What makes a good Medicaid managed care plan?
- Medicaid Encounter Data System (MEDS) III Data Dictionary (PDF) Change Log
- Provider Network Data Dictionary (PDF) Change Log
- MRT 1458: Medicaid Managed Care Supplemental Information and Updates
- Questions & Answers on the Elimination of Direct Marketing Related to Contract Provisions (Section 11, Appendices D & P)
- Medicaid Prenatal Care Standards
What does managed care actually mean?
Understanding Medicare Managed Care Plans
- Medicare managed care plans are offered by private companies that have a contract with Medicare.
- These plans work in place of your original Medicare coverage.
- Many managed care plans offer coverage for services that original Medicare doesn’t.
- Medicare managed care plans are often known as Medicare Part C or Medicare Advantage plans.
How to apply for Medicaid Managed Care?
Medicaid Managed Care. Medicaid Managed Care offers many New Yorkers a chance to choose a Medicaid health plan. Managed Care plans focus on preventive health care and provide enrollees with a medical home for themselves and their families. Use this web site to find out more about Medicaid managed care where you live.
What are the types of managed care?
What are the four types of managed care plans?
- Health Maintenance Organization (HMO)
- Preferred Provider Organization (PPO)
- Point of Service Plan (POS)
- Exclusive Provider Organization (EPO)
Is Managed Medicare the same as Medicare?
Managed care plans are also referred to as Medicare Part C (Medicare Advantage) plans. These plans cover everything original Medicare does, and they often cover additional services as well. For example, original Medicare doesn't cover routine dental care, but many managed care plans do.
What does managed care mean in healthcare?
Managed Care is a health care delivery system organized to manage cost, utilization, and quality.
What is the difference between Medicare fee for service and Medicare managed care?
Under the FFS model, the state pays providers directly for each covered service received by a Medicaid beneficiary. Under managed care, the state pays a fee to a managed care plan for each person enrolled in the plan.
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Is Medicare a managed care plan?
Medicare is a national health insurance program for seniors or those with disabilities. Medicare Advantage is Medicare's managed care program. If you join Medicare Advantage, you get all your care through an HMO or PPO that has a contract with Medicare.
What is an example of a managed care plan?
A good example of a managed care plan is an HMO (Health Maintenance Organization). HMOs closely manage your care. Your cost is lowest with an HMO. You are limited to seeing providers in a small local network, which also helps keep costs low.
How does managed care work?
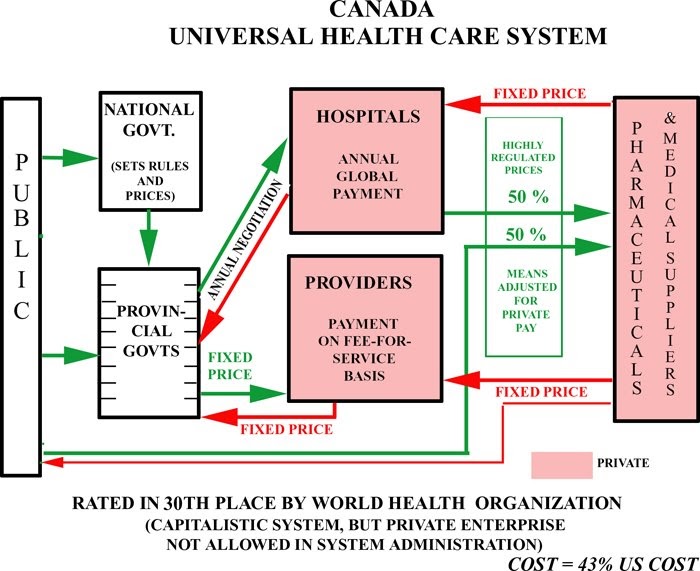
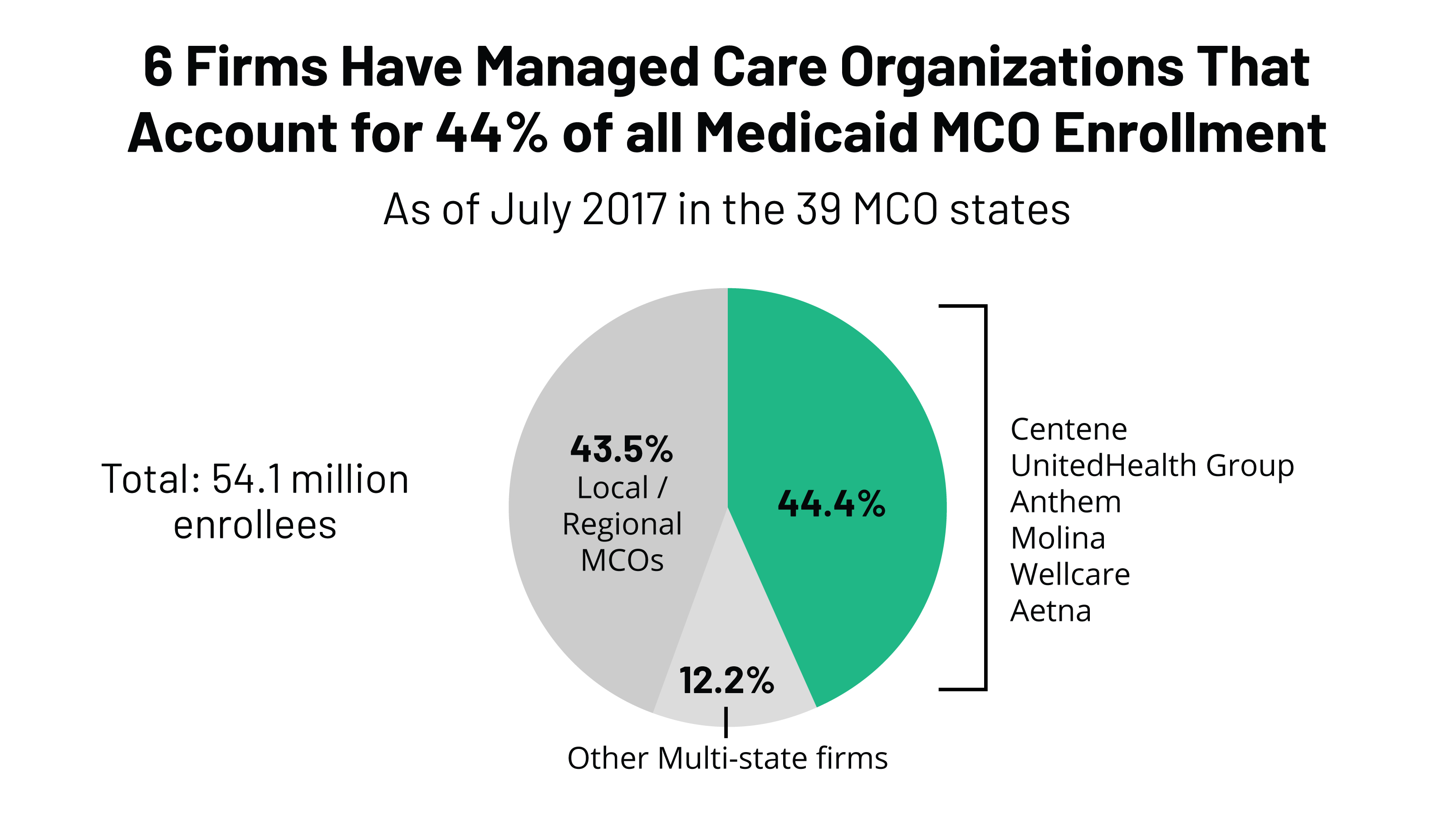
Under managed care, states sign contracts with "managed care organizations," or MCOs, that provide medical services through their own networks of doctors and hospitals. The state pays the MCO a fixed annual fee for each Medicaid patient. And the MCO takes responsibility for overseeing each person's care.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
