The Merit-based Incentive Payment System (MIPS) is one way to participate in the Quality Payment Program (QPP), a program authorized by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). The program changes how we reimburse MIPS eligible clinicians for Part B covered professional services and rewards them for improving the quality of patient care and outcomes.
How do I Pay my Medicare payment?
The incentive payment, with the remittance advice, will be issued by Carrier/MAC and identified as a separate payment under the eRx Incentive Program. Medicare contractors will use the indicator of LE (“Levy”) to indicate federally mandated payments. LE will appear in the PLB-03-1 segment of the 835.
How do we determine MIPS eligibility?
Participation Options Overview. Your MIPS eligibility status is specific to each practice ( TIN) you’re associated with and is based on the following 4 factors: your clinician type; the date you enrolled as a Medicare provider; whether you meet or exceed all three elements of the low-volume threshold; and. whether you’ve achieved QP status.
How does MIPS payment work?
Jan 19, 2022 · The Merit-Based Incentive Payment System (MIPS) determines Medicare payment adjustments; by utilizing a scoring system, eligible clinicians (ECs) might earn a payment bonus, penalty, or no adjustment. This is one of two paths for Medicare B providers to operate on a performance-based payment system under the Quality Payment Program (QPP).
Do you pay premiums on Medicare?
Jun 27, 2021 · 2021 APM Incentive Payment Details. The Centers for Medicare & Medicaid Services (CMS) has published 2021 Alternative Payment Model (APM) Incentive Payment details on the Quality Payment Program (QPP) website. To access this information, clinicians and surrogates can now log in to the QPP website using their HARP credentials.
What are Medicare incentives?
Incentive payments to eligible professionals, eligible hospitals, and critical access hospitals that demonstrate meaningful use of certified EHR technology. Uses a combination of incentive payments and payment adjustments to promote reporting of quality information by eligible professionals.
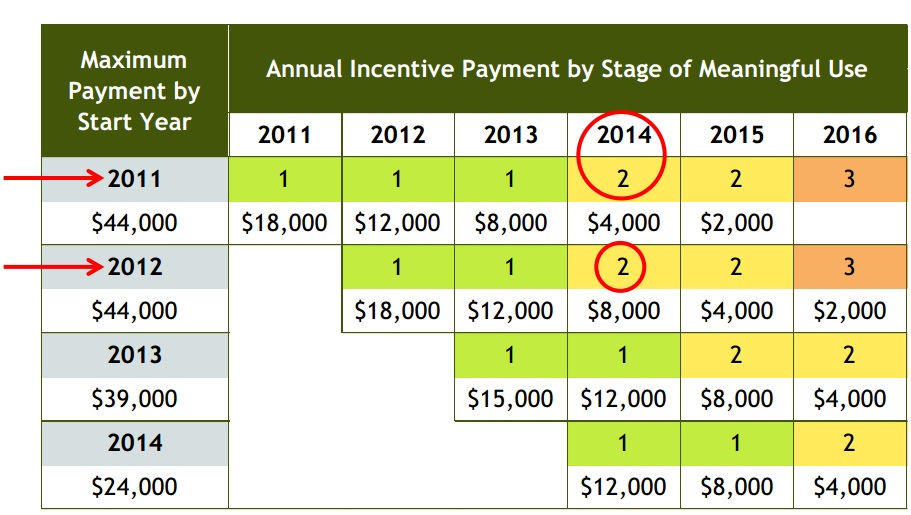
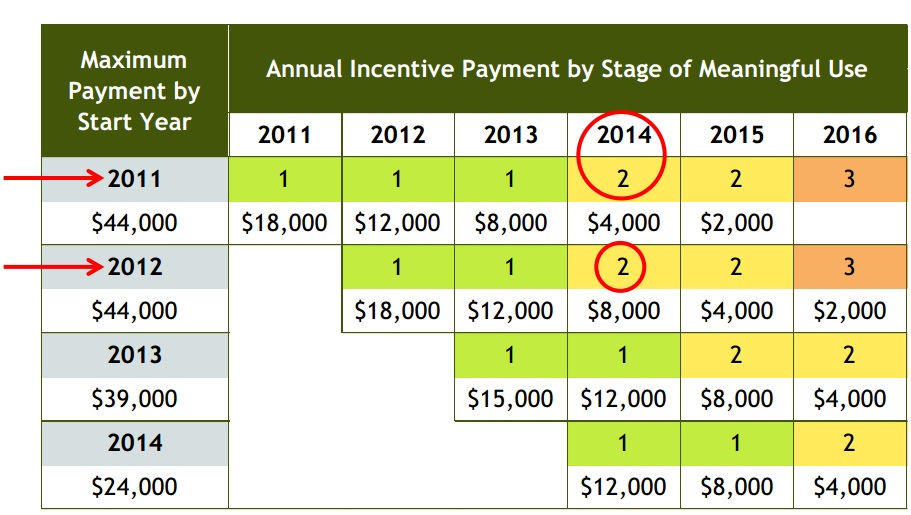
How much is the meaningful use incentive?
