Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
Full Answer
What is the timely filing period for Medicare fee for service claims?
define the timely filing period for Medicare fee for service claims. In general, such claims must be filed to the appropriate Medicare claims processing contractor no later than 12 months, or 1 calendar year, after the date the services were furnished. (See section §70.7 below for details of the exceptions to the 12 month timely filing limit.)
When do I need to file a Medicare claim?
When do I need to file a claim? Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
What is the receipt date of a claim?
A3-3600.1-Item 7 The receipt date of a claim is the date the contractor receives the claim (provided the filing is in a format and contains data sufficiently complete so that the filing qualifies as a claim).
When does my Medicare coverage start?
Medicare coverage starts based on when you sign up and which sign-up period you’re in. Generally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
What is the Medicare time limit to submit the claims?
12 monthsPolicy: The time limit for filing all Medicare fee-for-service claims (Part A and Part B claims) is 12 months, or 1 calendar year from the date services were furnished.
What date does Medicare consider date of service?
The date of service for the Certification is the date the physician completes and signs the plan of care. The date of the Recertification is the date the physician completes the review. For more information, see the Medicare Claims Processing Manual, Chapter 12, Section 180.1.
How do claims work with Medicare?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
What is a date of service?
Date of Service means the date on which the client receives medical services or items, unless otherwise specified in the appropriate provider rules.
What does date of service mean insurance?
What Does Date of Service Mean? The date of service is the specific time at which a patient has been given medical treatment. It is recorded for billing purposes and as an item in a patient's medical record.
What is retroactive Medicare entitlement?
(3) Retroactive Medicare entitlement involving State Medicaid Agencies, where a State Medicaid Agency recoups payment from a provider or supplier 6 months or more after the date the service was furnished to a dually eligible beneficiary.
Can I submit claims directly to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
Why is Medicare not paying on claims?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
How does Medicare crossover claims work?
1. What is meant by the crossover payment? When Medicaid providers submit claims to Medicare for Medicare/Medicaid beneficiaries, Medicare will pay the claim, apply a deductible/coinsurance or co-pay amount and then automatically forward the claim to Medicaid.
What does date of service for this requested mean?
Related Definitions Requested Service Date means the date requested by Customer for the commencement of Service.
What is the 26 modifier?
Modifier 26 is defined as the professional component (PC). The PC is outlined as a physician's service, which may include technician supervision, interpretation of results and a written report. Use modifier 26 when a physician interprets but does not perform the test.
What is place of service in medical billing?
Place of service (POS) codes are crucial for correctly preparing the claims. As evident from its name, the place of service code denotes the place at which the provider has rendered the medical services to the patient. The POS code should be coupled with the correct treatment or procedural code.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
How do I file a claim?
Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
What is an itemized bill?
The itemized bill from your doctor, supplier, or other health care provider. A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare.
What happens after you pay a deductible?
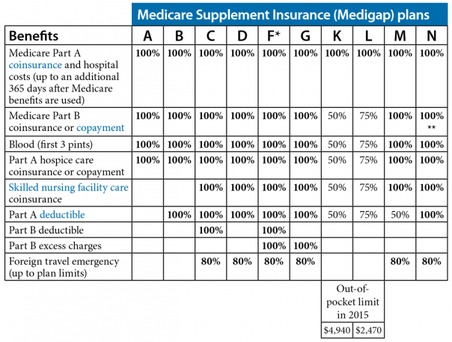
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). , the law requires doctors and suppliers to file Medicare. claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered.
What is Medicare 40.3?
40.3 - Readmission to Medicare Program After Involuntary Termination
What is 10.4 in Medicare?
10.4 - Claims Submitted for Items or Services Furnished to Medicare Beneficiaries in State or Local Custody Under a Penal Authority
What is a 50.1.1 form?
50.1.1 - Billing Form as Request for Payment
What is 30.3.7 billing?
30.3.7 - Billing for Diagnostic Tests (Other Than Clinical Diagnostic
What is 30.1?
30.1 - Content and Terms of Provider Participation Agreements
What do providers need to determine regarding the date of service?
Providers need to determine the Medicare rules and regulations concerning the date of service and submit claims appropriately . Be sure your billing and coding staffs are aware of this information.
What is the date of service for a physician certification?
The date of service for the Certification is the date the physician completes and signs the plan of care. The date of the Recertification is the date the physician completes the review.
What is the date of service for clinical laboratory services?
Generally, the date of service for clinical laboratory services is the date the specimen was collected. If the specimen is collected over a period that spans two calendar dates, the date of service is the date the collection ended. There are three exceptions to the general date of service rule for clinical laboratory tests:
What is the date of service for ESRD?
The date of service for a patient beginning dialysis is the date of their first dialysis through the last date of the calendar month. For continuing patients, the date of service is the first through the last date of the calendar month. For transient patients or less than a full month service, these can be billed on a per diem basis. The date of service is the date of responsibility for the patient by the billing physician. This would also include when a patient’s dies during the calendar month. When submitting a date of service span for the monthly capitation procedure codes, the day/units should be coded as “1”.
