Claims Processing Manual This manual contains billing requirements, rules, and regulations as they pertain to Medicare in all settings. This manual provides information on completing the CMS-1500 claim form used by physical and occupational therapists in private practice.
Full Answer
How do I make a Medicare claim?
Claim Medicare benefits at your doctor’s office. The quickest and easiest way to claim is at your doctor’s office straight after you pay. To do this you need to both: be enrolled in Medicare. show your Medicare card. If your doctor bulk bills, you don’t need to pay. When you pay at the doctor’s office, ask if they can make an electronic ...
How to process Medicare claims?
The verification process to discover what is your primary Medicare insurance is below:
- Visit https://www.mymedicare.gov/ and register for a MyMedicare.gov account.
- View what is in your MyMedicare.gov account and verify that your Medicare information is correct. ...
- If you see that your employer group health plan is still primary after you have enrolled in you and/or your spouse’s Medicare Part B, then Medicare is requesting that one ...
How to code and process Medicaid claims?
Medicare coding criteria. Medicare strictly adheres to the established National Correct Coding Initiative (NCCI) edits, along with procedure/medical necessity protocol. In addition, its claims processing system is highly refined. Any claim that is submitted with errors or without the correct information does not process, period.
What to do if Medicare denies your medical claim?
You can also take other actions to help you accomplish this:
- Reread your plan rules to ensure you are properly following them.
- Gather as much support as you can from providers or other key medical personnel to back up your claim.
- Fill out each form as carefully and exactly as possible. If necessary, ask another person to help you with your claim.

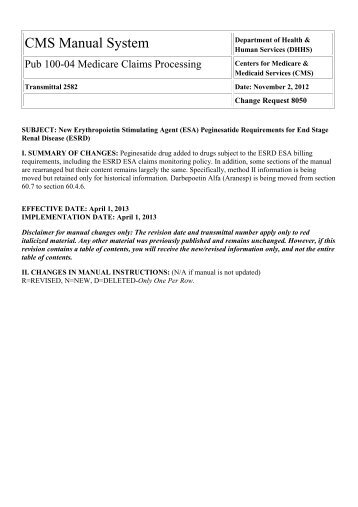
What is a CMS manual?
The CMS Online Manual System is used by CMS program components, partners, contractors, and State Survey Agencies to administer CMS programs. It offers day-to-day operating instructions, policies, and procedures based on statutes and regulations, guidelines, models, and directives.
How are Medicare claims processed?
Your provider sends your claim to Medicare and your insurer. Medicare is primary payer and sends payment directly to the provider. The insurer is secondary payer and pays what they owe directly to the provider. Then the insurer sends you an Explanation of Benefits (EOB) saying what you owe, if anything.
What is the first step in submitting Medicare claim?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
What document notifies Medicare beneficiaries of claims processing?
The MSN is used to notify Medicare beneficiaries of action taken on their processed claims. The MSN provides the beneficiary with a record of services received and the status of any deductibles.
How are claims processed?
How Does Claims Processing Work? After your visit, either your doctor sends a bill to your insurance company for any charges you didn't pay at the visit or you submit a claim for the services you received. A claims processor will check it for completeness, accuracy and whether the service is covered under your plan.
What are Medicare claims?
A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare. It explains what the doctor, other health care provider, or supplier billed for, the Medicare-approved amount, how much Medicare paid, and what you must pay.
Who files Medicare claims?
Overview. Your Medicare Part A and B claims are submitted directly to Medicare by your providers (doctors, hospitals, labs, suppliers, etc.). Medicare takes approximately 30 days to process each claim.
Can I submit claims directly to Medicare?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
How do I do Medicare billing?
For specific Medicare billing questions: Call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. For questions about your Part A or Part B coverage: Call Social Security at 1-800-772-1213. TTY: 1-800-325-0778.
What must a provider do to receive payment from Medicare?
Taking assignment means that the provider accepts Medicare's approved amount for health care services as full payment. These providers are required to submit a bill (file a claim) to Medicare for care you receive. Medicare will process the bill and pay your provider directly for your care.
How long does it take for Medicare to pay claims?
For clean claims that are submitted electronically, they are generally paid within 14 calendar days by Medicare. The processing time for clean paper claims is a bit longer, usually around 30 days.
How many days does Medicare have to pay a claim?
