Medicare conditions of participation are federal regulations with which particular health-care facilities must comply in order to receive funding from the Medicare and Medicaid programs.
Full Answer
What is Medicare?
Medicare is the federal health insurance program for: 1 People who are 65 or older 2 Certain younger people with disabilities 3 People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is a condition code on a Medicare bill?
Condition code only applicable on a xx8 type of bill. Use when canceling a claim for reasons other than the Medicare ID or provider number. Use when canceling a claim to repay a payment. Condition code only applicable to a xx8 type of bill.
What are the conditions of participation for Medicare?
On this basis, the Conditions of Participation, a set of regulations setting minimum health and safety standards for hospitals participating in Medicare, were promulgated in 1966 and substantially revised in 1986.
What are chronic conditions under Medicare Advantage?
“The chronic conditions we are defining today are specific to Medicare special needs plans and are being put into place to ensure that SNPs remain targeted to a specific population, and do not expand their services to mirror more generalized Medicare Advantage plans,” said Weems.
What is a Medicare condition code?
Basic of Medicare Condition Codes Condition codes refer to specific form locators in the UB-04 form that demand to describe the conditions applicable to the billing period. It is important to note that condition codes are situational. These codes should be entered in an alphanumeric sequence.
Under what conditions can a Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
Is condition 44 only for Medicare?
Hospitals use condition code 44 and condition code W2 to bill for Medicare Part B payment in cases where the attending physician orders an inpatient stay that does not meet Medicare's requirements for Part A payment. In such cases, Medicare will deny payment for inpatient admissions.
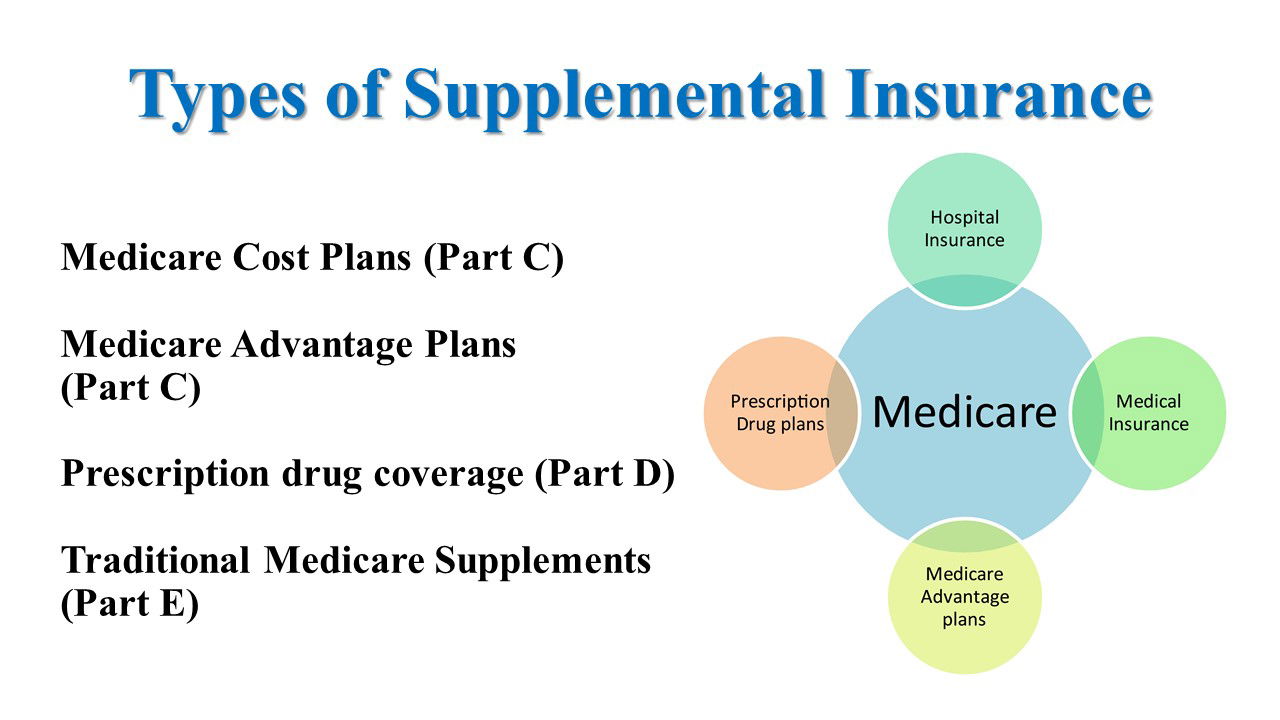
What are the three types of Medicare?
The different parts of Medicare help cover specific services:Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.Medicare Part B (Medical Insurance) ... Medicare Part D (prescription drug coverage)
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Does Medicare have pre existing conditions?
Medicare defines a pre-existing condition as any health problem that you had prior to the coverage start date for a new insurance plan. If you have Original Medicare or a Medicare Advantage plan, you are generally covered for all Medicare benefits even if you have a pre-existing condition.