What is a CPO in Medicare?
CPO is physician supervision of a patient receiving complex and/or multidisciplinary care as part of Medicare covered services provided by a participating home health agency or Medicare approved hospice. Providers must provide physician supervision of a patient involving 30 or more minutes of the physician's time per month to report CPO services. The claim for CPO must not include any other services and is only billed after the end of the month in which CPO was provided. The date of service submitted on the claim can be the last date of the month or the date in which at least 30 minutes of time is completed.
What is a radiology PC/TC indicator?
These services will have a PC/TC indicator of “1” on the Medicare Physician Fee Schedule (MPFS) Relative Value File. The technical component is billed on the date the patient had the test performed. When billing a global service, the provider can submit the professional component with a date of service reflecting when the review and interpretation is completed or can submit the date of service as the date the technical component was performed. This will allow ease of processing for both Medicare and the supplemental payers. If the provider did not perform a global service and instead performed only one component, the date of service for the technical component would the date the patient received the service and the date of service for the professional component would be the date the review and interpretation is completed.
What is noncompliance in Medicare?
Noncompliance will be considered in determining whether the provider is honoring its agreement, under which it may not charge for services for which payment may be made under the Medicare program.
What is M+CO in Medicare?
The provider must ascertain whether the patient is a member of a Medicare + Choice organization (M+CO). If the patient is a member of an M+CO, the provider must contact the M+CO specified by the patient or identified on the patient’s membership card, so the provider may determine whether to submit the claim to the M+CO.
What is a diagnostic service?
A service is “diagnostic” if it is an examination or procedure to which the patient is subjected, or which is performed on materials derived from a hospital outpatient to obtain information to aid in the assessment of a medical condition or the identification of a disease. Among these examinations and tests are diagnostic laboratory services such as hematology and chemistry, diagnostic x-rays, isotope studies, EKGs, pulmonary function tests, psychological tests, and other tests given to determine the nature and severity of an ailment or injury. Hospitals may determine whether services are diagnostic from their internal systems as appropriate.
What is a DME MAC?
The A/B MAC (A), (B), or (HHH), or DME MAC directs initial requests for assistance to the SSO if the problem is caused by difficulties in determining the beneficiary’s correct entitlement status. Examples of situations that may require SSO assistance are:
Can a provider collect a deductible?
The provider may collect deductible or coinsurance amounts only where it appears that the patient will owe deductible or coinsurance amounts and where it is routine and customary policy to request similar prepayment from non-Medicare patients with similar benefits that leave patients responsible for a part of the cost of their hospital services. In admitting or registering patients, the provider must ascertain whether beneficiaries have medical insurance coverage. Where beneficiaries have medical insurance coverage, the provider asks the beneficiary if he/she has a Medicare Summary Notice (MSN) showing his/her deductible status. If a beneficiary shows that the Part B deductible is met, the provider will not request or require prepayment of the deductible.
When are electronic claims received?
Electronic claims transmitted directly to a contractor, or to a clearinghouse with which the contractor contracts as its representative for the receipt of its claims, by 5:00 p.m. in the contractor’s time zone, or by its closing time if it routinely closes between 4:00 p.m. and 5:00 p.m., must likewise be considered as received on that day even if the contractor does not upload or process the data until a later date. NOTE: The differentiation between HIPAA-compliant and HIPAA-non-compliant electronic claims that is specified in §80.2.1.2 with respect to applying the payment floor, does not apply to establishing date of receipt. Use the methodology described above to establish the date of receipt for all electronic claims.
How is a paper claim considered received?
A paper claim is considered as received if it is delivered to the contractor’s place of business by the U.S. Postal Service, picked up from a P.O. box, or is otherwise delivered to the contractor’s place of business by its routine close of business time. If the contractor uses a P.O. box for receipt of mailed claims, it must have its mail picked up from its box at least once per business day unless precluded on a particular day by the emergency closing of its place of business or that of its postal box site.
What is the cutoff time for establishing receipts?
Unless a contractor closes its place of business early in an isolated situation due to an emergency, the contractor’s cutoff time for establishing the receipt date may never be earlier than 4:00 p.m.
What is considered a rejected claim?
Paper and electronic claims that do not meet the basic legibility, format, or completion requirements are not considered as received for claims processing and may be rejected from the claims processing system. Rejected claims are not considered as received until
Do electronic claims have to be delivered manually?
As electronic claim tapes and diskettes that may be submitted by providers or their agents to an FI are also subject to manual delivery, rather than direct electronic transmission, the paper claim receipt rule also applies to establish the date of receipt of claims submitted on such manually delivered tapes and diskettes.
When Do I Need to File A Claim?
- You should only need to file a claim in very rare cases
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicar… - If your claims aren't being filed in a timely way:
1. Contact your doctor or supplier, and ask them to file a claim. 2. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and yo…
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…