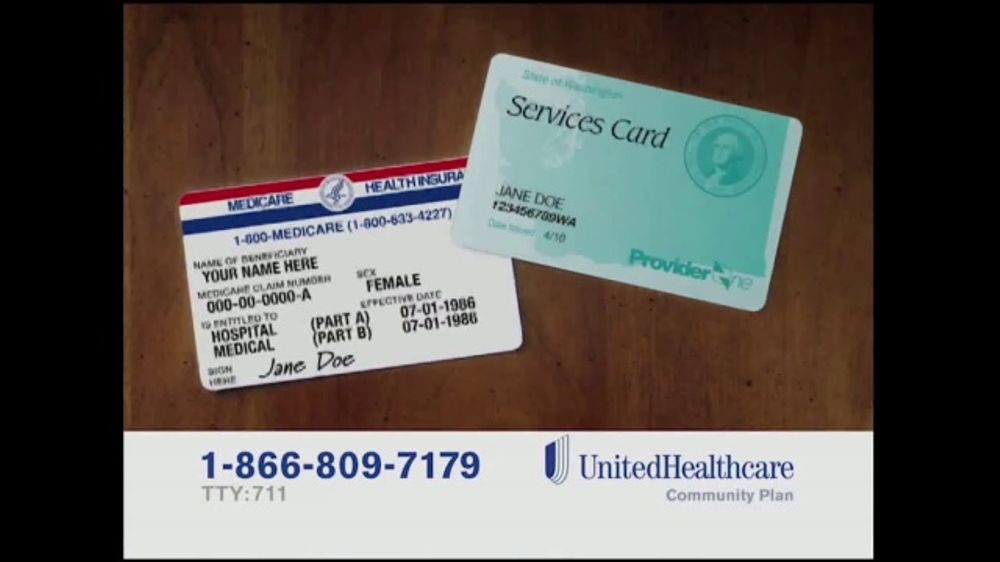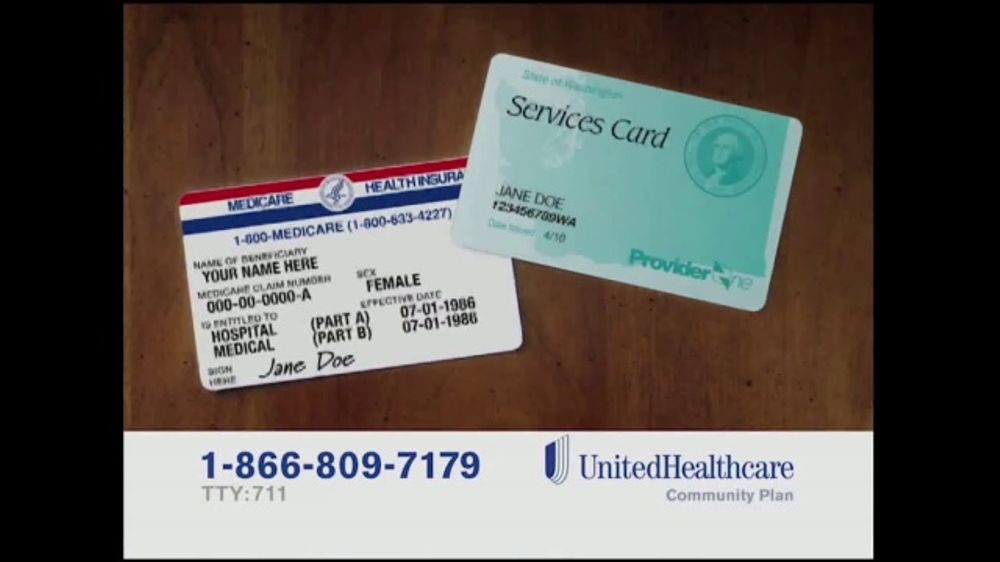
UnitedHealthcare Dual Complete (HMO D-SNP) is a 2021 Medicare Advantage Special Needs Plan plan by UnitedHealthcare. This plan from UnitedHealthcare works with Medicare to give you significant coverage beyond original Medicare. If you decide to sign up you still retain Original Medicare.
What is Medicare dual eligible and how do I qualify?
Jan 10, 2022 · A UnitedHealthcare Dual Complete plan is a DSNP that provides health benefits for people who are dually-eligible, meaning they qualify for both Medicare and Medicaid. Who qualifies? Anyone who meets the eligibility criteria for both Medicare and Medicaid is qualified to enroll in a DSNP.
What does dual eligible mean in Medicare?
Jul 08, 2020 · The term “full dual eligible” refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as “partial dual eligible.” *Cost sharing is the amount of your health care that you pay out of your own pocket.
What are the top 5 Medicare supplement plans?
Dec 08, 2021 · 61.9 million Americans are Medicare beneficiaries. 1 In 2019, more than 12 million Americans were dually eligible for Medicare and Medicaid and are enrolled in both programs. 2. Beneficiaries who are eligible for this combination of coverage are sometimes called Medicare dual eligible. If you are dual eligible for Medicare and Medicaid, you may qualify for a special …
What is full benefit dual eligible?
Jan 17, 2020 · UnitedHealthcare Dual Complete plans Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plan’s contract renewal with Medicare.

Is dual complete an Advantage plan?
Please check eligibility and benefits prior to providing services. UnitedHealthcare Dual Complete® (HMO D-SNP) is a Medicare Advantage plan.Jan 1, 2021
Is UnitedHealthcare dual complete a Medicare Advantage plan?
UHC Dual Complete includes both Medicare and Medicaid benefits. UHC Dual Complete plans cover everything found in Original Medicare (Medicare Part A and Part B). That includes both inpatient and outpatient care and durable medical equipment (DME).Sep 13, 2021
Is AARP Medicare Complete the same as Medicare?
AARP MedicareComplete is a Medicare Advantage health insurance plan that gives you both Medicare Part A and Part B along with additional benefits for drug coverage, hearing exams and wellness programs.
What are the 2 types of Medicare plans?
What's a Medicare health plan? Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
Does UnitedHealthcare Dual Complete have a deductible?
Annual Medical Deductible This plan does not have a deductible. Maximum Out-of-Pocket Amount (does not include prescription drugs) $0 annually for Medicare-covered services from in- network providers.Jan 1, 2021
What is a dual advantage plan?
Dual Advantage health coverage is for individuals who are “dual eligible,” meaning they qualify for both Medicare and Medicaid coverage.
Which two Medicare plans Cannot be enrolled together?
You generally cannot enroll in both a Medicare Advantage plan and a Medigap plan at the same time.Jun 2, 2021
What is the difference between Medicare Advantage and Medicare Complete?
Original Medicare covers inpatient hospital and skilled nursing services – Part A - and doctor visits, outpatient services and some preventative care – Part B. Medicare Advantage plans cover all the above (Part A and Part B), and most plans also cover prescription drugs (Part D).
What is the biggest difference between Medicare and Medicare Advantage?
With Original Medicare, you can go to any doctor or facility that accepts Medicare. Medicare Advantage plans have fixed networks of doctors and hospitals. Your plan will have rules about whether or not you can get care outside your network. But with any plan, you'll pay more for care you get outside your network.Oct 1, 2020
What is the biggest disadvantage of Medicare Advantage?
The primary advantage is the monthly premium, which is generally lower than Medigap plans. The top disadvantages are that you must use provider networks and the copays can nickel and dime you to death.Dec 12, 2021
Does Medicare cover dental?
Dental services Medicare doesn't cover most dental care (including procedures and supplies like cleanings, fillings, tooth extractions, dentures, dental plates, or other dental devices). Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
What is dual eligible?
Full dual eligible refers to those who receive full Medicaid benefits and are also enrolled in Medicare. People who are full dual eligible typically receive Supplemental Security Income (SSI) benefits, which provide cash assistance for basic food ...
What is a dual SNP?
If you are Medicare dual eligible, you may qualify for a Medicare D-SNP (Dual Special Needs Plan), which is a type of Medicare Advantage plan. 61.9 million Americans are Medicare beneficiaries. 1 In 2019, more than 12 million Americans were dually eligible for Medicare and Medicaid and are enrolled in both programs. 2.
Is Medicare the primary or secondary payer?
For dual eligible beneficiaries, Medicare serves as the primary payer, and Medicaid acts as the secondary payer. That means Medicare is the first to pay for covered services and items, and then Medicaid will help pay some or all of your remaining costs.
What is the difference between Medicare and Medicaid?
Medicaid include: Medicare is for people age 65 and over and for certain people under 65 who have a qualifying disability. Medicare eligibility is consistent for everyone across the U.S., no matter what state you live in.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments. Eligibility requires: Income of no more than $1,061 per month for an individual in 2019, or $1,430 per month for a married couple.
What is a SLMB?
