
What are the LIS levels for Medicare?
The LEP is an amount that is permanently added to your Medicare Part D Prescription Drug coverage premium.How does it happen?
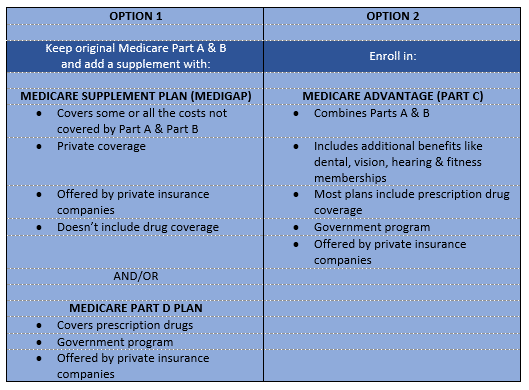
Which Medicare plan is right for me?
The late enrollment penalty is an amount that's permanently added to your Medicare drug coverage (Part D) premium. You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there's a period of 63 or more days in a row when you don't have Medicare drug coverage or other. creditable prescription drug coverage
What are the stages of Medicare Part D?
The late enrollment penalty (also called the “LEP” or “penalty”) is an amount that may be added to a person’s monthly premium for Medicare drug coverage (Part D).
What to expect with Medicare?
A Medicare Late Enrollment Penalty (LEP) is an additional monthly amount you will be required to pay to Medicare if you did not enroll in Medicare Part B and/or D when you first became eligible. Additionally, for those that have to pay for Medicare Part A, there is also a late enrollment penalty for not signing up when first eligible, which is typically when you turn 65.
Why does Medicare charge LEP?
The purpose of the LEP is to encourage Medicare beneficiaries to maintain adequate drug coverage. The penalty is 1% of the national base beneficiary premium ($33.37 in 2022) for every month you did not have Part D or certain other types of drug coverage while eligible for Part D.
How can I avoid Medicare Part D Penalty?
3 ways to avoid the Part D late enrollment penaltyEnroll in Medicare drug coverage when you're first eligible. ... Enroll in Medicare drug coverage if you lose other creditable coverage. ... Keep records showing when you had other creditable drug coverage, and tell your plan when they ask about it.
What is LEP amount?
The late enrollment penalty (also called the “LEP” or “penalty”) is an amount that may be added to a person's monthly premium for Medicare drug coverage (Part D).
Why do I have LEP?
A Late Enrollment Penalty (LEP) is issued when you have a lapse in coverage. You pay a penalty for the amount of time you have gone without coverage. The penalty is added to your Medicare plan's monthly premium for the remainder of the time you are on a Medicare plan.
Who has the cheapest Part D drug plan?
SilverScript Medicare Prescription Drug Plans Although costs vary by zip code, the average nationwide monthly premium cost of the SmartRX plan is only $7.08, making it the most affordable Medicare Part D plan on the market.
When did Part D become mandatory?
Medicare Part D Prescription Drug benefit Under the MMA, private health plans approved by Medicare became known as Medicare Advantage Plans. These plans are sometimes called "Part C" or "MA Plans.” The MMA also expanded Medicare to include an optional prescription drug benefit, “Part D,” which went into effect in 2006.Dec 1, 2021
How is Lep calculated?
The late enrollment penalty is calculated by multiplying 1% of the “national base beneficiary premium” ($32.74 in 2020) times the number of full, uncovered months the beneficiary didn't have Part D or other creditable coverage (but were eligible).
When did Medicare LEP start?
When the Part D program began in 2006, people already in Medicare could sign up until May 15 of that year without incurring a late penalty.
Do I need Medicare Part D if I don't take any drugs?
If you don't take any medications at all, you'll still want to enroll in Part D when you're first eligible (unless you have other creditable drug coverage), to avoid the late enrollment penalty described above.
What happens if I refuse Medicare Part D?
If you don't sign up for a Part D plan when you are first eligible to do so, and you decide later you want to sign up, you will be required to pay a late enrollment penalty equal to 1% of the national average premium amount for every month you didn't have coverage as good as the standard Part D benefit.
Can I cancel Medicare Part D?
To disenroll from a Medicare drug plan during Open Enrollment, you can do one of these: Call us at 1-800 MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Mail or fax a signed written notice to the plan telling them you want to disenroll.
What is formulary in Medicare?
Most Medicare drug plans have their own list of covered drugs, called a formulary. Plans cover both generic and brand-name prescription drugs. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes.
What is the LEP for Medicare Part B?
If you did not enroll in Medicare Part B when you were first eligible (during your Initial Enrollment Period- IEP) your monthly premium may go up 10% for each 12-month period you could have had Medicare Part B, but did were not enrolled. The penalty is based on the standard Medicare Part B premium, regardless of the premium amount you actually pay
Can I Avoid the Medicare Part B Penalty?
YES! If you are turning 65, and enroll in Medicare Part B during your Initial Enrollment Period (IEP), you will not incur a late penalty. If you don’t enroll in Medicare Part B during your IEP, typically you will have to wait for the General Enrollment Period (GEP) before you will be allowed to sign up.
When Does the Part B Penalty Not Apply?
If you miss the enrollment deadline during your Initial Enrollment Period (IEP) and sign up during the next General Enrollment Period, and that time period is within fewer than 12 full months, you will not pay a penalty.
Can I Appeal the Part B Penalty?
Yes! If you believe the Medicare Part B penalty should not apply to your current situation, you can ask for a review. Medicare has reconsideration request forms to file an appeal. Important note, you will still have to pay the penalty while waiting for your review to be processed.
Is there a Cap on the Part B Penalty?
Currently, there is no cap on the Medicare Part B late enrollment penalty.
What is the LEP for Medicare Part D?
The LEP is an amount that is permanently added to your Medicare Part D Prescription Drug coverage premium.How does it happen? You might owe a late enrollment penalty if you go without a Medicare Part D Prescription Drug plan or other creditable prescription drug coverage for any continuous period of 63 days or more after the end of your Initial Enrollment Period (or your Special Enrollment Period).
How is the Late Enrollment Penalty calculated Medicare Part D?
Medicare, not the individual plan, calculates the late enrollment penalty when you first enroll in a Medicare Part D Prescription Drug plan.
What happens if Medicare pays late enrollment?
If Medicare’s contractor decides that your late enrollment penalty is correct, the Medicare contractor will send you a letter explaining the decision, and you must pay the penalty.
What is the late enrollment penalty for Medicare?
Part D late enrollment penalty. The late enrollment penalty is an amount that's permanently added to your Medicare drug coverage (Part D) premium. You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there's a period of 63 or more days in a row when you don't have Medicare drug coverage or other.
What is creditable prescription drug coverage?
creditable prescription drug coverage. Prescription drug coverage (for example, from an employer or union) that's expected to pay, on average, at least as much as Medicare's standard prescription drug coverage. People who have this kind of coverage when they become eligible for Medicare can generally keep that coverage without paying a penalty, ...
Does Medicare pay late enrollment penalties?
, you don't pay the late enrollment penalty.
How long does Medicare cover a break?
When a person joins a Medicare drug plan, the plan will review Medicare’s systems to see if the person had a potential break in creditable coverage for 63 days or more in a row. If so, the Medicare drug plan will send the person a notice asking for information about prior prescription drug coverage. It’s very important that the person complete this form and return it by the date on the form, because this is the person’s chance to let the plan know about prior coverage that might not be in Medicare’s systems.
Is Mrs Martinez on Medicare?
Mrs. Martinez is currently eligible for Medicare, and her Initial Enrollment Period ended on May 31, 2016. She doesn’t have prescription drug coverage from any other source. She didn’t join by May 31, 2016, and instead joined during the Open Enrollment Period that ended December 7, 2018. Her drug coverage was effective January 1, 2019
Does Mrs Kim have Medicare?
Mrs. Kim didn’t join a Medicare drug plan before her Initial Enrollment Period ended in July 2017. In October 2017, she enrolled in a Medicare drug plan (effective January 1, 2018). She qualified for Extra Help, so she wasn’t charged a late enrollment penalty for the uncovered months in 2017. However, Mrs. Kim disenrolled from her Medicare drug plan effective June 30, 2018. She later joined another Medicare drug plan in October 2019 during the Open Enrollment Period, and her coverage with the new plan was effective January 1, 2020. She didn’t qualify for Extra Help when she enrolled in October 2019. Since leaving her first Medicare drug plan in June 2018 and joining the new Medicare drug plan in October 2019, she didn’t have other creditable coverage. However, she was still deemed eligible for Extra Help through December 2018. When Medicare determines her late enrollment penalty, Medicare doesn’t count:
How long does Medicare Part A last?
Additionally, for those that have to pay for Medicare Part A, there is also a late enrollment penalty for not signing up when first eligible, which is typically when you turn 65. The penalties for Parts B and D will last for your lifetime. For Part A, the maximum number of years the penalty can last is four.
What is the late enrollment penalty for Medicare Part D?
The late enrollment penalty for Medicare Part D is 1% of the average national base monthly premium, rounded to the nearest 10 cents for each month you did not enroll. This penalty is added to your premium each month you are enrolled, and generally lasts for as long as you have Medicare drug coverage.
What is Medicare late enrollment penalty?
What is a Medicare Late Enrollment Penalty? A Medicare Late Enrollment Penalty (LEP) is an additional monthly amount you will be required to pay to Medicare if you did not enroll in Medicare Part B and/or D when you first became eligible.
What is the penalty for Medicare Part A?
Medicare Part A Late Enrollment Penalties. The late enrollment penalty for Medicare Part A (for those who are not automatically enrolled), is 10% of your monthly premium if you miss your Medicare enrollment deadline. This is applied no matter how long the delay is, and the penalty is added to your premium cost for twice the number ...
Can you speculate on the amount of your Medicare penalty?
You can speculate on the amount of your penalty; however, you will be notified of the actual amount when you formally apply for Medicare Parts A, B or D. Once the government is aware of your enrollment into these parts of Medicare, they will calculate your penalty and send you, in writing, the actual amount you owe for the upcoming year. ...
