Depression screenings. Medicare Part B covers an annual depression screening. You do not need to show signs or symptoms of depression to qualify for screening. However, the screening must take place in a primary care setting, like a doctor’s office. This means Medicare will not cover your screening if it takes place in an emergency room,...
What are the USPSTF recommendations for depression screening?
The USPSTF recommends screening for major depressive disorder (MDD) in adolescents aged 12 to 18 years. Screening should be implemented with adequate systems in place to ensure accurate diagnosis, effective treatment, and appropriate follow-up.
Should depression screenings be a part of primary care?
Despite high prevalence rates of depression in primary care, depressive symptoms are often undetected by physicians. Screening for depression is now recommended as a part of routine primary care; however, recent estimates of rates and patterns of depression screening are lacking in the literature.
How does depression screening work?
Depression screenings are often used as a first step in determining whether a physician should inquire more about an individual’s mental health. A patient may be given the screening to complete before seeing the physician or the physician may ask the questions during an exam.
How often are Medicare preventive screenings covered?
Medicare provides it’s members with preventive and screening services coverage, although some are covered annually, while others occasionally or even one-time. Below is a list of the covered preventive services and how often they are covered. Abdominal aortic aneurysm screening – Covered by Part B. A one-time abdominal aortic aneurysm ultrasound.
What is the Medicare patient's responsibility for one depression screening a year?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers one depression screening per year.
What questions do they ask when testing for depression?
“These various screens may include questions about motivation, fatigue, sleep patterns, suicidality, or hopelessness. They may also ask about frequency and duration,” adds Shadick. “In most cases, a depression symptom must be present most days of the week for at least two weeks to be significant."
What screening tool is used for depression?
The Beck Depression Inventory (BDI) is widely used to screen for depression and to measure behavioral manifestations and severity of depression. The BDI can be used for ages 13 to 80.
Can a depression screening be done over the phone?
Mobile phone apps can effectively screen mental health conditions, including depression. However, it is not known how effective such screening methods are in motivating users to discuss the obtained results of such apps with health care professionals.
How long does a depression screening take?
This usually takes less than five minutes. If you are being tested by a mental health provider, he or she may ask you more detailed questions about your feelings and behaviors. You may also be asked to fill out a questionnaire about these issues.
How do doctors know if u have depression?
What Does the Doctor Look for to Make a Depression Diagnosis? A doctor can rule out other conditions that may cause depression with a physical examination, a personal interview, and lab tests. The doctor will also do a complete diagnostic evaluation, discussing any family history of depression or other mental illness.
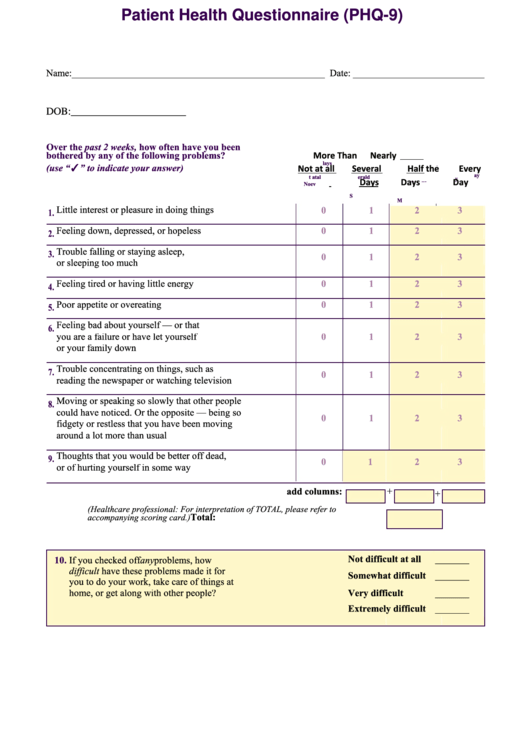
What is a normal depression score?
0 to 4 points:No depression5 to 9 points:Mild depression10 to 14 points:Moderate depression15 to 19 points:Moderately severe depression20 to 27 points:Severe depression
What is the most commonly used measure of depression?
The Hamilton Depression Rating Scale is the most widely used interview scale, developed in 1960 to measure severity of depression in an inpatient population.