The maximum incentive payment is $63,750 per eligible professional, paid over 6 years. The first year payment is $21,250, and $8,500 per year for subsequent years.
What are the benefits of MIPS?
Establishment of MIPS provides an opportunity to revise, rework and improve the existing Medicare programs focused on quality, costs and use of electronic health records to improve their relevance to real-world medical practice and reduce administrative burdens for physicians.
What are the goals of the merit-based incentive payment system?
According to the HHS, “MIPS was designed to tie payments to quality and cost-efficient care, drive improvement in care processes and health outcomes, increase the use of healthcare information, and reduce the cost of care.”Nov 5, 2019
What is merit based incentive payment MIPS?
The Merit-Based Incentive Payment System (MIPS) is the program that will determine Medicare payment adjustments. Using a composite performance score, eligible clinicians (ECs) may receive a payment bonus, a payment penalty or no payment adjustment.
What is a Medicare eligible professional EP under meaningful use?
An EP (as defined under this section) who furnishes 90% or more of his or her covered professional services in a hospital setting in the year preceding the payment year.
What's the downside to MIPS?
The other disadvantage to MIPS is that you could actually be forced to pay penalties. If you opt-in to the standard, flat-rate pay system, instead of the incentive based one, you know exactly how much you will get paid every time and never have to worry about penalties.Nov 20, 2017
What are the 4 MIPS categories?
MIPS includes four performance categories: Quality, Cost, Improvement Activities, and Promoting Interoperability (formerly Meaningful Use).
Is MIPS only for Medicare patients?
MIPS reporting of individual measures applies to all patients. Eligibility for a measure is based on CMS documentation (denominator criteria).
What are two items that exempt eligible clinicians from a merit-based incentive payment system?
A clinician is exempt from MIPS under the Low Volume Threshold if they have fewer than or equal to $90,000 annual allowed Medicare Part B charges and/or see 200 or fewer unique Medicare Part B patients, and/or offer 200 or fewer Medicare services.
What is a good MIPS score for 2021?
If you are an EC, MIPS performance in 2021 will determine your MIPS payment adjustment in 2023. Therefore, in 2021, you must achieve at least 60 points through your performance in the four MIPS performance categories to avoid a negative payment adjustment in 2023.Feb 3, 2021
What is MIPS and APM?
MIPS stands for Merit-Based Incentive Payment System, while APM stands for Alternative Payment Model. Health care providers need to begin the verification process this year, and the first payments under these systems will be made in 2019. Both MIPS and APMs are processes that use value-based payment models.
What is eRx feedback?
The Electronic Prescribing (eRx) Incentive Program Feedback Report User Guide is designed to assist eligible professionals, CMS-selected group practices, and their authorized users in accessing and interpreting the 2012 eRx Incentive Program feedback reports. For the 2012 eRx Incentive Program, the feedback reports reflect data from the Medicare Part B Physician Fee Schedule (PFS) claims received for the dates of service January 1, 2012 – December 31, 2012 that were processed into National Claims History (NCH) by February 22, 2013. Additionally in 2012, quality data was received from qualified registries and EHR systems for purposes of the eRx Incentive Program. The 2012 eRx incentive payment is scheduled to be distributed in the fall of 2013. To view click on the document titled "2012 eRx Feedback Report User Guide"in the "Downloads"section below.
When did sequestration end?
The American Taxpayer Relief Act of 2012 postponed sequestration for 2 months. As required by law, President Obama issued a sequestration order on March 1, 2013. Under these mandatory reductions, 2013 eRx Incentive Program incentive payments made to eligible professionals and group practices will be reduced by 2%.
Payment Details Available on QPP Website
CMS has taken time to ensure correct payments and information are available during the 2021 payment year. CMS’s process includes verifying eligible clinicians’ Advanced APM participation and the calculation of the APM Incentive Payment.
What Do I Need to Do in Order to Receive the APM Incentive Payment?
You will not need to do anything to receive your payment, unless CMS is unable to verify your Medicare billing information. If you do not receive your payment, you should find your name on this public notice, which indicates that you will need to verify your Medicare billing information.
Additional Information on Medicare
As a top advisor to physicians, I help increase practice profits by delivering hands-on, expert medical accounting/tax support, practice counsel, and revenue-building strategies. Read more →
What Does Incentive Payment Mean?
Incentive payments are paid to hospitals, private practices and other health care facilities that are able to prove that they are ready and willing to adopt electronic health record (EHR) systems.#N#This initiative is part of the American Recovery and Reinvestment Act (ARRA) of 2009, in which funds were allocated for the development of nationwide electronic health care records.
Techopedia Explains Incentive Payment
According to the Center for Medicare and Medicaid Services (CMS), ARRA will provide 90 percent in matching funds for states to plan activities that center around EHR development, including IT EHR university-based training (UBT) and education.#N#In order to receive incentive payments, acute-care hospitals need 10 percent of their patients to be Medicare/Medicaid patients, while non-hospital providers need 30 percent of their patients to come from Medicare/Medicaid patient populations.#N#Incentive payments are received through audits conducted to ensure proper payments are being made and that eligible providers (EP) and health care treating facilities and practices are following meaningful use (MU) guidelines set forth by the Health Information Technology for Economic and Clinical Health Act (HITECH), which is monitored by the Department of Health and Human Services (HHS).#N#Incentive payments were slated to begin in 2010 but they actually started in 2011.They will be provided for up to five years and those who have already implemented EHR systems are still eligible for incentive payments if they upgrade their systems..
What is MIPS in Medicare?
MIPS (Merit-based Incentive Payment System) The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is a federal legislation that required CMS to create the metric-driven Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program to reward clinicians for value over volume based on performance points scored according ...
How does TPCC measure Medicare?
The TPCC measure assesses total Medicare Parts A and B expenditures for a patient attributed to an individual clinician or clinician group during a performance period (Jan. 1 – Dec. 31) by calculating the risk-adjusted, per capita costs. Patients are attributed to a clinician or clinician group based on the amount of primary care services (shown in Table A) they received by their primary care clinician (PCC)—or specialist, if they don’t see a PCC—during the performance period. Attributable patients must reside in the United States and be enrolled in both Medicare Parts A and B (unless newly enrolled) for the full year. The case minimum for this measure is 20 attributable patients.
How many providers are included in the additional measure for all cause hospital readmissions?
Practices with 16 or more providers and at least 200 eligible cases are included in the additional measure for All-Cause Hospital Readmissions. CMS will calculate this measure from claims data and will score in the same way as the other Quality measures (that have benchmarks), from 3 to 10 points.
What is improvement activity?
The Improvement Activities (IA) performance category focuses on care coordination, beneficiary engagement, and patient safety. Changes in Year 4 include two new activities, seven modified activities, and 15 removed activities.
What is episode based measure?
Episode-based measures only look at items and services related to applicable episodes of care, identified by procedure and diagnosis codes reported on Medicare B claims or Medicare Severity Diagnosis-related Group (MS-DRG) codes on Medicare Part A claims.
What is MIPS point?
As you probably know, each MIPS point a provider earns above the performance threshold (PT) results in higher incentives. Conversely, each MIPS point below the PT, to an established limit, penalizes the provider. Because few providers will receive a zero-payment adjustment resulting from their 2020 MIPS scores, rewards in the 2022 payment year will exceed dollar amounts awarded in the first 3 years of the program.
What is HSIP in Medicare?
HSIP was developed to improve Medicare beneficiary access to major surgical procedures. Incentives are for physicians enrolled as general surgeons when providing surgical procedures defined by a 10-day or 90-day global period.
What is HPSA designation?
HPSA designations are a function of the Bureau of Primary Health Care, Division of Shortage Designations (BPHC DSD) in conjunction with the US Census Bureau. Noridian does not determine zip code or county designations.
What is a HPSA?
Health Professional Shortage Area (HPSA) HPSA s are geographic areas, or populations within geographic areas, that lack sufficient health care providers to meet the health care needs of the area or population.