What are the two types of Medicare plans?
There are 2 main ways to get Medicare: Original Medicare includes Medicare Part A (Hospital Insurance) and Part B (Medical Insurance). If you want drug coverage, you can join a separate Medicare drug plan (Part D).
Which is better PPO or HMO?
HMO plans typically have lower monthly premiums. You can also expect to pay less out of pocket. PPOs tend to have higher monthly premiums in exchange for the flexibility to use providers both in and out of network without a referral. Out-of-pocket medical costs can also run higher with a PPO plan.
What is Medicare A and B?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers.
What are the benefits of Medicare managed care?
Benefits can include routine vision, dental and hearing services. Additionally, managed care plans offer prescription drug coverage. The cost of medications out-of-pocket can be financially exhausting. Medicare managed care plans can provide some relief.
What is managed care plan?
Managed-care plans or Advantage plans bundles all health-care coverage under one neat plan. MA plans decide on rate amounts, making prices different from plan to plan. Processing payments are done through the private plan, not Medicare.
What is Medicare Advantage 2021?
Updated on March 19, 2021. Medicare managed care plans are an alternative to Original Medicare. Otherwise known as Medicare Advantage plans with many plan types, most are either HMOs or PPOs. Managed-care plans provide benefits for gaps in Parts A and B coverage. These alternative health-care plans make up Part C of Medicare.
What is indemnity health insurance?
Before HMOs, PPOs, and others, Indemnity plans were the main plans to choose from. Indemnity plans pre-determine the percentage of what they consider a reasonable and customary charge for certain services. Carriers pay a percentage of charges for a service and the member pays the remainder.
Does an indemnity plan have a provider network?
Members will receive reimbursement for medical expenses (up to a certain amount). Indemnity plans have no provider network, members can visit the doctor (s) of their choice. Contrarily, managed care plans have a network (s) of providers, with different plan options.
Does managed care plan limit doctors?
On the other hand, managed care plans may limit beneficiaries to only the doctors within the plan’s network. If having the freedom to see any healthcare provider of choice is important, remember that Advantage plans limit provider options. While traveling within the country, managed care pays for emergency services only.
Is Medicare Supplement the same as Managed Care?
Managed-care plans and Medicare Supplement plans are not the same. This misconception is common. Both provide additional benefits to Original Medicare. However, they serve two totally different purposes. Managed-care plans or Advantage plans bundles all health-care coverage under one neat plan.