What is a positive PHQ score?
The PHQ-9 has 9 questions with a score ranging from 0 to 3 for each question (maximum score of 27). A threshold score of 10 or higher is considered to indicate mild major depression, 15 or higher indicates moderate major depression, and 20 or higher severe major depression.
What does a positive depression screening mean?
What does a positive screen mean? This woman is suffering from many of the symptoms of depression. It does NOT mean she has depression. Only a mental health professional or primary care provider can determine a diagnosis of depression. There is a 25 to 40% chance that she will be diagnosed with depression.
What does a depression score of 13 mean?
5-9: This is considered mild depression. In response to this result, healthcare providers can use their clinical judgment about treatment based on the duration and severity of symptoms. 10-14: This is considered moderate depression.
What does a depression score of 15 mean?
Scoring between 5-9 points indicates mild depression, 10-14 points indicates moderate depression, 15-19 points indicates moderately severe depression, and 20 or more points indicates severe depression. The higher your score, the more symptoms of depression you experience, and the more severe your depression is.
What is depression screening?
Depression screenings should be conducted by your primary care provider (PCP) or another trusted doctor to ensure that you are correctly diagnosed and treated.
Can you screen for depression during a Medicare visit?
However, your provider can choose to screen you during a separate visit. Note: Your provider is required to review your potential for depression and other mental health conditions during your Welcome to Medicare Visit and your first Annual Wellness Visit.
Does Medicare cover depression screening?
Medicare Part B covers an annual depression screening. You do not need to show signs or symptoms of depression to qualify for screening. However, the screening must take place in a primary care setting, like a doctor’s office.
Due to a variety of life changes, adults over the age of 65 are at high risk for depression
Depression is one of the most common mental health disorders in the U.S. While experiences can vary, it's estimated that more than 19 million adults in the U.S. had at least one major depressive episode, and more than 11% of adults aged 18 and older have regular feelings of worry, nervousness, or anxiety.
How often does Medicare cover a depression screening?
Medicare Part B covers one depression screening per year. If your doctor accepts assignment, you pay $0 for this screening and the Part B deductible does not apply. You do not have to show signs or symptoms of depression to qualify for the screening; however, to be covered, it must take place in a primary care setting, such as a doctor's office.
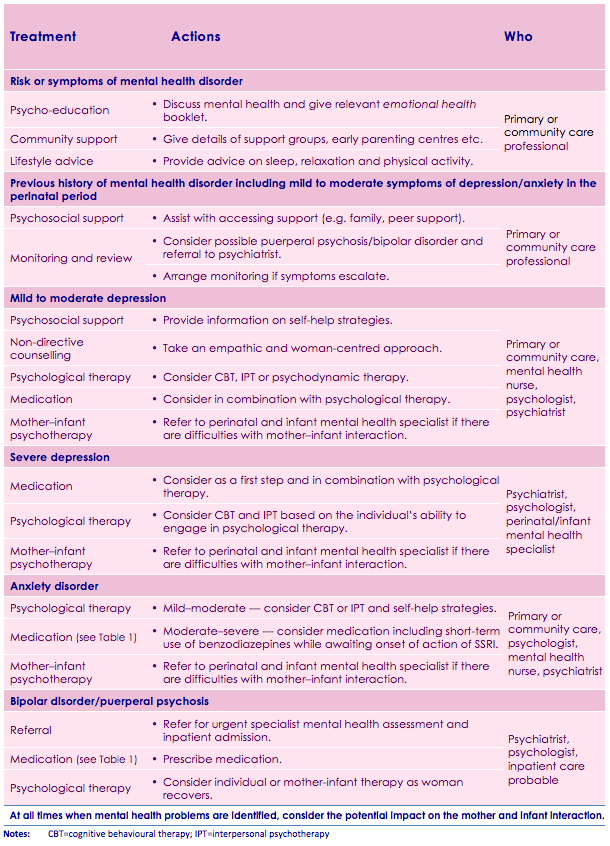
Medicare depression screening questionnaire
The Patient Health Questionnaire (PHQ) is the most commonly used test for depression screening. Most depression screenings are a two-step process. The first questions you will be asked are:
Medicare coverage for other mental health services
In addition to a depression screening, Medicare Part A and Part B covers other inpatient and outpatient mental health services.