What does condition code 45 mean?
Ambiguous Gender CategoryPolicy: For Part A claims processing, institutional providers shall report condition code 45 (Ambiguous Gender Category) on any outpatient claim related to transgender or hermaphrodite issues.
What does CC 44 mean?
Condition Code 44--Inpatient admission changed to outpatient – For use on outpatient claims only, when the physician ordered inpatient services, but upon internal review performed before the claim was initially submitted, the hospital determined the services did not meet its inpatient criteria.
What does condition code 44 mean?
A Condition Code 44 is a billing code used when it is determined that a traditional Medicare patient does not meet medical necessity for an inpatient admission.
What part of Medicare is free?
Part APart A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A." Most people get premium-free Part A.
What are the two types of Medicare plans?
There are 2 main ways to get Medicare: Original Medicare includes Medicare Part A (Hospital Insurance) and Part B (Medical Insurance). If you want drug coverage, you can join a separate Medicare drug plan (Part D). as “Part C”) is an “all in one” alternative to Original Medicare.
Is Medicare and Medicaid the same?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What is a Medicare notice?
A notice you get after the doctor, other health care provider, or supplier files a claim for Part A or Part B services in Original Medicare. It explains what the doctor, other health care provider, or supplier billed for, the Medicare-approved amount, how much Medicare paid, and what you must pay.
What is Medicare approved amount?
Medicare-approved amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
What is a select medicaid?
Medicare SELECT. A type of Medigap policy that may require you to use hospitals and, in some cases, doctors within its network to be eligible for full benefits.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What are the different types of Medicare Advantage Plans?
A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: 1 Health Maintenance Organizations 2 Preferred Provider Organizations 3 Private Fee-for-Service Plans 4 Special Needs Plans 5 Medicare Medical Savings Account Plans
What is a certified provider?
Providers are approved or "certified" by Medicare if they've passed an inspection conducted by a state government agency. Medicare only covers care given by providers who are certified.
What is PFFS in Medicare?
Medicare Private Fee-For-Service (PFFS) Plan [Glossary] A type of Medicare Advantage Plan (Part C) in which you can generally go to any doctor or hospital you could go to if you had Original Medicare, if the doctor or hospital agrees to treat you.
What is a CPL for Medicare?
A CPL provides information on items or services that Medicare paid conditionally and the BCRC has identified as being related to the pending claim. For cases where Medicare is pursuing recovery from the beneficiary, a CPL is automatically sent to the beneficiary within 65 days of issuance of the Rights and Responsibilities letter (a copy of the Rights and Responsibilities letter can be obtained by clicking the Medicare's Recovery Process link). All entities that have a verified Proof of Representation or Consent to Release authorization on file with the BCRC for the case will receive a copy of the CPL. Please refer to the Proof of Representation and Consent to Release page for more information on these topics. The CPL includes a Payment Summary Form that lists all items or services the BCRC has identified as being related to the pending claim. The letter includes the interim total conditional payment amount and explains how to dispute any unrelated claims. The total conditional payment amount is considered interim as Medicare might make additional payments while the beneficiary’s claim is pending.
What does BCRC do with conditional payment?
The BCRC will adjust the conditional payment amount to account for any claims it agrees are not related to what has been claimed or released. Upon completion of its dispute review process, the BCRC will notify all authorized parties of the resolution of the dispute.
Does Medicare require a copy of recovery correspondence?
The beneficiary does not need to take any action on this correspondence.
Can you get Medicare demand amount prior to settlement?
If the beneficiary is settling a liability case, he or she may be eligible to obtain Medicare's demand amount prior to settlement or to pay Medicare a flat percentage of the total settlement. Click the Demand Calculation Options link to determine if the beneficiary's case meets the required guidelines.
Does Medicare pay for a secondary plan?
Under Medicare Secondary Payer law (42 U.S.C. § 1395y (b)), Medicare does not pay for items or services to the extent that payment has been, or may reasonably be expected to be, made through a no -fault or liability insurer or through a workers' compensation entity. Medicare may make a conditional payment when there is evidence that the primary plan does not pay promptly conditioned upon reimbursement when the primary plan does pay. The Benefits Coordination & Recovery Center (BCRC) is responsible for recovering conditional payments when there is a settlement, judgment, award, or other payment made to the Medicare beneficiary. When the BCRC has information concerning a potential recovery situation, it will identify the affected claims and begin recovery activities. Beneficiaries and their attorney (s) should recognize the obligation to reimburse Medicare during any settlement negotiations.
How are Medicare Advantage plans paid?
As a result of using HCCs, Medicare Advantage plans are paid using a risk-adjusted payment model that reimburses Medicare Advantage plans based on the actual costs of care for each individual beneficiary rather than an average per-capita payment for everyone.
What is HCC in medical terms?
Hierarchical condition categories (HCC) are designated groups of diagnoses that directly impact how much it may cost an insurance plan provider to pay for your covered care . From your Medicare plan carrier’s perspective, not all of your diagnoses increase your overall health risk and expected care costs.