Effective immediately, any Medicare Fee-For-Service claim with a date of service on or after January 1, 2010, must be received by your Medicare contractor no later than one calendar year (12 months) — or Medicare will deny the claim. Yes, one calendar year.
Medicare Claims Processing Manual
Coding and Billing Information | CMS
Billing and Coding Guidelines - CMS
Condition Codes - JE Part A - Noridian
What is the overarching adjustment claim logic?
“Overarching adjustment claim logic” is defined as the logic that CWF will employ, independent of a specific review of claim monetary changes, when a COBA trading partner’s COIF specifies that it wishes to exclude all adjustment claims.
When did the CWF change its systematic logic?
Effective with April 1, 2008, the CWF maintainer shall change its systematic logic to accept a new version of the COIF that now features a new “all adjustment claims” exclusion option.
What happens if a claim is incomplete?
If a claim is submitted with incomplete or invalid information, it may be returned to the submitter as unprocessable. See Chapter 1 for definitions and instructions concerning the handling of incomplete or invalid claims.
Can a physician choose a primary specialty code?
Physicians are allowed to choose a primary and a secondary specialty code. If the A/B MAC (B) and DME MAC provider file can accommodate only one specialty code, the A/B MAC (B) or DME MAC assigns the code that corresponds to the greater amount of allowed charges. For example, if the practice is 50 percent ophthalmology and 50 percent otolaryngology, the A/B MAC (B)/DME MAC compares the total allowed charges for the previous year for ophthalmology and otolaryngology services. They assign the code that corresponds to the greater amount of the allowed charges.
What is a consolidated billing for SNF?
Effective January 1, 2005, section 410 of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) amended the SNF consolidated billing law to specify that when a SNF’s Part A resident receives the services of a physician (or another type of practitioner that the law identifies as being excluded from SNF consolidated billing) from a RHC or a FQHC, those services are not subject to CB merely by virtue of being furnished under the auspices of the RHC or FQHC. Accordingly, under section 410 of the MMA, services otherwise included within the scope of RHC and FQHC services that are also described in clause (ii) of section 1888(e)(2)(A) are excluded from consolidated billing, effective with services furnished on or after January 1, 2005. Only this subset of RHC/FQHC services may be covered and paid separately when furnished to SNF residents during a covered Part A stay (see the regulations at 42 CFR 411.15(p)(2)(xvii) and 405.2411(b)(2)). Use TOBs 71x and 73x, respectively, to bill for these RHC/FQHC services. See Pub. 100-02, Medicare Benefit Policy Manual, chapter 13 for additional information on Part B coverage of RHC/FQHC services.
What is the revenue code for SNF?
The SNF Pricer shall calculate the rate for each line item with revenue code 0022 on a SNF claim. The SNF Pricer shall determine the rate using the following information:
How long does a beneficiary have to transfer to a second SNF?
It is certainly possible that a beneficiary may remain at a facility under sanction for a period of time and later transfer to a second SNF. The 30-day transfer requirement will be applied in the same way it would be for a beneficiary transferring between two SNFs that are not under sanction. Part A coverage will be available to the second SNF for all remaining days in the benefit period as long as the beneficiary:
When did CWF implement the unsolicited response edit?
Effective July 1, 2002 , CWF implemented the unsolicited response edit based on the same coding files made available for the reject edits. Upon receipt of a Part A SNF claim at CWF, CWF searches paid claims history and compares the period between the SNF from and through dates to the line item service dates of the claims in history. It then identifies any services within the dates of the SNF stay that should have been subject to consolidated billing and should not have been separately paid by the A/B MAC (B)/DME
Does Medicare coordinate care require consolidated billing?
Services for beneficiaries covered under the Medicare Coordinated Care Demonstration will not be subject to consolidated billing. Common Working File (CWF) will appropriately edit for these codes so that the A/B MACs (B) will pay them separately.
Can a provider furnish a covered item?
provider may have others furnish certain covered items and services to their patients through arrangements under which receipt of payment by the provider for the services discharges the liability of the beneficiary or any other person to pay for the service. In permitting providers to furnish services under arrangements, it is not intended that the provider merely serve as a billing mechanism for the other party. Accordingly, for services provided under arrangements to be covered, the provider must exercise professional responsibility over the arranged-for services. See the Medicare General Information, Eligibility, and Entitlement Manual, Chapter 5, “Definitions,” §10.3, for additional discussion on services furnished under arrangement.