Why take a depression screening?
Depression is extremely common in the U.S., but you may not feel depressed. Perhaps you aren’t experiencing some of the classic "symptoms" of depression. Or, maybe you don't recognize them in yourself.
How to apply for Medicare
If you begin receiving Social Security benefits at least 4 months before turning 65, you'll be automatically enrolled in Medicare Part A and Part B when you're eligible.
How common is depression in older people?
Depression is an extremely common disease. The Centers for Medicare and Medicaid Services reports that one in six persons older than 65 suffer from depression and that depression in older patients occurs in 25% of those with other physical illnesses.
Is depression screening covered by Medicare?
Depression screenings are free under Medicare. In fact, under the current Medicare system, you are entitled to one free depression screening per year. That’s right; an annual depression screening is covered as a form of preventive maintenance under Medicare Part B. If you are enrolled in a Medicare plan, you’re eligible.
Is depression a stigma?
Over the past several years, the stigmas associated with mental illnesses such as depression have slowly begun to evaporate. If you’re 65 years of age or older, you were probably raised in a society that tended to treat those suffering from depression as though they were invisible, or just needed to ‘cheer up.’.
Decision Summary
The Centers for Medicare & Medicaid Services (CMS) has determined that the evidence is adequate to conclude that screening for depression in adults, which is recommended with a grade of B by the U.S.
Decision Memo
The Centers for Medicare & Medicaid Services (CMS) has determined that the evidence is adequate to conclude that screening for depression in adults, which is recommended with a grade of B by the U.S.
What is the code for depression screening?
Code G0444 may be reported for an annual depression screening up to 15 minutes using any standardized instrument (e.g., PHQ-9) in a primary care setting with clinical staff who can advise the physician of screening results and who can facilitate and coordinate referrals to mental health treatment as necessary.
How many months does it take to get a depression screening?
Screening for depression is non-covered when performed more than one time in a 12-month period. Eleven full months must elapse following the month in which the last annual depression screening took place. Medicare coinsurance and Part B deductible are waived for this preventive service.
What is the HCPCS level 2 code for depression?
The CMS bulletin for this stated:#N#The provider must have in place staff-assisted depression care supports who can advise the physician of screening results and who can facilitate and coordinate referrals to mental health treatment. HCPCS Level II code is G0444 Annual depression screening, 15 minutes.#N#At a minimum level, staff-assisted depression care supports consist of clinical staff (e.g., nurse, Physician Assistant) in the primary care office who can advise the physician of screening results and who can facilitate and coordinate referrals to mental health treatment.#N#More comprehensive care supports include a case manager working with the primary care physician; planned collaborative care between the primary care provider and mental health clinicians; patient education and support for patient self management; plus attention to patient preferences regarding counseling, medications, and referral to mental health professionals with or without continuing involvement by the patient’s primary care physician.#N#Note: Coverage is limited to screening services and does not include treatment options for depression or any diseases, complications, or chronic conditions resulting from depression, nor does it address therapeutic interventions such as pharmacotherapy, combination therapy (counseling and#N#medications), or other interventions for depression. Self-help materials, telephone calls, and web-based counseling are not separately reimbursable by Medicare and are not part of this NCD.#N#Screening for depression is non-covered when performed more than one time in a 12-month period. Eleven full months must elapse following the month in which the last annual depression screening took place. Medicare coinsurance and Part B deductible are waived for this preventive service.
Can depression screen be billed with IPPE?
Depression Screen#N#G0444 is NOT able to be billed with G0402 (IPPE), but it can be billed with G0438 and G0439 as part of the the annual wellness visit. It cannot be performed with the IPPE, as it is a part of the IPPE and cannot be billed separately. You must perform the PHQ-9 not the PHQ-2 in order to bill the code. What's 7 more questions really? It will be covered and not applied to the patients deductible when performed during the annual wellness visit.
Is depression screening covered by Medicare?
Depression screening is only reimbursed during the Welcome to medicare or IPPE. Use appropriate screening questions or standardized questionnaires recognized by national. professional medical organizations to review, at a minimum, the following areas: