What does a5500 code mean on HCPCS?
11 rows · A5500 is a valid 2022 HCPCS code for For diabetics only, fitting (including follow-up), custom ...
What does a5500-a5514 stand for?
A5500 is a standardized code for Medicare and other health insurance providers to provide healthcare claims. Diabetic shoes (sometimes referred to as extra depth, therapeutic shoes or Sugar Shoes) are intended to reduce the risk of skin breakdown in diabetics with pre-existing foot disease. Our shoes are designed to help.
What is an a5500 shoe?
The Healthcare Common Procedure Coding System (HCPCS) is a collection of codes that represent procedures, supplies, products and services which may be provided to Medicare beneficiaries and to individuals enrolled in private health insurance programs.
What products can be billed with a code a5514?
The HCPCS codes range Diabetic Footwear A5500-A5514 is a standardized code set necessary for Medicare and other health insurance providers to provide healthcare claims. Subscribe to …

What is Medicare Code A5500?
HCPCS code A5500 for For diabetics only, fitting (including follow-up), custom preparation and supply of off-the-shelf depth-inlay shoe manufactured to accommodate multi- density insert(s), per shoe as maintained by CMS falls under Diabetic Footwear .
What is A5500 Diabetic shoe?
A5500 is a standardized code for Medicare and other health insurance providers to provide healthcare claims. Diabetic shoes (sometimes referred to as extra depth, therapeutic shoes or Sugar Shoes) are intended to reduce the risk of skin breakdown in diabetics with pre-existing foot disease.
Does Medicare pay for foot orthotics?
Medicare Part B pays for 80 percent of the approved cost of either custom-made or pre-made orthotic devices. Of course, this is only possible if your health care provider feels it is medically necessary. Medicare categorizes orthotics under the durable medical equipment (DME) benefit.
Does Medicare cover shoes for neuropathy?
Medicare will cover the cost of one pair of extra-depth shoes (diabetic shoes) and three pairs of inserts for diabetics but only if they have a medical need for them. Extra-depth shoes may be medically necessary as a protection for insensitive feet or against diabetic neuropathy (nerve damage in the feet).
Can a podiatrist write a prescription for diabetic shoes?
The doctor who treats your diabetes must certify your need for therapeutic shoes or inserts. A podiatrist (foot doctor) or other qualified doctor must prescribe the shoes or inserts, and you must get the shoes or inserts from one of these: A podiatrist. An orthotist.
What is special about diabetic shoes?
Diabetic shoes decrease the risk of diabetic foot ulcers and thereby reduce amputations. They provide support and protection while minimizing pressure points on the feet. They also have extra depth to accommodate diabetic inserts. There are many styles to choose from, and the shoes look much like any other shoe.
How are orthotics covered by Medicare?
Orthotics are devices used to treat injured muscles and joints. Medicare will typically cover 80 percent of the costs for orthotic devices under Medicare Part B if they are deemed medically necessary by a doctor. You are still responsible for 20 percent of the cost after you meet your deductible.
Does Medicare cover podiatry for plantar fasciitis?
Yes, as long as you met the eligibility requirements, your doctor can give you a prescription for treatment. Plantar Fasciitis is a severe breakdown of the soft tissue around your heel. This can be extremely painful and make it difficult to walk.
Does Medicare cover foot problems?
Foot care coverage Medicare Part B covers outpatient care, including cover for a podiatrist to evaluate and treat conditions at their office. For example, treatment could be for a foot injury, foot infection, or diabetes. Part B also pays for medically necessary care related to foot changes such as: bunions.
Can neuropathy in feet be cured?
There is no cure for peripheral neuropathy but proper treatment will slow progression and address your symptoms. If the cause of the foot neuropathy is known, then treatment of the underlying cause may provide relief.
What can you do for neuropathy in your feet?
To help you manage peripheral neuropathy:Take care of your feet, especially if you have diabetes. Check daily for blisters, cuts or calluses. ... Exercise. ... Quit smoking. ... Eat healthy meals. ... Avoid excessive alcohol. ... Monitor your blood glucose levels.
What shoes are best for diabetic neuropathy?
Some of the best shoes for neuropathyPropét Women's Tour Walker Strap Sneaker.Orthofeet Men's Lava Stretch Knit.Dr Comfort Women's Lu Lu.Dr Comfort Men's Stallion.Skechers Women's GOwalk Arch Fit – Classic Outlook.Skechers Men's After Burn – Memory Fit.
What is the HCPCS code for Medicare?
HCPCS Code. A5500. The Healthcare Common Procedure Coding System (HCPCS) is a collection of codes that represent procedures, supplies, products and services which may be provided to Medicare beneficiaries and to individuals enrolled in private health insurance programs.
How many pricing codes are there in a procedure?
Code used to identify the appropriate methodology for developing unique pricing amounts under part B. A procedure may have one to four pricing codes.
What is CMS type?
The carrier assigned CMS type of service which describes the particular kind (s) of service represented by the procedure code.
What is the A5512?
A5512. For diabetics only, multiple density insert, direct formed, molded to foot after external heat source of 230 degrees Fahrenheit or higher, total contact with patient's foot, including arch, base layer minimum of 1/4 inch material of shore a 35 durometer or 3/16 inch material of shore a 40 durometer (or higher), prefabricated, each.
What is the HCPCS code for diabetic footwear?
The HCPCS codes range Diabetic Footwear A5500-A5514 is a standardized code set necessary for Medicare and other health insurance providers to provide healthcare claims.
What is code A5514?
Code A5514 describes a total contact, custom fabricated, multiple density, removable inlay that is directly milled from a rectified virtual model of the beneficiary's foot so that it conforms to the plantar surface and makes total contact with the foot, including the arch. A custom fabricated device is made from materials that do not have predefined trim lines for heel cup height, arch height and length, or toe shape.
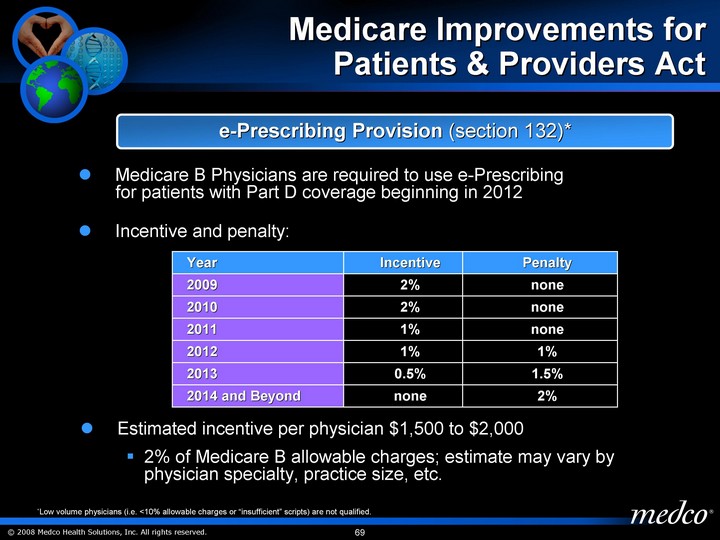
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administration of the Medicare, Medicaid and the State Children's Health Insurance Programs, contracts with certain organizations to assist in the administration of the Medicare program. Medicare contractors are required to develop and disseminate Articles. CMS believes that the Internet is an effective method to share Articles that Medicare contractors develop. While every effort has been made to provide accurate and complete information, CMS does not guarantee that there are no errors in the information displayed on this web site. THE UNITED STATES GOVERNMENT AND ITS EMPLOYEES ARE NOT LIABLE FOR ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION, PRODUCT, OR PROCESSES DISCLOSED HEREIN. Neither the United States Government nor its employees represent that use of such information, product, or processes will not infringe on privately owned rights. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information, product, or process.
Can you use CPT in Medicare?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of CMS internally within your organization within the United States for the sole use by yourself, employees and agents. Use is limited to use in Medicare, Medicaid or other programs administered by the Centers for Medicare and Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
Is ICD-10 code sufficient?
The presence of an ICD-10 code listed in this section is not sufficient by itself to assure coverage. Refer to the Non-Medical Necessity Coverage and Payment Rules section for other coverage criteria and payment information.
Who must review and verify all of the NP or PA notes in the medical record pertaining to the provision of therapeutic
The supervising physician must review and verify (sign and date) all of the NP or PA notes in the medical record pertaining to the provision of the therapeutic shoes, acknowledging their agreement with the actions of the NP or PA.
Is CPT a year 2000?
CPT is provided “as is” without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon no upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
Does Medicare cover shoe modifications?
Medicare will cover shoe modifications instead of inserts.
What is Medicare reimbursement form?
The Medicare reimbursement form, also known as the “Patient’s Request for Medical Payment, ” is available in both English and Spanish on the Medicare website.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
Does Medicare reimburse doctors?
Medicare Reimbursement for Physicians. Doctor visits fall under Part B. You may have to seek reimbursement if your doctor does not bill Medicare. When making doctors’ appointments, always ask if the doctor accepts Medicare assignment; this helps you avoid having to seek reimbursement.
Can you get a surprise bill from a doctor?
However, occasionally you may receive a surprise bill from a doctor that was involved in your inpatient treatment. If this happens, contact the doctor and find out if they accept Medicare assignment and if and when they plan to submit the claim to Medicare.
Does Medicare cover nursing home care?
Your doctors will usually bill Medicare, which covers most Part A services at 100% after you’ve met your deductible.