Specified Low-Income Medicare Beneficiary (SLMB) Program. The SLMB program helps pay for Medicare Part B premiums. Eligibility requires: Income of no more than $1,269 per month for an individual in 2019, or $1,711 per month for a married couple.
What is a special needs plan?
A Medicare special needs plan is a certain type of Medicare Advantage plan that is designed for people with specific health conditions or circumstances. A D-SNP is built for the specific needs of dual eligibles. All Medicare SNPs (including Medicare D-SNPs) provide prescription drug coverage.
What makes this a plan for people who are dual-eligible?
Dual Special Needs Plans are for people who could use some extra help. That may be because of income, disabilities, age and/or health conditions. Dual Special Needs Plans are a type of Medicare Advantage plan. Dual Special Needs Plans are also called D-SNP for short. These names all mean the same thing.
How does dual coverage health insurance work with both Medicaid and Medicare?
A Dual Special Needs Plan works together with your Medicaid health plan. You’ll keep all your Medicaid benefits. Most dual health insurance plans also give you more benefits and features than you get with Original Medicare. All with as low as a $0 plan premium.
More help for you
Care coordination is another big benefit you get with a Dual Special Needs Plan. You’ll have a personal care coordinator. That’s someone who can help you:
What is Medicare dual eligible?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program for seniors and disabled persons, Medicaid is a state and federal medical assistance program for financially needy persons of all ages. Both programs offer a variety of benefits, including physician visits and hospitalization, but only Medicaid provides long-term nursing home care. Particularly relevant for the purposes of this article, Medicaid also pays for long-term care and supports in home and community based settings, which may include one’s home, an adult foster care home, or an assisted living residence. That said, in 2019, Medicare Advantage plans (Medicare Part C) began offering some long-term home and community based benefits.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
How old do you have to be to apply for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
Does Medicare provide long term care?
Long-Term Care Benefits. Medicaid provides a wide variety of long-term care benefits and supports to allow persons to age at home or in their community. Medicare does not provide these benefits, but some Medicare Advantage began offering various long term home and community based services in 2019. Benefits for long term care may include ...
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Is there an age limit for Medicare?
Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
What is a dual complete HMO?
UnitedHealthcare Dual Complete (HMO D-SNP) is a Local HMO. With a health maintenance organization (HMO) you will be required to receive most of your health care from an in-network provider. Health maintenance organizations require that you select a primary care physician (PCP). Your PCP will serve as your personal doctor to provide all ...
What is a dual SNP?
All Medicare SNPs also provide Medicare additional Part-D drug coverage. UnitedHealthcare Dual Complete (HMO D-SNP) DS-H4590 is a Dual Eligible Special Needs Plan (D-SNP). A Dual Eligible SNP is for beneficiaries who are eligible for both Medicare and Medicaid. If you have Medicare and get help from Medicaid you can join any Medicare SNP you ...
What is HMO D SNP?
UnitedHealthcare Dual Complete (HMO D-SNP) is a 2021 Medicare Advantage Special Needs Plan plan by UnitedHealthcare. This plan from UnitedHealthcare works with Medicare to give you significant coverage beyond original Medicare. If you decide to sign up you still retain Original Medicare. But you will get additional Part A (Hospital Insurance) ...
How much will I have to pay for prescription drugs in 2021?
In 2021 once you and your plan provider have spent $4130 on covered drugs. (combined amount plus your deductible) You will be in the coverage gap. (AKA "donut hole") You will be required to pay 25% for prescription drugs unless your plan offers additional coverage.
What is the gap in 2021?
Gap Coverage. In 2021 once you and your plan provider have spent $4130 on covered drugs. (combined amount plus your deductible) You will be in the coverage gap. (AKA "donut hole") You will be required to pay 25% for brand-name drugs and 25% on generic drugs unless your plan offers additional coverage.
What is dual eligibility?
Dual Eligibility. If you qualify for both Medicare and Medicaid, you are considered "dual eligible.". Sometimes the two programs can work together to cover most of your health care costs. Individuals who are dual eligible can often qualify for special kinds of Medicare plans.
What is a federal health insurance program?
A federal health insurance program for people who are: 65 or older. Under 65 with certain disabilities. Of any age and have End Stage Renal Disease (ESRD) or Amyotrophic Lateral Sclerosis (ALS, also called Lou Gehrig's Disease)
Does each state have its own medicaid program?
Each state creates its own Medicaid program, but has to follow federal guidelines, like the required and optional benefits they include. Some of the benefits Medicaid programs have to include are: