Group Medicare Advantage plans are insurance plans offered by employers or unions to their retirees. EGWPs are provided by private insurance companies who manage your company’s retiree Medicare benefits. Under EGWPs, Medicare pays the insurance company a fixed amount to provide benefits.
What group of people are covered under Medicare?
The program was designed to cover those groups or categories of people who are eligible to receive cash payments under one of the existing welfare programs established under the Social Security Act; that is, Title IV-A, the program of Aid to Families with Dependent Children (AFDC), or Title XVI, the Supplemental Security Income (SSI) program for the aged, blind, and disabled.
Which is primary Medicare or group insurance?
Medicare is primary when your employer has less than 20 employees. Medicare will pay first and then your group insurance will pay second. If this is your situation, it’s important to enroll in both parts of Original Medicare when you are first eligible for coverage at age 65. This rule applies for spouses on the same coverage as well.
What are the top 5 Medicare supplement plans?
- Plan G
- Plan N
- Plan A
- Plan F
- High Deductible Plan F
What are the best Medicare plans?
... Jerry represent most of the supplement plan and drug -plan carriers and all Medicare advantage plan carriers. Sign up today for a FREE virtual event and let Silver Supplements Solutions help you understand your best option for your own peace of mind!
Is Medicare a primary or group?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
What groups are covered by Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
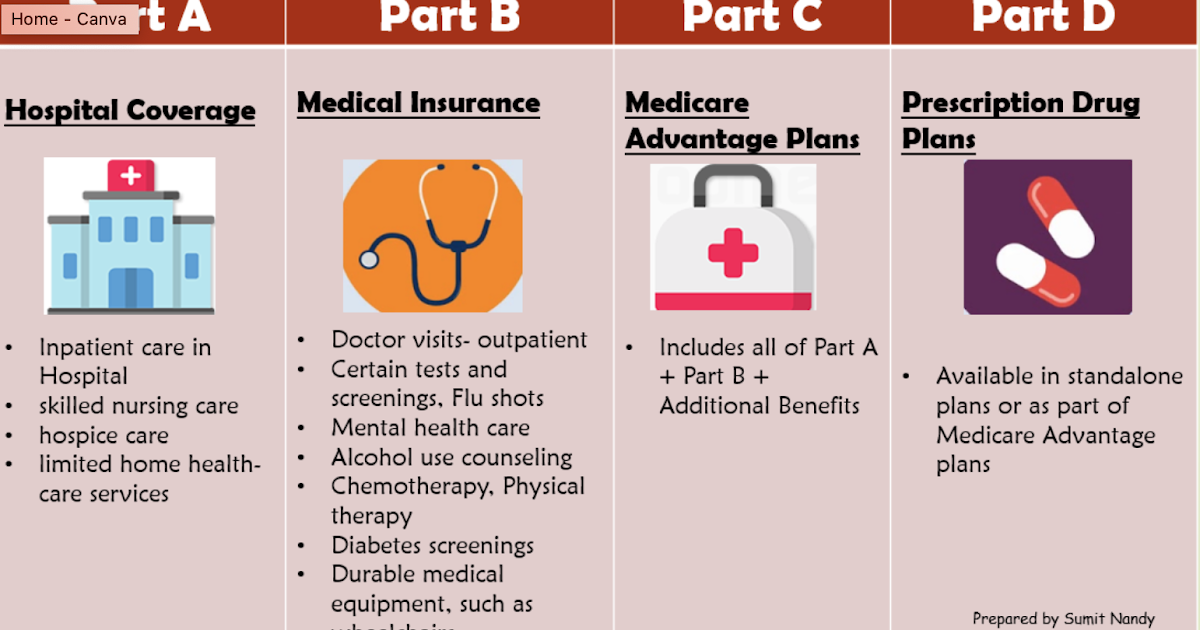
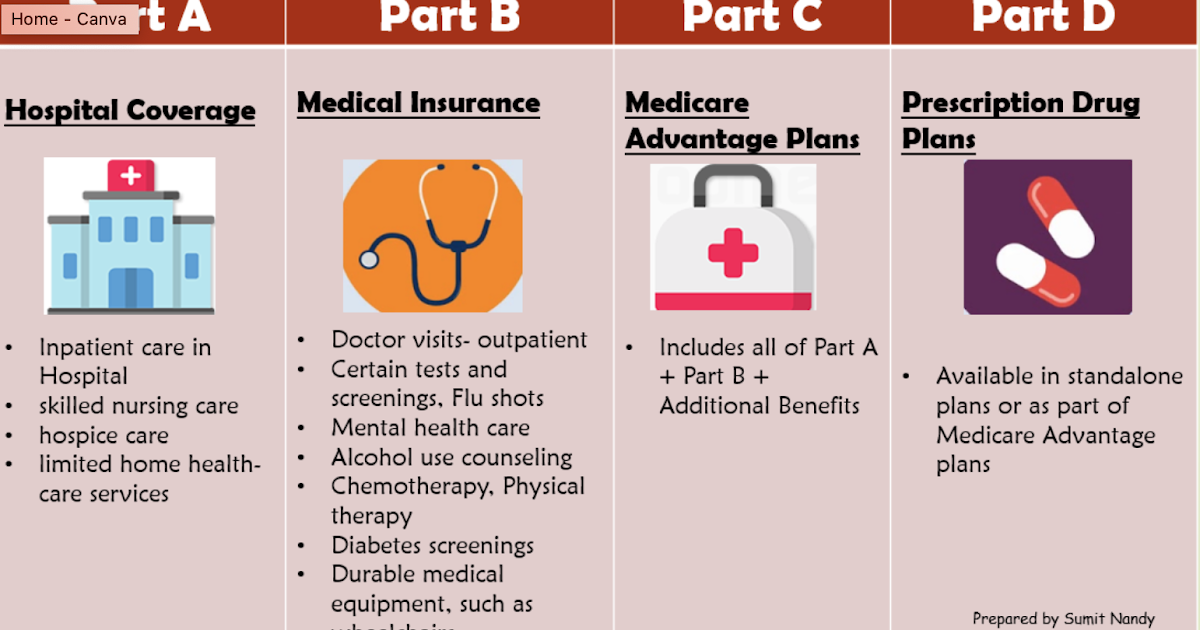
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What are the three types of Medicare?
The different parts of Medicare help cover specific services:Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.Medicare Part B (Medical Insurance) ... Medicare Part D (prescription drug coverage)
What type of Medicare do I have?
Visit the Check Your Enrollment page on Medicare.gov, the official website for Medicare. Fill out the requested information, including your zip code, Medicare number, name, date of birth and your effective date for Medicare Part A coverage or Part B coverage.
Is Medicare and Medicaid the same?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What is the difference between Medicare A and B?
Medicare Part A and Medicare Part B are two aspects of healthcare coverage the Centers for Medicare & Medicaid Services provide. Part A is hospital coverage, while Part B is more for doctor's visits and other aspects of outpatient medical care.
What are the two types of Medicare plans?
