these extra costs. While Medicare covers many of your medical needs, it doesn't cover every cost you'll face. When you enroll in a Medigap plan, you can get help with copays, deductibles, and coinsurance.