What is Medicare managed care?
A Medicare managed care plan is a type of Medicare Advantage plan. Learn what managed care plans are and how they could be a good fit for you. A Medicare managed care plan is one type of Medicare Advantage plan. The term “managed care plan” generally refers to HMO (health maintenance organization), PPO (preferred provider organization) ...
What is managed care network?
The networks of managed care plans often include pharmacies, which can help make ordering and filling prescriptions faster and easier for everyone involved . There’s less uncertainty about a beneficiary’s costs for care in a managed care plan, provided they stay within the assigned network for qualified services.
What is a HMO plan?
Health maintenance organization (HMO) In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. Preferred provider organization (PPO)
What are the different types of Medicare plans?
Types of Medicare managed care plans 1 Health maintenance organization (HMO)#N#In a Medicare HMO plan, you use a primary care physician to coordinate your care, and you receive services from a network of health care providers that partner with your plan. 2 Preferred provider organization (PPO)#N#In a Medicare PPO plan, you may or may not use a primary care physician, and you are typically not required to get a referral to see a specialist. You’ll have a network of providers from which to choose .You will generally can receive at least some coverage when receiving care outside of the network of providers, though your health care services may cost more than if you received them from a provider within your plan network. 3 Point of service (POS)#N#You can use a primary care physician in a Point of Service plan, as you would with an HMO plan. But as with a PPO plan, you can go outside of the plan network and still receive some coverage for services, though you may pay higher out-of-pocket costs than if you selected an in-network provider.
How to contact Medicare Advantage?
For more information about managed care plans or other types of Medicare Advantage plans, including plan benefits, eligibility, enrollment and availability, contact a licensed insurance agent by calling. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 24 hours a day, 7 days a week.
Why do you see a primary care physician?
Seeing a primary care physician allows patients to build a rapport with their doctor, and the doctor gets to know the patient’s health history firsthand . When a patient is referred to a specialist, there is communication between the primary care physician and the specialist regarding the patient’s health and treatment.
Can you use a primary care physician in a point of service plan?
But as with a PPO plan, you can go outside of the plan network and still receive some coverage for services, though you may pay higher out-of-pocket costs than if you selected an in-network provider.
Is an indemnity plan a managed care plan?
Indemnity plans were popular before the advent of modern managed care plans, but they have been largely replaced by managed care plans over the last few decades, and the vast majority of privately insured Americans are in some form of managed care plan.
Is managed care part of Medicare?
Even in the Medicaid and Medicare systems, managed care is playing an increasingly large role: More than two-thirds of the people enrolled in Medicaid were covered under private Medicaid managed care plans as of 2017.
How does managed care work?
The primary way in which managed care plans work is by establishing provider networks. A provider network serves plan members over a certain geographic area in which the health plan is available. The providers in these networks agree to offer their services at reduced costs. Your health plan pays more of the cost of your care if you see providers ...
What is managed care organization?
A managed care organization or MCO is a health care company or a health plan that is focused on managed care as a model to limit costs, while keeping quality of care high.
What is HMO insurance?
Health Maintenance Organization (HMO) manages care by requiring you to see network providers, usually for a much lower monthly premium. HMOs also often require you to see a PCP before going elsewhere, and do not cover you to see providers outside the network. Preventive care is covered at 100%.
What is no cost preventive care?
No-cost preventive care is a big incentive for plan members to try and maintain good health. Primary Care Providers (PCP): Your health plan may require you to choose a PCP if you don’t already have one. You may be required to see your PCP first before going to any other doctor or specialist.
What is preventive care incentive?
Preventive care incentives: Managed care plans typically focus on making preventive care a priority. Most preventive services, such as annual check-ups, routine screenings, and certain vaccines, are covered at 100% by your health plan.
What are some examples of managed care?
They are examples of managed care: Provider networks: Health insurance companies contract with groups of providers to offer plan members reduced rates on care and services. These networks can include doctors, specialists, hospitals, labs, and other health care facilities. Some health plans require you to use the plan’s provider network ...
What is a prior authorization?
Prior authorization: Most managed care plans require you to get approval before you have certain types of procedures or treatments done, or are prescribed certain types of specialty medications. This is called prior authorization, precertification, or preapproval, depending on your insurer. Part of managed care’s goal is to help ensure you are not ...
Why is managed care important?
Managed care also helps control costs so you can save money .
What is Medicare Advantage?
Medicare Advantage (Part C) is personal insurance from private companies that’s approved by Medicare. Plan types that are available run the gamut — from HMO to PPO to POS — and include coverage for preventive healthcare, routine and major care, prescription drug coverage, even emergency coverage when traveling outside Nevada.
What is an HMO plan?
HMO: lower monthly premiums, comprehensive benefits. With an HMO plan, a primary care physician (PCP) typically must be selected. The PCP is responsible for coordinating all the members’ healthcare — a referral is often required before seeing a specialist or another physician.
What is the difference between a PPO and an HMO?
Like an HMO, PPO plans also have a network. The big difference is that members can go out of network for their healthcare — often without a referral — but they will pay more. Most of the time , monthly premiums are higher than an HMO.