There are 2 main ways to get Medicare: Original Medicare includes Medicare Part A (Hospital Insurance) and Part B (Medical Insurance). If you want drug coverage, you can join a separate Medicare drug plan (Part D). as “Part C”) is an “all in one” alternative to Original Medicare.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
What is Medicare Part C called?
A Medicare Advantage is another way to get your Medicare Part A and Part B coverage. Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are offered by Medicare-approved private companies that must follow rules set by Medicare.
Does everyone get Medicare?
Everyone pays premiums for both regardless of work history. If you are still working at 65, you don't have to sign up for Medicare — but there are benefits to signing up while still employed. Similarly, if you have never worked, you can still get Medicare.
Is Medicare Part A and B free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is Medicare DRG?
What exactly is a Medicare DRG? A Medicare DRG (often referred to as a Medicare Severity DRG) is a payment classification system that groups clinically-similar conditions that require similar amounts of inpatient resources. It’s a way for Medicare to easily pay your hospital after an inpatient stay.
What does DRG mean in Medicare?
A DRG dictates how much Medicare pays the hospital if you’re admitted as an inpatient. However, keep in mind that your DRG does not affect what you owe for an inpatient admission when you have Medicare Part A coverage, assuming you receive medically necessary care and that your hospital accepts Medicare.
Why was the DRG system created?
The DRG system was created to standardize hospital reimbursement for Medicare patients while also taking regional factors into account. Another goal was to incentivize hospitals to become more efficient. If your hospital spends less money taking care of you than the DRG payment it receives, it makes a profit.
How is a DRG determined?
How is a Medicare DRG determined? A Medicare DRG is determined by the diagnosis that caused you to become hospitalized as well as up to 24 secondary diagnoses (otherwise known as complications and comorbidities) you may have. Medical coders assign ICD-10 diagnosis codes to represent each of these conditions.
How to contact Medicare DRG?
Speak with a licensed insurance agent. 1-800-557-6059 | TTY 711, 24/7. Your Medicare DRG is based on your severity of illness, risk of mortality, prognosis, treatment difficulty and need for intervention as well as the resource intensity necessary to care for you. Here’s how it works:
How long does it take for Medicare to readmit a patient?
However, Medicare has rules in place that penalize hospitals in certain circumstances if a patient is readmitted within 30 days. This deters premature discharges and helps ensure Medicare patients are discharge only when they are truly ready to go home or to another post-discharge care setting.
Does Medicare have an out-of-pocket spending limit?
All Medicare Advantage plans are required to include an annual out-of-pocket spending limit, which Original Medicare doesn't offer. Inpatient hospital care costs can add up quickly, depending on your diagnosis related group and the services you receive.
What is Medicare for people 65 and older?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
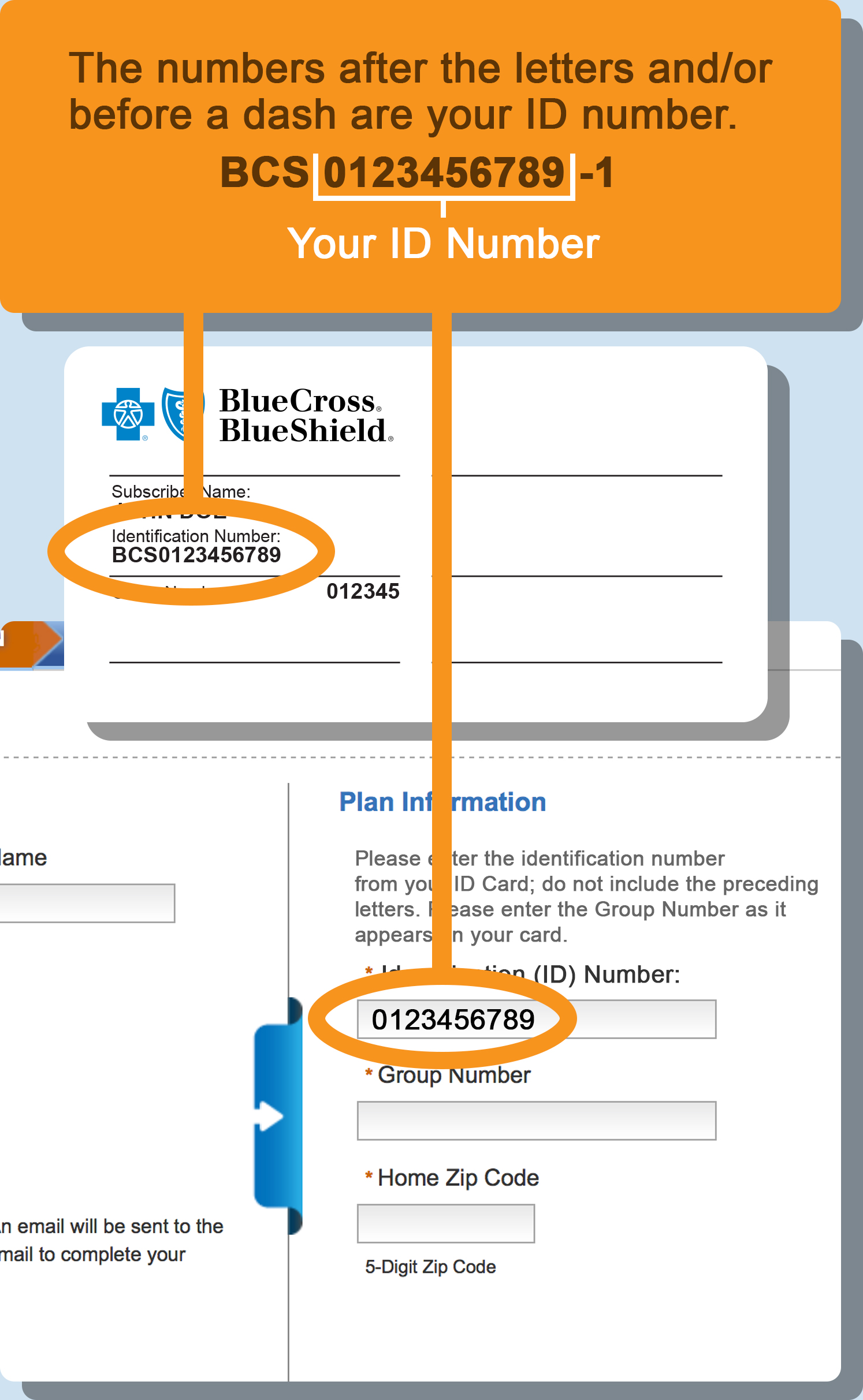
What Is My Member Id Number
What is insurance group number? Almost all insurance plans will assign you a member ID number, regardless of whether it is employer based or not. This number is individual to you specifically, whereas the insurance group number can apply to multiple people who have the same employer as you, as well as their dependents.
Not Sure If You Have An Npi
A suspension, termination, or revocation of a license to provide health care by a state licensing authority or the Medicaid Program
Provider Enrollment Site Visits
In 2011, CMS implemented a site visit verification process using a National Site Visit Contractor . A site visit is a screening to prevent questionable providers and suppliers from enrolling or staying enrolled in the Medicare Program.
What Is Medicaid Policy Number
Your Medicaid number also known as a recipient number or individual number is a 9-digit number than can be found on the Your Texas Benefits card. Doctors and pharmacies use this number for billing. Your case number can be found on letters you receive from HHSC or you may also request it from a rep at 211.
Im A New Member Is There Anything I Can Do Before I Receive My Member Id Card
While youre watching the mail for your member ID card to arrive, there are a few things you can do while youre waiting for your coverage to start, including looking for network providers and learning how to register for a health plan account.
How To Shop For Group Medicare Advantage Plans
If your company offers you an EGWP, you may need to talk to the companys insurance representative. Some things to consider about EGWPs include:
Where Can You Find Your Medicare Claim Number
Your Medicare claim number, or Medicare Beneficiary Identifier is an 11-character number Medicare uses to identify you. Learn how to find your number and how to use it to file a Medicare claim or track your Medicare claim status.
What Is a Health Insurance Group Number?
A group number is assigned to the employer or other group that sponsors an insurance plan for its employees or other individuals covered by the group plan. Each member of the group will share the same group number, but each person will have their own unique member number.
Does Private Medicare Have Group Numbers?
Original Medicare is not group coverage and therefore has no corresponding group number. But private Medicare plans may have a group number associated with the plan.
What Is a Medicare Group?
While Original Medicare is not group coverage, there are some group Medicare insurance plans available from private insurance companies.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
Our Services
Repeat Prescriptions We offer a free prescription collection and delivery service and text messages when your item is ready.
Innovation in MediCare
MediCare Pharmacy Group is committed to investing in the future of pharmacy. We use cutting-edge robotic technology to improve the speed, efficiency and accuracy of the dispensing services we provide.
Featured products
Our Click & Collect online store offers a wide range cosmetic products, fragrances and gifts.
Free Prescription Collection
MediCare Pharmacy Group offers a free prescription collection & delivery Service. It's easy, convenient and saves you time! All you have to do is…
Ask Your Pharmacist Week
It’s national Ask Your Pharmacist Week from 2nd-9th November 2020. The theme of this year’s campaign is ‘Your local pharmacy in the NHS...
Covid-19 Pharmacy Heroes
As the lockdown restrictions begin to ease, we are continuing to improve access to our pharmacies with the installation of new protective...
We have 53 stores across NI
MediCare Pharmacy Group has 53 stores across Northern Ireland. Click on the link below to locate your nearest store and see opening hours,
What is a DRG?
A diagnosis related group, or DRG, is a way of classifying the costs a hospital charges Medicare or insurance companies for your care. The Centers for Medicare & Medicaid Services (CMS) and some health insurance companies use these categories to decide how much they will pay for your stay in the hospital. CMS and insurers have created metrics and ...
What is the DRG system?
One the one hand, the system prods hospitals to increase efficiency and use only the necessary treatments, to keep costs down. On the other hand, some hospitals may attempt to discharge patients as quickly as possible.
How does DRG work?
How DRGs Work. Medicare pays your hospital a pre-set amount for your care, which is based on your DRG or diagnosis. These payments are processed under what is known as the inpatient prospective payment system (IPPS). Medicare assigns you to a DRG when you are discharged from the hospital. The DRG is determined by your primary diagnosis, ...
How is DRG determined?
Medicare assigns you to a DRG when you are discharged from the hospital. The DRG is determined by your primary diagnosis, along with as many 24 secondary diagnoses. CMS determines what each DRG payment amount should be by looking at the average cost of the products and services that are needed to treat patients in that particular group.
What is the goal of DRG?
The goal of the DRG system is to save on costs. When the hospital spends less than the predetermined DRG payment for a patient’s condition, it makes a profit. Conversely, if it spends more than the DRG payment, it suffers a loss. Like most complex systems, the DRG payment system has both benefits and problems.
What are the factors that determine the CMS base rate?
Among the factors considered are: Primary diagnosis. Secondary diagnoses. Comorbidities (other health conditions) Necessary medical procedures. Age. Gender. CMS first sets a base rate, which is recalculated every year and released to hospitals, insurers and other health providers.
What age is Medicare?
Retiree Health Plans. Individual is age 65 or older and has an employer retirement plan: Medicare pays Primary, Retiree coverage pays secondary. 6. No-fault Insurance and Liability Insurance. Individual is entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What age does GHP pay?
Individual is age 65 or older, is covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, ...
Does GHP pay for Medicare?
GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, is self-employed and covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary.