Full Answer
What is G0 modifier used for?
- Planned or Staged
- More extensive than original procedure
- For therapy following a surgical procedure.
What is a GA modifier for Medicare?
This GA modifier is to notify Medicare from provider that ABN is on file, and provider anticipates Medicare probably or certainly will not to cover those item or service. So by this provider indicates that patient has signed ABN form by appending GA modifier to CPT and patient will be responsible for the charges billed, if those items or service not covered by Medicare.
When to use G codes for Medicare?
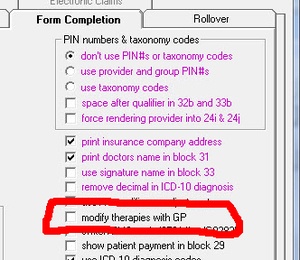
Here are the therapy discipline modifiers which must be on every claim line (including functional limitation reporting:
- Physical Therapist – signified by GP
- Occupational Therapist – signified by GO
- Speech-Language Pathologist – signified by GN (GN??)
What is gz modifier?
- Medicare will auto-deny services submitted with a GZ modifier
- The patient is not responsible for payment
- Medicare will not perform complex medical review on the service
- Medical will maintain the original denial on appeal without a request to remove the GZ
- On appeal, if requested to remove the GZ, all appropriate Medicare rules will apply

What is the GA modifier?
This GA modifier is to notify Medicare from provider that ABN is on file, and provider anticipates Medicare probably or certainly will not to cover those item or service. So by this provider indicates that patient has signed ABN form by appending GA modifier to CPT and patient will be responsible for the charges billed, if those items or service not covered by Medicare.
Why do you need to add GA modifier to CPT?
GA modifier should be append to a CPT, for which the provider had a patient sign an ABN form because there is a possibility the service may be denied because the patient’s diagnosis might not medically necessary. By this provider ensure upon Medicare denial, member will be liable to pay those services.
What is an ABN for Medicare?
ABN is also known as Waiver of Liability, signed by Medicare patients. In other way we can say a notice the hospital or doctor gives the patient before the treatment, telling the patient that Medicare may not pay for some treatment or services. This ABN document is signed by the patient, stating that, in case of Medicare is not going to pay, or not covering the payment, the patient himself is liable for the payment.
Can you use ABN modifiers on Medicare Advantage?
ABN modifiers are prohibited for Medicare advantage enrollees. As per CMS, dated on May 05, 2014 released that Advance Beneficiary notice modifiers i.e. GA, GX, GY or GZ to be used only for Medicare beneficiaries and not to be used for members of Medicare advantage plans.
Does Medicare cover CPT 15775?
CPT 15775 and 15776 performed for cosmetic reason will be denied as non-covered. Medicare does not cover cosmetic surgery codes that are performed to reshape or improve the beneficiary appearance.
What is a GY modifier?
GY – Item or service statutorily excluded or does not meet the definition of any Medicare benefit. GZ – Item or service expected to be denied as not reasonable and necessary. 2. Use of the GA, GY, and GZ Modifiers for Services Billed to Local Carriers. The GY modifier must be used when physicians, practitioners, ...
When did Medicare allow gy modifiers?
Beginning in January 2002, Medicare allowed providers and suppliers to use the GY modifier to indicate that a service or item is not covered by Medicare, either because it is statutorily excluded (e.g., hearing aids) or does not meet the definition of any Medicare benefit (e.g., surgical dressings that are used to clean or protect intact skin).9
When to use GZ modifier?
The GZ modifier must be used when physicians, practitioners, or suppliers want to indicate that they expect that Medicare will deny an item or service as not reasonable and necessary and they have not had an Advance Beneficiary Notification (ABN) signed by the beneficiary.
Can Medicare exclude home infusion?
These are statutorily excluded services. For services that Medicare does not allow, such as home infusion, providers need only file statutorily excluded services directly to their local plan using the GY modifier and will no longer have to submit to Medicare for consideration.
What is a GY modifier?
The definition is for GY is it is to be used for items or services that are statutorily excluded items or that do not meet the definition of any Medicare benefit.
Can a lab test be modified with a GY modifier?
The Medicare NCD Manual for Laboratory Tests lists the diagnosis that are considered screening and as such can be modified with the GY modifier in order to transfer the liability to the patient. Here is a link to the Manual.